Silent Intruders How Ureaplasma and Mycoplasma Shape Pregnancy Outcomes (Prospective Study in Kosovo)
- 1. Gynegologist- Obstetrician, Regional Hospital “Dr. Daut Mustafa” Prizren – Kosovo
- 2. Anesthesiology and Intensive Care Resident, Regional Hospital “Dr. Daut Mustafa” Prizren – Kosovo
Abstract
Ureaplasma and Mycoplasma are atypical microorganisms classified as intracellular bacteria. Their ability to survive and replicate within host cells enables them to evade immune responses. These microorganisms are associated with urogenital tract infections, which can contribute to complications during pregnancy, including preterm labor. Often underestimated, these infections require thorough evaluation for effective pregnancy management. This prospective study was conducted at the University Clinical Center of Kosovo in 2024 and involved 7654 births, of which 819 were preterm. Patients were diagnosed with Ureaplasma and Mycoplasma infections through culture methods and PCR. The distribution of infections was analyzed based on previous abortions, WBC and CRP levels in mothers and newborns, newborn weight, and the stages of preterm birth categorized by gestational days. The aim of this study was to evaluate the impact of these microorganisms on preterm labor and birth outcomes. Among the participants, 73 pregnant women tested positive for these bacteria; for comparison, 73 women who tested negative were selected to assess differences in preterm birth and pregnancy outcomes.
Keywords
• Preterm birth
• Bacterial infection
• Mycoplasma
• Ureaplasma
• WBC levels
• CRP levels
• Previous abortion
• Birth weight
• Pregnancy duration
Citation
Sinani F, Birdaini S (2025) Silent Intruders: How Ureaplasma and Mycoplasma Shape Pregnancy Outcomes (Prospective Study in Kosovo). Med J Obstet Gynecol 13(2): 1198.
INTRODUCTION
According to the World Health Organization (WHO), preterm birth is defined as the expulsion or complete removal of the products of conception from the mother’s body with a weight of at least 500 grams. If the weight is unknown, a gestational age of 20 weeks or a length of at least 25 centimeters at birth is considered [1-4]. Thus, preterm birth includes any delivery occurring after the 20th–22nd week of pregnancy, with a fetal weight exceeding 500 grams, but before the completion of the 37th week, with signs of breathing at birth. Preterm newborns continue to face high mortality rates due to inadequate neonatal care, particularly in low-and middle-income countries [5]. Preterm birth remains a leading cause of infant mortality and morbidity. While the main causes of preterm labor are not fully understood, it is believed to be a multifactorial and complex process [6]. Microbial infections involving the placenta, amniotic fluid, vaginal canal, and even the oral cavity are recognized as significant contributors to preterm birth [7].
Witt et al., detected Ureaplasma spp. and Mycoplasma spp. in cases of suspected chorioamnionitis by analyzing maternal and umbilical cord samples [8]. Similarly, Jang et al., reported a 26.5% positive culture rate for Ureaplasma among pregnant women admitted with preterm labor; however, no cases of Mycoplasma hominis were identified [9].
Genital Mycoplasma can ascend from the vagina through the cervix into the uterus and amniotic sac, leading to intrauterine infections, particularly during the second trimester. Intrauterine infections are responsible for preterm labor in approximately 40% of cases, largely due to the maternal immune response. Bacterial surface antigens, known as pathogen-associated molecular patterns (PAMPs), are detected by Toll-like receptors (TLRs) on innate immune cells, triggering activation of macrophages and monocytes. This immune reaction increases the production of inflammatory cytokines and chemokines, such as IL-1, IL-6, IL-8, and TNF-α, which subsequently stimulate the release of metalloproteinases and prostaglandins, ultimately leading to preterm labor [10,11]. This study aimed to determine the role of genital Mycoplasma in preterm labor by examining and comparing the frequency of four species of genital Mycoplasma among pregnant women experiencing preterm labor.
MATERIALS
Our research employed a prospective monitoring approach, tracking pregnant women from their initial presentation at the clinic through to delivery. This method enabled direct assessment of the risk factors associated with disease development. The study included 146 pregnant women with gestational ages ranging from 28 weeks and 0 days to 36 weeks and 6 days. Gestational age was calculated based on the first day of the last menstrual period and confirmed by the initial ultrasound examination.
