Clinical Profile and Predictors of Uncontrolled Arterial Hypertension in Hypertensive Obese Patients: Insights from the Tunisian Multicentric Observational Study NATURE HTN
- 1. Biophysics laboratory faculty of medicine of sousse, Tunisia
Abstract
Background: Obesity and arterial hypertension (AHT) are both significant cardiovascular risk factors, with obesity being a major contributor to the development of AHT. AHT in obese patients is particularly challenging to control due to the increased risk of target organ damage. Obesity has been identified as an independent predictor of uncontrolled AHT in Tunisian patients, as demonstrated by the national multicentric study on AHT (NATURE HTN). Therefore, we aimed to examine the profile of AHT in obese Tunisian adults recruited from the Tunisian registry NATURE HTN.
Methods: A total of 23601 hypertensive individuals were recruited from the national multicentric registry NATURE HTN. Participants were divided into groups based on whether they had controlled or uncontrolled AHT defined as an average of systolic blood pressure above 140 mmHg or an average of systolic blood pressure above 90mmHg AHT according to their body mass index (BMI).
Results: The profile of AHT in obese Tunisian adults was as follow: female predominance (69.47%), half was diabetic, 74.67% have a low educational level; renal and cardiac impact were present (24.82% of microalbuminuria, 14.47% of left ventricular hypertrophy on transthoracic echocardiography), and 15% were untreated. This profile classifies our population at high cardiovascular risk although. There is a linear association between severity of obesity and uncontrolled blood pressure (BP). In the subgroup of severe obesity, mellitus diabetes and heart rate were associated with uncontrolled AHT [odds-ratio and confidence interval: 1.09 [1.06-1.12]; 1.11 [1.07-1.15], respectively]. In multivariate analysis, diastolic blood pressure (DBP) and Heart rate (HR) were independently associated with obesity.
Conclusion: There was a strong association between severity of obesity and uncontrolled BP CF and DBP were independently associated with obesity. obese and hypertensive patients were also diabetic and had organ damage. Therefore, an urgent and targeted treatment strategy is necessary.
Keywords
• Hypertension
• Management
• Obesity
• Tunisia
Citation
Imen B (2025) Clinical Profile and Predictors of Uncontrolled Arterial Hypertension in Hypertensive Obese Patients: Insights from the Tunisian Multicentric Observational Study NATURE HTN. Ann Cardiovasc Dis 9(2): 1044.
ABBREVIATIONS
ABPM: Ambulatory Blood Pressure Measurment; ACE: Angiotensin–converting Enzyme; AHT: Arterial Hypertension; ARB: Angiotensin Renin Bloker; AUC: Area Under Curve; BMI: Body Mass Index; BP: Blood Pressure; CCB: Calcium Channel Bloker; CI: Confidence Intervals; DBP: Diastolic blood pressure; EKG: Electrocardiogram; ESC: European Society of Cardiology; ESH: European Society of Hypertension; HR: Heart Rate; LVH: Left Ventricular Hypertrophy; OR: Odds Ratio; SBPM: Self Blood Pressure Measurment; TTE: TransThoracic Echocardiography; US: Ultra Sound According to the World Health Organization (WHO), obesity contributes to 7.1% of all-cause deaths [1], and 4.9% of disabilities worldwide [2]. In the United States, for example, 35% of individuals with obesity have high blood pressure, compared to only 18% of individuals with normal weight [3]. Furthermore, the global economic burden of obesity is expected to exceed $4 trillion by 2035 [4]. In Tunisia, the situation is equally concerning. The prevalence of obesity continues to rise, accompanied by a high incidence of related diseases, including hypertension [5,6]. The Tunisian TAHINA project has identified obesity as a key predictor of the onset of AHT (adjusted odds ratio (aOR) = 2.83 (2.50-3.20) [7]. Additionally, the national multicenter NATURE HTN study confirmed that obesity is an independent predictor of uncontrolled AHT in Tunisian patients [8]. Obesity and hypertension together increase the strain on the ventricular wall, contributing to the development of heart failure with preserved ejection fraction (HFpEF). These conditions pose serious health risks for patients, and their management remains a significant challenge for healthcare systems Against this backdrop, the objectives of this study, based on the NATURE HTN registry, are to: i) describe the clinical profile of Tunisian hypertensive patients with obesity, and ii) evaluate the management and predictors of uncontrolled AHT within this specific subgroup.
