Role of Vasopressin in Total Laparoscopic Hysterectomy-A Randomized Controlled Tria
- 1. Department of Endoscopy, Paul’s Hospital, Centre for Advanced Endoscopy &Infertility, India
ABSTRACT
Objective: To evaluate the use of intramyometrial vasopressin for reducing blood loss in total laparoscopic hysterectomy (TLH) in cases where the uterus is ≥ 12 weeks size.
Design: A randomized controlled trial was conducted at a tertiary care center over 2.5 years. A total of 110 participants were randomized into Group A (vasopressin), and group B (normal saline), with equal arms.
Materials and Methods: Group A and group B received intramyometrial injection of dilute vasopressin and normal saline, respectively. Estimated blood loss (EBL), and change in the postoperative hemoglobin were evaluated as primary outcomes. Bleeding from the pedicles and myoma spiral site were used to assess the role of vasopressin to maintain a clear surgical field.
Results: The median EBL was 200 mL in group A and 250 mL in group B, the difference not being statistically significant. The mean postoperative Hb was 10.7 g/dL in group A and 10.8g/dL in group B. The occurrence of bleeding at the pedicles was comparable in both groups. There was no bleeding at the myoma spiral site in 89% of patients in the vasopressin group compared to 45% in the control group, and this difference is significant.
Conclusion: There was no significant difference in the blood loss with the use of vasopressin in TLH for a uterine size of > 12 weeks compared to normal saline. Vasopressin helps reduce bleeding from the myoma spiral site used for uterine manipulation.
KEYWORDS
- Vasopressin
- Blood loss in laparoscopic hysterectomy
- Myoma spiral
- Large uteri
CITATION
Paul PG, Shilotri M, Chowdary AK, Degapudi M, Paul G, et al. (2022) Role of Vasopressin in Total Laparoscopic Hysterectomy - A Randomized Controlled Trial. Med J Obstet Gynecol 10(1): 1156.
DISCUSSION
Laparoscopic hysterectomy is the preferred method where an abdominal route is indicated for hysterectomy [15]. Blood loss during laparoscopic hysterectomy is on an average < 230 mL in large uteri [16]. But the blood loss further increases with the duration and the complexity of hysterectomy, especially when the uterus is enlarged [2].There are a few studies on the use of intramyometrial vasopressin during hysterectomy. However, there are no studies on its use in TLH. To our knowledge, this is the first RCT on the use of intramyometrial vasopressin during TLH to reduce bleeding with normal saline as the control group. This study found no difference in the blood loss during TLH for uteri > 12 weeks size between the intramyometrial vasopressin and normal saline groups. Myoma spiral site bleeding, which was used to manipulate the uterus, was significantly lesser in the vasopressin group.
Vasopressin has been shown to reduce blood loss in many gynecological surgeries and is used very commonly [7-10]. It is secreted by the posterior pituitary and mediated via 3 distinct receptors. The V1 receptor is located throughout the vascular tree, but primarily on the capillaries, small arterioles and venules, and smooth muscle throughout the body, including the myometrium [5].The vasoconstrictive effect and increased myometrial contractility may contribute to the effectiveness of vasopressin as a hemostatic agent in gynecologic surgery. 1 study has shown blood flow to the uterine artery is markedly reduced for 20 minutes [17].
We selected 100 mL of diluted vasopressin (20 U in 200 mL saline), equivalent to 10 U, a safe quantity used in many studies [5]. We preferred to use a larger volume as there is a lesser chance of an accidental intravascular large bolus that can precipitate side effects. A larger volume also allows for some loss of the medication during intramyometrial injection without reducing its effect. We used a similar volume of normal saline as a control so that the tourniquet effect of the fluid would be balanced in both groups.