Type of Study
This is a descriptive, prospective cohort study. A cohort design was selected due to its effectiveness in simultaneously describing the distribution of exposure and health outcomes within a population. This design is particularly appropriate for investigating common conditions such as Mycoplasma hominis and Ureaplasma urealyticum, given their high prevalence.
Study Period
The study was conducted between January 1, 2024, and December 31, 2024.
Study Institution
The research was carried out at the Obstetrics and Gynecology Clinic of the University Clinical Center of Kosovo, the only tertiary healthcare facility in Kosovo.
Informed Consent
All participants were informed about the procedures necessary for completing standardized medical data forms and consented to undergo regular examinations. All procedures were conducted with strict confidentiality, and participation was entirely voluntary.
METHODOLOGY
The methodology applied to test the study hypotheses involved a comprehensive set of statistical techniques, including multiple linear regression, descriptive statistics, frequency analyses, cross-tabulations, chi square tests, correlations, and additional data analysis methods. This combination provided a robust and precise framework for understanding the relationships and effects between dependent and independent variables. Multiple linear regression was utilized to evaluate the linear associations between the dependent variable and one or more independent variables. Its application facilitated the identification and measurement of the potential effects of independent variables on the integrating dependent variable, thus supporting hypothesis testing. By these statistical approaches, the methodology ensured a comprehensive understanding of the data structure and interrelationships, offering a solid foundation for making accurate and reliable evaluations of the tested hypotheses. The adopted methodology thereby guarantees a thorough and consistent analysis of the data.
RESULTS
During the one-year study period, 73 pregnant women who tested positive for Mycoplasma and Ureaplasma (study group) were identified, along with 73 pregnant women who tested negative for these bacteria (control group); all participants experienced preterm delivery.
Analysis of the data collected at the Clinic for Gynecology and Obstetrics at the University Clinical Center in Prishtina, from January 1, 2024, to December 31, 2024, revealed significant differences between the clinical presentations and laboratory findings of the study and control groups.
During the one-year study period, 73 pregnant women who tested positive for Mycoplasma and Ureaplasma (study group) were identified, along with 73 pregnant women who tested negative for these bacteria (control group); all participants experienced preterm delivery.
Analysis of the data collected at the Clinic for Gynecology and Obstetrics at the University Clinical Center in Prishtina, from January 1, 2024, to December 31, 2024, revealed significant differences between the clinical presentations and laboratory findings of the study and control groups. As the first parameter, previous miscarriages were considered. The distribution of previous miscarriages was relatively balanced between the groups; however, a notable distinction emerged: among bacteria negative mothers, none had experienced more than three miscarriages, whereas among bacteria-positive mothers, five had a history of more than three miscarriages (Figure 1).
Figure 1 Previous abortion (Source: Author’s research).
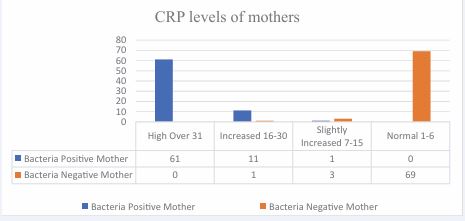
Regarding the laboratory findings, the C-reactive protein (CRP) levels in the study group were markedly elevated, with 61 cases recording CRP values above 31. In contrast, in the control group, 69 participants exhibited normal CRP levels, ranging between 1 and 6 (Figure 2).
Figure 2 CRP levels in mothers (Source: Author’s research).
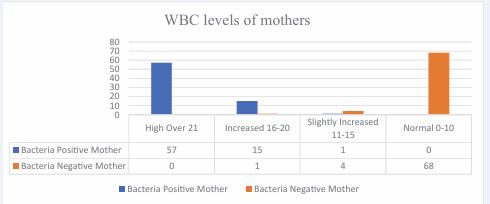
The leukocyte count among mothers in the study group was significantly elevated: 57 participants had values above 21, 15 had elevated levels ranging from 16 to 20, and one had a slightly elevated count between 11 and 15. Notably, none of the participants in the study group had normal leukocyte levels. In the control group, only one pregnant woman exhibited an elevated leukocyte count, four had slightly elevated values, and 68 had normal leukocyte counts (Figure 3).