INTRODUCTION
Obesity is a chronic condition characterized by excess body fat, typically measured using body mass index (BMI). A BMI greater than 30 kg/m² is classified as obesity. This condition has significant implications for public health, as it is a major risk factor for several diseases, including dyslipidemia, type 2 diabetes, cardiovascular disease, and hypertension (AHT). Globally, obesity has become a major public health crisis, affecting approximately 13% of the adult population and leading to severe consequences. According to the World Health Organization (WHO), obesity contributes to 7.1% of all-cause deaths [1], and 4.9% of disabilities worldwide [2]. In the United States, for example, 35% of individuals with obesity have high blood pressure, compared to only 18% of individuals with normal weight [3]. Furthermore, the global economic burden of obesity is expected to exceed $4 trillion by 2035 [4]. In Tunisia, the situation is equally concerning. The prevalence of obesity continues to rise, accompanied by a high incidence of related diseases, including hypertension [5,6]. The Tunisian TAHINA project has identified obesity as a key predictor of the onset of AHT (adjusted odds ratio (aOR) = 2.83 (2.50-3.20) [7]. Additionally, the national multicenter NATURE HTN study confirmed that obesity is an independent predictor of uncontrolled AHT in Tunisian patients [8]. Obesity and hypertension together increase the strain on the ventricular wall, contributing to the development of heart failure with preserved ejection fraction (HFpEF). These conditions pose serious health risks for patients, and their management remains a significant challenge for healthcare systems Against this backdrop, the objectives of this study, based on the NATURE HTN registry, are to: i) describe the clinical profile of Tunisian hypertensive patients with obesity, and ii) evaluate the management and predictors of uncontrolled AHT within this specific subgroup.
PATIENTS AND METHODS
Study design and ethical considerations
The NATURE HTN registry is an observational, multicenter national study conducted across all governorates of Tunisia involving both public and private health care sectors. The study protocol has been previously published [9]. Patients were enrolled between April 15, 2019, to and May 15, 2019, a period that included the month of Ramadan. The enrolment and clinical examinations were performed by a diverse team of investigators, including cardiologists, general practitioners, nephrologists, endocrinologists, and internists. The study included all patients with known or newly diagnosed hypertension (AHT) who consulted their doctors during the enrolment period. The study protocol and informed the consent form were reviewed and approved by a national ethics committee. Data were collected and managed using the Clinical Suite platform (Dacima Software), which complies with international standards including US Food and Drug Administration 21 Code of Federal Regulations Part 11, the US Health Insurance Portability and Accountability Act, International Conference on Harmonisation, and Medical Dictionary for Regulatory Activities. The Clinical Suite platform allowed us to track the entered data and to check for inconsistencies and missing data. A steering committee was established to oversee patient inclusions, verify data sources, ensure compliance with the study protocol and prepare statistical analysis plan. We confirm that all study procedures were conducted in accordance with relevant guidelines and regulations. All experimental protocols were approved by the ethic committee of the Hospital of the Internal Security Forces (Tunis,Tunisia). Written informed consent was obtained from all patients. In case of illiterate patients, informed consent was obtained from legal guardians.
Inclusion Criteria
During the office visits, we included patients who met the following criteria: a history of elevated blood pressure (BP) for at least six months .Age older than 18 years and written informed consent. For patients with newly diagnosed hypertension (AHT), the diagnosis was confirmed according to the European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines [10]. Diagnosis of new AHT was confirmed if either out-of-office BP measurement above the recommended thresholds or repeated office BP measurements on more than one visit above 140 mmHg for the systolic blood pressure (SBP) and /or 90 mmHg for the diastolic blood pressure (DBP).