The site and timing of vasopressin administration also vary in different studies. In the study on LSH by Ghomi et al., vasopressin (20 U in 50 mL saline) was injected into the myometrium after coagulating the uterine pedicles and just before amputating the uterine corpus from the cervix [12]. In the study by Chan et al. vasopressin (5 U in 40 mL saline) was injected in the submucosa circumferentially around the cervix before commencing the vaginal part of the LAVH [11]. In the study describing the use of vasopressin in total abdominal hysterectomy (TAH) by Okin et al., 10 U of vasopressin was injected bilaterally, 1 cm medial to the uterine vessels at the most distal area of the lower uterine segment [9]. In our study, 10 U of vasopressin was injected at the fundus and before beginning the hysterectomy, with the aim of preventing bleeding from the myoma spiral site, pedicles, and during adhesiolysis.
Several methods are used to estimate blood loss during laparoscopic surgery, and all of them are far from perfect. In our study, we estimated blood loss by measuring the suctioned blood and subtracting the fluid volume irrigated. The mean blood loss was 200 mL in the vasopressin group and 250 mL in the control group; however, this difference was not statistically significant. The change in Hb after surgery was also used as an additional parameter. The postoperative Hb was not significantly different between both the groups (10.7 vs. 10.8 g%). This observation is comparable to the studies on LAVH and LSH [11,12]. In contrast, in the studies on the use of vasopressin in TAH and VH, there was a definite reduction in the blood loss [9,10]. In the study on vasopressin in TAH, the reduction in blood loss averaged 280 mL, which was 40 % lesser than that in the placebo group [9]. However, there was no significant difference in the postoperative Hb, which they have not explained. Ascher-Walsh et al. also demonstrated a significant reduction in blood loss of 121 mL with the use of vasopressin in VH, while the change in Hb was not assessed [10].
In this study, we additionally tried to determine whether the use of vasopressin during TLH maintains a clean surgical field and reduces the additional use of suction and coagulation of the surgical site bleeding during dissection. We found that moderate and severe bleeding from the myoma spiral site was significantly lesser in the vasopressin group. The myoma spiral is a beneficial instrument for manipulating an enlarged and distorted uterus and aids optimal visualization of pedicles. The uterine manipulator alone is not effective in such a situation. The myoma spiral site can bleed profusely and obscure the surgical field when changing from 1 port to another. Thus, the use of vasopressin can definitely help to reduce this bleeding. We could not find this observation in any other studies. There was no difference in the bleeding during adhesiolysis in both the groups; however, the number of cases requiring adhesiolysis was less to draw a conclusion.
The total duration of surgery was significantly longer in the vasopressin group compared to the control group (141.1 vs. 123.9 minutes). In comparison, the total operating time did not differ between the vasopressin and control groups in the studies on TAH, VH, LAVH, and LSH [9-12].This discrepancy can be explained by the larger uterus size in the vasopressin group (580 g vs. 480 g), although this difference is not statistically significant. Since the time to reach the uterine pedicles was similar in both the groups, the total operating time was more in the vasopressin group due to the longer time taken for specimen retrieval. However, we did not objectively note the time taken for specimen retrieval as the study was not so planned.
There was a transient rise in systolic BP after the injection of vasopressin. A similar effect was noted in the studies where vasopressin was used in TAH and VH [9,10]. The main concern about the use of vasopressin is the serious cardiac complications. The potential complications are cardiac arrest, myocardial infarction, cardiogenic shock, arrhythmias, pulmonary edema, and life-threatening hypotension.5 There were no such complications in our group. The absence of complications in our study may be explained by the limited number of participants and a low quoted incidence of these complications in other studies. We also used a safe dose of 10 U of vasopressin diluted in a large volume which may have provided a margin of safety.
There were no cases of postoperative infections, cuff cellulitis, or readmissions in our study. An older study showed higher rates of cuff cellulitis with the use of epinephrine in vaginal hysterectomy and attributed it to its vasoconstricting action [18]. But an RCT conducted later did not substantiate this finding [19].
The limitation of our study is the estimation of intraoperative blood loss. In laparoscopic surgery, blood gets collected in the subdiaphragmatic space and the paracolic gutters where it is not possible to suction satisfactorily. The use of irrigation fluid for achieving hemostasis also makes the measurement inaccurate. Postoperative Hb measurement done after 18 hours can be inconsistent as the Hb tends to vary with time and the amount of fluid infusion given during and after surgery.