Figure 3 Leukocyte count in mothers (Source: Author’s research).
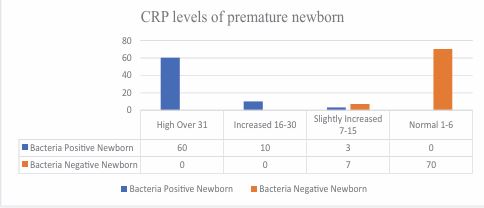
Regarding the serum CRP levels of premature infants in the study group, 60 babies exhibited high CRP levels, 10 had elevated levels, and 3 had slightly elevated values, while none had normal CRP levels. In contrast, in the control group, 70 babies had normal CRP levels, and 3 exhibited slightly elevated values (Figure 4).
Figure 4 CRP levels in premature infants (Source: Author’s research).
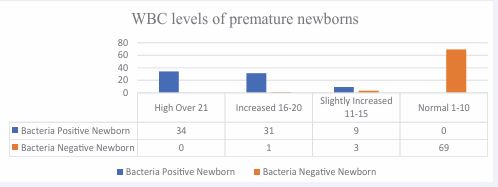
Regarding the leukocyte count in premature infants, babies born to mothers in the study group exhibited high leukocyte counts, whereas those in the control group demonstrated normal values (Figure 5).
Figure 5 Leukocyte count in premature infants (Source: Author’s research)
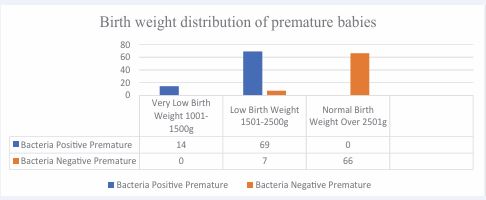
The next parameter analyzed was birth weight. In the study group, bacterial infections had a notable impact on birth weight, with 14 premature infants having very low birth weight (1001–1500g) and 69 having low birth weight (1501–2500g). In contrast, in the control group, 66 premature infants had a normal birth weight (above 2501g), while 7 had low birth weight (Figure 6).
Figure 6 Birth weight (Source: Author’s research).
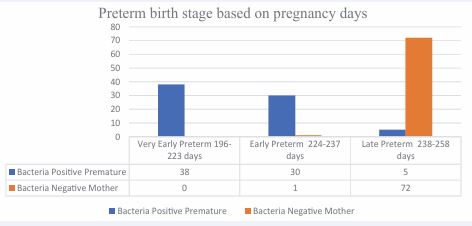
Regarding the timing of delivery, the study group had 38 babies born very early (196–223 days), 30 born early preterm (224–237 days), and only 5 born late preterm (238–258 days). In contrast, in the control group, only one baby was born early preterm, while the rest were late preterm (Figure 7).
Figure 7 Timing of Delivery (Source: Author’s research).
DISCUSSION
In recent years, intrauterine infections have increasingly been recognized as significant contributors to adverse pregnancy outcomes, including preterm birth, spontaneous abortion, and the delivery of infants with congenital anomalies. Our study contributes to the growing body of evidence supporting this association, with a particular emphasis on the ascending pathway of infection one of the most common routes by which pathogens invade the intrauterine environment. This ascending route involves the migration of microorganisms from the lower genital tract into the uterus, potentially leading to chorioamnionitis, premature rupture of membranes, and, ultimately, preterm labor.
Our findings support this mechanism, as we observed a strong correlation between the presence of bacterial pathogens in the cervical region and various negative obstetric outcomes, including shortened gestational age, reduced birth weight, and, in some cases, miscarriage. The clinical and laboratory findings in our study population were particularly noteworthy. Pregnant women who tested positive for bacterial infections exhibited more pronounced symptoms of vaginal discomfort, abnormal discharge, and inflammation, accompanied by laboratory evidence of elevated inflammatory markers. These changes reflect an active infectious process that, if left untreated, may progress and compromise both maternal and fetal health.