Exclusion Criteria
We excluded the following patients from the final analysis: Patients undergoing hemodialysis, pregnant women, patients classified as having white coat hypertension, and patients who refused to sign the consent form.
Clinical evaluation and data collection during the office visit
During the office visit the physician had to complete the case report form collected socio-demographic information, including age, sex, education level (with low education level as illiteracy or a primary education) health insurance, smoking habits, and medical story such as diabetes mellitus, pulmonary diseases, hypothyroidism, moderate renal failure (defined by an Modification of Diet in Renal Disease (MDRD) creatinine clearance 35 mm) or an R wave in aVL ≥ 11 mm, as recommended by the ESC/ESH guidelines. Additionally, echocardiographic findings were reviewed for LVH if the patient had an echocardiogram within the last year before study inclusion. We also recorded the most recent laboratory tests, including creatinine (µmol/L), glycaemia (mmol/L), cholesterol (mmol/L), and potassium (kaliemia) (mmol/L), performed within the last six months prior to the office visit, along with microalbuminuria (mg/L) if tested within the past year. The office-based GLOBORISK cardiovascular disease risk score was calculated using age, sex, systolic blood pressure (SBP), current smoking status, and BMI. Based on the Tunisian clinical guidelines on AHT management, patients were categorized into four risk groups: low (<10%), moderate (10-19%), high (20 29%), and very high (≥30%), with the score not applicable for individuals under 40 years old [14,15]. The primary endpoint of our study was the rate of hypertension (AHT) control according to BMI value. Uncontrolled AHT was defined, following the ESC/ESH guidelines and Tunisian clinical practice guidelines, as an average SBP above 140 mmHg and/or an average diastolic blood pressure (DBP) above 90 mmHg [10-16].
Statistical Analysis
All statistical analyses were achieved using the SPSS 23.0 (SPSS, Chicago, IL, USA) statistical package. Continuous variables were presented as means value ± standard deviation in case of Gaussian distribution and as medians as well as extremes values in case of non-Gaussian distribution. We distinguished two groups according to the AHT control (controlled group versus uncontrolled group), and four groups according to corpulence status [normal BMI, moderate, morbid, and severe obesity]. The comparison between the four groups and the subgroup of uncontrolled AHT was achieved by Student’s t test and Chi2 test for continuous variables and categorical variables, respectively. Univariate logistic regression analyses were used to determine crude odds ratio (OR) with the 95% approximate confidence intervals (CI) as estimators of the uncontrolled AHT for various characteristics of the study population. To assess the predictors of uncontrolled BP, we performed a multivariate logistic regression model to identify independent predictors of uncontrolled AHT; Variables with a p-value < 0.10 in univariate analysis were included in the model. Multicollinearity was assessed prior to inclusion. The significance threshold was set at p < 0.05. The receiver operator characteristics analysis was used to compare the area under the curve (AUC) to determine the optimal cut-off BMI for uncontrolled AHT.
RESULTS
Sociodemographic characteristics of the population study
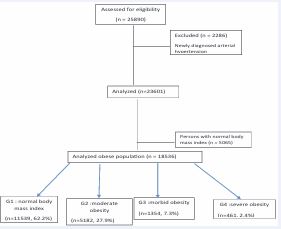
A total of 23601 individuals was enrolled in the present study: 6494 were obese and 15940 had a normal to overweight corpulence status. The obese hypertensive population was divided into four groups according to the BMI value, the proportions of moderate, morbid and severe obesity groups were 20.2%, 5.3%, and 1.8%, respectively (Figure 1).