The strength of our study is that it is an RCT, and the surgeries were performed by a single experienced surgeon in the same institution using a standard technique.
As vasopressin has proven useful in reducing blood loss during TAH and VH, further studies may be needed with a larger sample population to demonstrate its utility in TLH. Alternate methods for reducing blood loss in TLH, especially in cases with large uteri, endometriosis or adhesions, are worth exploring.
ABBREVIATIONS
SD: Standard Deviation; LSCS: Lower-Segment Caesarean Section; TLH: Total Laparoscopic Hysterectomy; RCT: Randomized Controlled Trial; VH: Vaginal Hysterectomy; Hb: Haemoglobin; LAVH: Laparoscopic Assisted Vaginal Hysterectomy; LSH: Laparoscopic Supracervical Hysterectomy; TAH: Total Abdominal Hysterectomy; EBL: Estimated Blood Loss; IQR: Interquartile Range; SNOSE: Serially Numbered Opaque Sealed Envelope
RESULTS
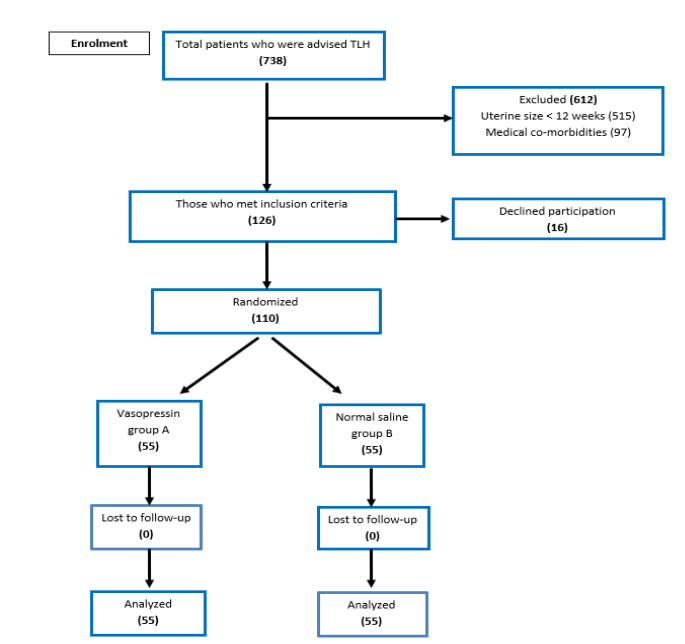
During the study period, the total number of patients who were advised TLH was 738, as shown in Figure 1. Of this, 515 patients were excluded due to a uterine size of < 12 weeks, while 97 patients were excluded due to concomitant medical disorders as described in the exclusion criteria. 16 patients declined to participate in the study. 110 patients who satisfied both the inclusion and exclusion criteria were randomized into 2 groups: group A (vasopressin) and group B (normal saline), containing 55 patients each.
Figure 1 CONSORT Diagram showing the flow of patients in the study.