In comparison to previous research, our study confirms the conclusions drawn by multiple authors that chronic vaginal and cervical infections are major risk factors for early pregnancy loss. However, our findings also emphasize that the presence of subclinical infections—those without overt symptoms—can be equally dangerous, underscoring the need for routine screening even in asymptomatic patients.
Early detection plays a pivotal role in mitigating the risks associated with these infections. Timely diagnosis facilitates the prompt initiation of antimicrobial therapy, which can significantly reduce the risk of intrauterine spread and prevent complications such as preterm labor. Our data suggest that frequent screening throughout pregnancy, particularly in high-risk populations, can lead to improved gestational outcomes and better neonatal health.
Ultimately, our study underscores the importance of integrating routine microbiological assessments into prenatal care. By identifying and treating infections early, we have the potential to reduce the incidence of preterm birth and its associated complications, improving both short- and long-term health outcomes for mothers and their infants.
CONCLUSION
This study highlights the significant impact of Ureaplasma and Mycoplasma infections on adverse pregnancy outcomes, particularly preterm birth. The findings demonstrate that women infected with these microorganisms show higher inflammatory markers, such as CRP and leukocyte counts, and have a greater likelihood of delivering infants with lower birth weight and earlier gestational age compared to uninfected women.
These results reinforce the hypothesis that ascending genital tract infections play a crucial role in triggering inflammatory responses that lead to premature labor. Early detection and treatment of Ureaplasma and Mycoplasma infections during pregnancy are therefore essential to improving neonatal outcomes and reducing the incidence of preterm delivery.
The implementation of routine microbiological screening in prenatal care should be considered a key preventive strategy. Through timely diagnosis and adequate antibiotic therapy, it is possible to mitigate infection-related complications, safeguard maternal health, and promote optimal fetal development.
REFERENCES
- Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. Lancet Glob Health. 2019; 7: e37-e46.
- Davidson KM. Detection of premature rupture of the membranes. Clin Obstet Gynecol. 1991; 34: 715-724.
- Gunn GC, Mishell DRJr, Morton DG. Premature rupture of the fetal membranes: A review. Am J Obstet Gynecol. 1970; 106: 469-475.
- Hannah ME, Hodnett ED, Willan A, the TermPROM Study Group. Prelabor rupture of the membranes at term: Expectant management at home or in hospital? Obstet Gynecol. 2000; 96: 533-538.
- Jang YS, Min JW, Kim YS. Positive culture rate and antimicrobial susceptibilities of Mycoplasma hominis and Ureaplasma urealyticum. Obstet Gynecol Sci. 2019; 62: 127-133.
- Moridi K, Hemmaty M, Azimian A, Fallah MH, Abyaneh HK, GhazviniK. Epidemiology of genital infections caused by Mycoplasma hominis,M. genitalium, and Ureaplasma urealyticum in Iran: A systematic review and meta-analysis study (2000–2019). BMC Public Health. 2020; 20: 1020.
- Muhe LM, McClure EM, Nigussie AK, Mekasha A, Worku B, Worku A, et al. Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): A prospective, cross-sectional, observational study. Lancet Glob Health. 2019; 7: e1130-e1138.
- Pavlidis I, Spiller OB, Demarco GS, MacPherson H, Howie SE, Norman JE, et al. Cervical epithelial damage promotes Ureaplasma parvum ascending infection, intrauterine inflammation, and preterm birth induction in mice. Nature Communications. 2019; 11: 199.
- Shubeck F, Benson RC, Clark WW. Jr.. Fetal hazard after rupture of the membranes: A report from the collaborative project. Obstet Gynecol. 1966; 28: 22-31
- Witt RG, Blair L, Frascoli M, Rosen MJ, Nguyen QH, Bercovici S, et al. Detection of microbial cell-free DNA in maternal and umbilical cord plasma in patients with chorioamnionitis using next generation sequencing. PLOS ONE. 2020; 15: e0231239.
- You YA, Yoo JY, Kwon EJ, Kim YJ. Blood microbial communities during pregnancy are associated with preterm birth. Front Microbiol. 10: 1122.