Figure 1 Study flowchart. G1: Normal Body Mass Index. G2: Moderate Obesity. G3: Morbid Obesity. G4: Severe Obesity
The obese hypertensive population was younger than the non-obese (63.7 ± 11.3, p<0.001). Approximately 75% of patients were women. On the other hand, diabetes mellitus was very present in this population (46.9%, p<0.001), which seems to be more controlledthan non obese population and such patient phenotype tends to have more COPD, apnea syndrome, and hypothyroidism (1.9%, 4.4%, and 6.5%, respectively). Regarding BP control, this population had more ABPM and SMBP without effective BP control compared to non-obese hypertensive persons. The grade of AHT in this patient phenotype is higher than the non-obese, without more electrical or echocardiographic left ventricular hypertrophy. The frequent association between obesity and diabetes mellitus classified this population at high risk of cardiovascular morbidity and mortality at 10 years (Table 1).
Table 1: Sociodemographic, anthropometric behaviour factors, drugs of patients with obesity and arterial hypertension.
|
Data (unit) |
G1; N=11539 |
G2; N=5182 |
G3; N=1354 |
G4; N=461 |
p-value |
|
Mean age, (years) |
64.4 ± 12.1 |
63.4 ± 11.7 |
62.7 ±11.5 |
61.7 ± 10.7 |
<0.001 |
|
Sex (Female), n (%) |
5515,51.9% |
3285,67.7% |
995,77.0% |
355,81.3% |
<0.001 |
|
National Social Security (CNAM), n (%) |
7775,73.0% |
3406,70.6% |
979,75.0% |
346979.20% |
<0.001 |
|
Smoking, n (%) |
1610,15.4% |
450,9.8% |
75,6.1% |
20,4.8% |
<0.001 |
|
Diabetes mellitus, n (%) |
4326,60.7% |
2226,55.3% |
596,54.4% |
219,51.6% |
<0.001 |
|
Hypothyroidism |
581,5.4% |
283 ,5.9% |
94,7.2% |
42,9.3% |
<0.001 |
|
Apnea syndrome (yes) |
100,0.9% |
125,2.6% |
90,7.0% |
70,16.1% |
<0.001 |
|
Chronic obstructive pulmonary disease |
227,2.0% |
91,1.8% |
26,1.9% |
9,2.0% |
0.8 |
|
Low Education level |
7798,72.3% |
3623,74.7% |
984,76.4% |
327,75.3% |
<0.001 |
|
Intermediate and high education level |
2810,27.7% |
1161,25.3% |
288,23.6% |
105,24.7% |
|
|
Coronary artery disease, % |
|
|
|
|
|
|
Stroke history, % |
582,6.7% |
255,6.0% |
50,4.2% |
18,4.3% |
0.001 |
|
Body mass index mean |
27.3 ± 1.4 |
32.0 ± 1.4 |
36.9±1.4 |
43.7±4.2 |
<0.001 |
|
Obesity (≥30) |
|
|
|
|
|
|
Systolic blood pressure (mmHg) |
138.8±19.4 |
139.5±19.5 |
140.6±20.2 |
141.3±20.6 |
<0.001 |
|
Diastolic blood pressure |
79.1±10.9 |
79.6±11.0 |
79.3±11.0 |
80.3±11.4 |
0.001 |
|
Heart Rate |
74.0±10.9 |
74.0±10.7 |
74.0±10.9 |
73.7±11.4 |
0.26 |
|
Glycaemia |
1.77±5.63 |
1.79±5.76 |
1.59±3.86 |
1.52±0.81 |
<0.001 |
|
Of????ice based Globorisk score |
9.67±6.27 |
11.14±7.46 |
10.32±5.96 |
10.12±5.92 |
0.003 |
|
LVH on EKG |
11.30% |
9.90% |
11.20% |
12.80% |
0.036 |
|
LVH on TTE |
13.20% |
12.40% |
14.70% |
17.60% |
0.004 |
|
Microalbuminuria |
527,32.5% |
312,33.2% |
101,38.7% |
28,27.4% |
<0.001 |
|
Drug treatment: |