Sociodemographic and preoperative characteristics of the study groups (Table 1)
|
Table 1: Sociodemographic and preoperative characteristics (N=110). |
||||||
|
|
|
Vasopressin |
Normal saline |
|
||
|
|
|
N = 55 |
N = 55 |
p value |
||
|
|
n |
% |
n |
% |
||
|
A |
Sociodemographic Characteristics |
|||||
|
1 |
Mean (SD) Age, in years |
45.2 (4.7) |
|
46.3 (4.5) |
|
0.208 |
|
2 |
Previous Surgery |
|||||
|
|
No |
20 |
36.4 |
23 |
41.8 |
0.558 |
|
Yes |
35 |
63.6 |
32 |
58.2 |
||
|
3 |
Previous LSCS |
|||||
|
|
No |
36 |
65.4 |
34 |
61.8 |
0.887 |
|
Yes |
19 |
34.6 |
21 |
38.2 |
||
|
B |
Details of surgery |
|||||
|
1 |
Indication of TLH |
|||||
|
|
Myomas |
47 |
85.4 |
44 |
80 |
0.199 |
|
Adenomyosis |
3 |
5.5 |
8 |
14.6 |
||
|
Endometriosis |
5 |
9.1 |
2 |
3.6 |
||
|
Others (ovarian cysts, endometrial hyperplasia) |
0 |
0 |
1 |
1.8 |
||
|
2 |
Additional procedure |
|||||
|
|
No |
22 |
40 |
25 |
45.4 |
0.563 |
|
Yes |
33 |
60 |
30 |
54.5 |
||
|
3 |
Endometriosis |
|||||
|
|
Absent |
44 |
80 |
47 |
85.4 |
0.449 |
|
Present |
11 |
20 |
8 |
14.5 |
||
|
4 |
Severity of Endometriosis |
|||||
|
|
Minimal/Mild |
1 |
9.1 |
2 |
25 |
0.302 |
|
Moderate |
2 |
18.2 |
3 |
37.5 |
||
|
Severe |
8 |
72.7 |
3 |
37.5 |
||
|
5 |
Uterus Size (SD), in weeks |
15 (2.6) |
|
14.5 (2.4) |
|
0.288 |
|
6 |
Preoperative haemoglobin, in g/dL |
11.9 (1.3) |
|
11.7 (1.1) |
1.1 |
0.379 |
|
SD: Standard deviation. LSCS: Lower-segment caesarean section. TLH: Total laparoscopic hysterectomy. |
||||||
The mean (SD) age of the participants in group A and group B was 45.2 (4.7) years and 46.3 (4.5) years, respectively, and is comparable in both groups. The number of patients who previously underwent any abdominal surgeries was 35 (64%) in group A vs. 32 (58%) in group B. The number of women who underwent cesarean sections was similar in both the study groups (group A: 19 (35%) vs. group B: 21 (38%). All the participants underwent TLH for benign conditions such as myoma uterus, adenomyosis, endometriosis, or additional pathologies like ovarian cysts and endometrial hyperplasia. The distribution of indications for hysterectomy in both groups was comparable. A similarly proportionate number of women underwent additional surgical procedures in both the groups, i.e. 33 in group A (60%) vs. 30 in group B (54. 5%). The overall number of patients who underwent hysterectomy with endometriosis was equivalent in both groups. Both the study groups were similar in terms of the size of the uterus in weeks. The mean preoperative Hb level in group A is 11.9 (1.3) g/dL and 11.7 (1.1) g/dL in group B and was comparable in both the study groups.
Operative and postoperative characteristics of the study groups (Table 2)
|
Table 2: Operative and postoperative characteristics. |
||||||
|
|
|
Vasopressin |
Normal saline |
|
||
|
|
|
Mean |
SD |
Mean |
SD |
p value |
|
1 |
Change in blood pressure (BP), in mm Hg |
|
||||
|
a |
Preoperative systolic BP |
128.4 |
14.4 |
128.9 |
15.5 |
0.848 |
|
b |
Preoperative diastolic BP |
86 |
10.5 |
84 |
11.5 |
0.342 |
|
c |
Postoperative systolic BP |
138 |
19.1 |
130.2 |
16 |
0.022 |
|
d |
Postoperative diastolic BP |
90 |
15 |
86.2 |
12.2 |
0.147 |
|
2 |
Suctioned blood, in mL |
200 |
150-400 |
250 |
150-400 |
0.729 |
|
3 |
Postoperative hemoglobin, in g/dL |
10.7 |
1.2 |
10.8 |
1 |
0.731 |
|
4 |
Duration of surgery, in minutes |
141.1 |
48.80 |
123.9 |
31.9 |
0.031 |
|
5 |
Time to reach uterine pedicles in minutes |
33 |
12.3 |
33.9 |
12.1 |
0.708 |
|
6 |
Number of intraoperative complications |
0 |
|
0 |
|
|
|
7 |
Number of Postoperative complications |
1 |
|
2 |
|
0.558 |
|
8 |
Duration of hospital stay |
1 |
0.10 |
1 |
0.2 |
0.5625 |
|
9 |
Weight of specimen, in grams |
580 |
350 -750 |
480 |
300 -800 |
0.471 |
|
SD:Standard deviation. |
||||||
.The mean (SD) systolic BP before injecting the drug was 128.4 (14.4) mmHg in group A and 128.9 (15.5) mmHg in group B. After the injection of the drug, we observed a rise in the systolic BP in group A with a mean value of 138 (19.1) mm Hg and this is significantly higher when compared to that in group B 130.2 (16) mm Hg. The diastolic BP was equivalent in both the groups before and after injecting the medication.
The median (IQR) EBL was 200 (150-400) mL in group A and 250 (150-400) mL in group B. Though the blood loss is more in the normal saline group, the difference is not statistically significant. The mean (SD) postoperative Hb was 10.7 (1.2) g/dL in group A and 10.8 (1) g/dL in group B, and there is no significant difference between the study groups. The mean total operative time in group A is 141 (48.8), minutes and 123.9 (31.9) in group B, this difference being statistically significant. The time to reach the uterine pedicle is 33.1 minutes in the vasopressin group (group A) and 33.9 minutes in the control group (group B). The uterine specimen weighed 580 g in the vasopressin group and 480 g in the normal saline group, the difference not being statistically significant. The mean duration of hospital stay was 1 day in both groups. 1 of the patients in the vasopressin group was transfused 1 unit of packed red cells preoperatively in view of anemia. None of the patients required intraoperative or postoperative blood transfusion. There were no intraoperative complications in either of the study groups. 1 patient in each group developed fever in the immediate postoperative period, which resolved with antibiotics. There was 1 case of urinary tract infection in the normal saline group.
The assessment of severity of bleeding at various steps during the TLH is described in Table 3. There was no bleeding at the myoma spiral site in 89% (49) patients in the vasopressin group compared to 45% (25) in the control group, and this difference was significant. The occurrence of bleeding and its severity at the pedicles was comparable in both groups; 25 (45.4%) in group A and 31 (56.3 %) in group B. There was no significant difference in bleeding during adhesiolysis in both groups.
|
Table 3: Assessment of severity of bleeding during TLH. |
||||||
|
|
|
n |
% |
n |
% |
p value |
|
1 |
Myoma spiral site bleeding |
|||||
|
|
No |
49 |
89.1 |
25 |
45.4 |
|
|
Moderate bleeding |
5 |
9.1 |
23 |
41.8 |
<0.001 |
|
|
Severe bleeding |
1 |
1.8 |
7 |
12.7 |
0.06 |
|
|
2 |
Pedicle Bleeding |
|||||
|
|
No |
30 |
54.5 |
24 |
43.6 |
0.421 |
|
Moderate bleeding |
19 |
34.6 |
25 |
45.5 |
||
|
Severe bleeding |
6 |
10.9 |
6 |
10.9 |
||
|
3 |
Adhesiolysis |
|||||
|
|
No |
7 |
77.80 |
3 |
60 |
0.58 |
|
Yes |
2 |
22.20 |
2 |
40 |
||
|
Moderate bleeding |
1 |
50.00 |
2 |
100 |
|
|
|
Severe Bleeding |
1 |
50.00 |
0 |
0 |
|
|
INTRODUCTION
Hysterectomy is the most common major gynecological surgery performed worldwide [1]. Common indications for total laparoscopic hysterectomy (TLH), are leiomyoma, adenomyosis, endometrial hyperplasia, endometriosis, and abnormal uterine bleeding refractory to medical management. Conditions like large uteri, pelvic adhesions, and endometriosis are associated with increased blood loss during TLH [2]. Some of the patients may already be anemic due to heavy menstrual bleeding. It has always been a challenge for gynecologists to reduce blood loss in these situations, and several interventions have been suggested. They include ligation of the uterine artery at the origin before proceeding with the hysterectomy and intraoperative use of vessel-sealing bipolar instruments or ultrasonic devices. Perioperative use of misoprostol, oxytocin, and vasopressin has also been studied [3-5].
Vasopressin has been used in gynecologic surgery for reducing blood loss since the1950s [6].There are many studies supporting the intraoperative administration of vasopressin to minimize blood loss in abdominal and laparoscopic myomectomy as well as in abdominal and vaginal hysterectomy (VH) [7-10]. The studies on laparoscopy-assisted vaginal hysterectomy (LAVH) and laparoscopic supracervical hysterectomy (LSH), using vasopressin for reducing blood loss concluded that the routine use of intramyometrial vasopressin does not reduce blood loss [11,12]. But, to our knowledge, there are no studies on its use in TLH. We thus planned to undertake a randomized controlled trial (RCT), to assess the role of vasopressin in TLH.
The primary aim of our study was to compare the blood loss during TLH with the use of dilute vasopressin versus normal saline in cases where the uterus is ≥ 12 weeks size, with or without endometriosis or adhesions. Intramyometrial vasopressin gives blanching of the uterus, and there is less likelihood of bleeding during dissection. If the surgical field is clear without bleeding, there are fewer instrument changes for suction and coagulation, which can reduce the strain on the surgeon. Lesser the additional steps required to achieve hemostasis, faster is the progress to the uterine pedicles. Thus, the secondary aims were to determine the role of vasopressin in maintaining a clear surgical field, the time taken to reach the uterine pedicles, and the intraoperative/ postoperative complications associated with its use.
MATERIALS AND METHODS
This RCT was conducted at Paul’s Hospital, a tertiary care center, over 2.5 years from October 2017 to April 2020. The study was approved by the institutional review board (Institutional Ethics Committee, Paul’s Hospital, Kochi, Kerala, India approval number IEC-PH-2017-GYN-002 dated 30th September 2017). All women scheduled for elective TLH with or without salpingo- oophorectomy were identified as possible participants for this study.
As there were no RCTs in estimating the mean blood loss in TLH, the sample size for the study was determined using total blood loss as the primary outcome variable as in a study conducted by Asher-Walsh et al., in VH [10]. The mean blood loss in a VH with and without the use of vasopressin was 144 mL and 266 mL, respectively, as observed in this study. With a confidence level of 95% and power of 80%, a sample size of 41 participants in each arm was derived. We recruited 55 participants in each arm to compensate for any dropouts during the study.
Women above 35 years of age with benign gynecological conditions and the uterus enlarged to > 12 weeks size were included in the study. Women with a history of cardiovascular diseases like coronary artery disease, myocardial infarction, cardiomyopathy, uncontrolled hypertension and other conditions like neurological disorders, migraine, asthma, chronic obstructive pulmonary disease, abnormal renal and liver function, any suspected bleeding or coagulation disorders, and history of allergy to vasopressin were excluded from the study. Informed consent was obtained from all the patients who satisfied the inclusion and exclusion criteria. Preoperative assessment was done on an outpatient basis within 7 days of the surgery. Demographic data and clinical history of the patients were recorded. The patients were divided into 2 groups; Group A constituted women who received dilute vasopressin, while Group B constituted women who received normal saline. Serially Numbered Opaque Sealed Envelopes (SNOSE) were created using random number table in Microsoft Excel. Randomization was done at the participant level by the circulating nurse. The nurse would open the envelope in the pre-operative room and would allocate the patient to the right arm. The surgeon and operative staff could not be blinded due to the difficulty in concealing the blanching effect of vasopressin on the uterus.
Operative procedure
General anesthesia was administered in all cases. No other drugs that would affect the circulatory system were administered during surgery. All patients received a prophylactic dose of an antibiotic before surgery. Intermittent pneumatic compression was used as prophylaxis for deep vein thrombosis.
The TLH was performed by a standard 4-port technique described earlier and was uniformly followed in all the cases [13,14].The patient was in Trendelenburg position at an incline of 20 degrees, and intra-abdominal pressure was set at 15 mmHg. Pneumoperitoneum was created by inserting a Veress needle at the umbilicus or Palmer’s point. A 10 mm primary camera port was inserted 3-4 cm above the upper margin of the enlarged uterus. A visual entry technique for primary entry was performed if the patient had any previous laparotomies or if bowel adhesions were suspected. 3 working ports of 5 mm each (1 suprapubic and 2 lateral), were placed 3-4 cm above the line joining the anterior superior iliac spines. A 30-degree telescope was used for the surgery. After the initial inspection of the abdomen, a single intramyometrial injection of 100 mL of either dilute vasopressin solution (20 IU in 200 mL normal saline) or normal saline, using a laparoscopic injection needle, was administered. A myoma spiral was used midline near the fundus along with a manipulator for uterine manipulation in all the cases. Vessel-sealing devices or bipolar diathermy with an ultrasonic device were used for coagulation and division of the pedicles. Opportunistic salpingectomy was performed in all cases when the ovaries were preserved. The specimen was removed vaginally after morcellation with a cold knife. The vaginal cuff was closed vaginally with conventional delayed absorbable or laparoscopically with barbed sutures. Additional procedures, if any, such as cystectomy, pelvic floor repair, appendicectomy, or hernia repair were performed at this stage.
In addition to the routine intraoperative monitoring, the patient’s blood pressure (BP), was recorded at the time of injection and 10 minutes after injection to calculate the change in these parameters. The total suction canister fluid was measured, and estimated blood loss (EBL), during surgery was calculated as EBL = total suction canister fluid volume - irrigated fluid volume. Postoperative hemoglobin (Hb) was measured before discharging the patient (approximately 12-16 hours after surgery). Other parameters such as total operative time, intraoperative and postoperative complications were noted.
We assessed the severity of bleeding at the myoma spiral site, lateral pedicles, during bladder dissection, and adhesiolysis. The severity of bleeding was graded as moderate (controlled by coagulation), and severe bleeding (needs suctioning and coagulation). The time to reach the uterine pedicles was also noted. We did not assess bleeding from the tackling of uterine vessels onwards as the action of vasopressin is not expected to be effective after 20 minutes. This assessment was done by watching all the surgical videos by assistant gynecologists, who were not part of the operative procedures.
Patients were followed up 2-4 weeks after surgery. The data collected from the medical records included information such as age, history of any previous surgeries, indication for the present surgery, any additional procedures done with hysterectomy, the uterine size, uterine weight, presence of endometriosis, the intraoperative change in BP on injection of the drug, change in the postoperative Hb, perioperative blood transfusion, the length of hospital stay and complications such as postoperative fever, if any.
Statistical analysis
The data retrieved from the records was entered in Microsoft Excel. Continuous variables like age, BP, and Hb levels were summarized as mean with standard deviation (SD). Other independent variables such as clinical details of the participants like any history of previous surgery, indication of surgery, any
additional procedures undertaken, etc. were summarized as frequency with proportions. The independent variables were compared across the 2 study groups using unpaired t-test or Mann-Whitney U test (for continuous data) and Chi-square or Fisher’s exact test (for proportions).
EBL followed a non-normal distribution and hence was summarized as median with its interquartile range (IQR) and compared using Mann-Whitney U Test between the study groups. The duration of surgery and time to reach the uterine pedicles were summarized as mean with SD and compared using the unpaired t-test. Presence of bleeding from the pedicles and myoma spiral site was summarized as proportions and compared between the 2 groups using the Chi-square test. Analysis was performed using Stata version 14.0 developed by StataCorp, 2015. A p-value less than 0.05 was considered significant throughout the study.
ACKNOWLEDGEMENTS
We thank Dr. Sharan Murali, Consultant (Medical), India EIS Training Programme, NIE - ICMR, Chennai for his invaluable help with the statistical analysis.
CONCLUSION
Our RCT on the use of vasopressin in TLH for a uterine size of >12 weeks did not find any significant difference in the blood loss compared to normal saline. There were no untoward events with the use of dilute vasopressin in this study. Vasopressin helps reduce bleeding from the myoma spiral site used for uterine manipulation during TLH.
REFERENCES
- Hammer A, Rositch AF, Kahlert J, Gravitt PE, Blaakaer J, Søgaard M. Global epidemiology of hysterectomy: possible impact on gynecological cancer rates. Am J Obstet Gynecol. 2015; 213: 23-29.
- Maclaran K, Agarwal N, Odejinmi F. Perioperative outcomes in laparoscopic hysterectomy: identifying surgical risk factors. Gynecol Surg. 2016; 13: 75-82.
- Biswas J, Chaudhuri P, Mandal A, Bandyopadhyay SN, Dasgupta S, Pal A. Effect of a single preoperative dose of sublingual misoprostol on intraoperative blood loss during total abdominal hysterectomy. Int J Gynaecol Obstet. 2013; 122: 244-247.
- Wang CJ, Yuen LT, Yen CF, Lee CL, Soong YK. A simplified method to decrease operative blood loss in laparoscopic-assisted vaginal hysterectomy for the large uterus. J Am Assoc Gynecol Laparosc. 2004; 11: 370-373.
- Chudnoff S, Glazer S, Levie M. Review of vasopressin use in gynecologic surgery. J Minim Invasive Gynecol. 2012; 19: 422-433.
- Dillon TF. Vasopressin as a hemostatic in gynecologic surgery. Am J Obstet Gynecol. 1959; 78: 1285-1291.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev. 2014; CD005355.
- Soliman R, Yacoub A, Elbiaa AAM. Assessment of the perioperative effect of vasopressin in patients undergoing laparoscopic myomectomy: A double-blind randomised study. Indian J Anaesth. 2021; 65: 139-145.
- Okin CR, Guido RS, Meyn LA, Ramanathan S. Vasopressin during abdominal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2001; 97: 867-872.
- Ascher-Walsh CJ, Capes T, Smith J, Michels A. Cervical vasopressin compared with no premedication and blood loss during vaginal hysterectomy: a randomized controlled trial. Obstet Gynecol. 2009; 113: 313-318.
- Chan C, Yu M, Hwang K, Wu G, Liu J, Chu T. Can Vasopressin decrease the blood loss in laparoscopic assisted vaginal hysterectomy? A randomized study. J Med Sci. 2003; 23: 281-283.
- Ghomi A, Makhlouf F, Kasturi S, Einarsson JI. Intramyometrial injection of vasopressin in laparoscopic supracervical hysterectomy. J Minim Invasive Gynecol. 2008; 15: 197-201.
- Paul PG, Mannur S, Shintre H, Paul G, Gulati G, Mehta S. Thirteen Years of Experience with Opportunistic Bilateral Salpingectomy During TLH in Low-Risk Premenopausal Women. J Obstet Gynaecol India. 2018; 68: 314-319.
- Paul PG, Prathap T, Kaur H, Shabnam K, Kandhari D, Chopade G. Secondary hemorrhage after total laparoscopic hysterectomy. JSLS. 2014; 18: e2014.00139.
- Royal College of Obstetricians and Gynaecologists/ The British Society for Gynaecological Endoscopy. Management of Endometrial Hyperplasia. London: RCOG; 2016. (Green-top Guideline No. 67).
- Sinha R, Sundaram M, Lakhotia S, Mahajan C, Manaktala G, Shah P. Total laparoscopic hysterectomy for large uterus. J Gynecol Endosc Surg. 2009; 1: 34-39.
- Takeuchi H, Shimanuki H, Kobori H, Kitade M, Kikuchi I, Kinoshita K. Effect of vasopressin on blood flow and RI of the uterine artery during laparoscopic myomectomy. J Minim Invasive Gynecol. 2005; 12: 10-11.
- England GT, Randall HW, Graves WL. Impairment of tissue defenses by vasoconstrictors in vaginal hysterectomies. Obstet Gynecol. 1983; 61: 271-274.
- Kammerer-Doak DN, Rogers RG, Johnson Maybach J, Traynor Mickelson M. Vasopressin as an etiologic factor for infection in gynecologic surgery: a randomized double-blind placebo-controlled trial. Am J Obstet Gynecol. 2001; 185: 1344-1347.