|
|
|
|
<0.001 |
|
no drugs |
1753,14.7% |
797,15.0% |
205,14.8% |
60,11.5% |
|
|
Monotherapy |
2209,48.5% |
1688,44.4% |
408,40.9% |
111,32.3% |
|
|
Bitherapy |
2324,25.4% |
1553,27.3% |
417,28.8% |
135,30.6% |
|
|
Tritherapy or more |
6161,11.4% |
746,13.3% |
642,15.4% |
126,25.6% |
|
|
ACE inhibitors |
|
||||
|
ARBs |
|||||
|
CCB diuretics Betablockers |
|||||
|
Diuretics |
8715,20.8% |
1049,22.2% |
271,21.1% |
92,20.8% |
0.24 |
|
Betablockers |
1652,21.9% |
1049,22.0% |
291,22.9% |
105,24.1% |
0.62 |
|
Salt restriction |
55.70% |
2724,54.4% |
685,51.8% |
217,48.6% |
0.001 |
|
Drug compliance |
78.40% |
3870,76.8% |
1037,78.5% |
338,75.1% |
0.062 |
|
Physical activity |
15.60% |
562,11.7% |
124,!9.7% |
29, 6.5% |
<0.001 |
|
ABPM |
2.30% |
3.00% |
2.40% |
4.30% |
0.003 |
|
SMBP |
6.60% |
7.20% |
7.30% |
5.40% |
0.24 |
ABPM : Ambulatory Blood Pressure Measurment ; ACE : Angiotensin Converting Enzyme; ARBs : Angiotensin Receptor Blokers; CCB: Calcium Channel Blockers ; LVH : Left Ventricular Hypertrophy; EKG : Electrocardiogramm; SMBP : Self Measurment of Blood Pressure ; TTE: Transthoracic Echocardiography.
Subgroup analysis of different obesity patterns
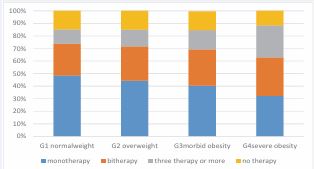
The group of patients with the highest BMI had higher BP than the other groups with greater left ventricular impact. Half of this population were diabetics and 28.6% had microalbuminuria. We had difficulties in the management of these patients and only three quarter of them had therapeutic compliance; 32.3% were on monotherapy, 30.6 % under bitherapy and 25.6% under triple therapy, 11.5% were untreated (Figure 2).
Figure 2 Comparison of number of antihypertensive drugs among the four patters of obesity.
Only 20.8% were under diuretics despite a salty restriction in only 48.6%. Patients who practice regular physical activity did not exceed 15.6% in all groups combined. All patients had a GLOBORISK score between 20% and 30%, which classifies them at high risk of fatal or non-fatal cardiovascular events over the next 10 years (Table 1).
Analysis of factors associated with uncontrolled blood pressure in the group of obese hypertensive patients
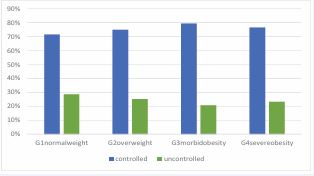
The uncontrolled AHT risk increased rapidly with the increase of BMI (Figure 3).
Figure 3 Comparaison of the prevalence rate of hypertension among different obesity patterns and BP control.
The risk of uncontrolled of BP is increased when obesity, whatever its grade, is associated with one of the following factors: smoking (p<0.001), diabetes mellitus (p=0.06), microalbuminuria (p=0.001) and apnea syndrome (p=0.026) (Table 2, Figure 4).
Table 2: Bi-variable analyses on factors associated with uncontrolled BP among adult patients whatever pattern of obesity.
|
|
Controlled HTN |
Uncontrolled HTN |
p-value |
|
Obesity and smoking |
38.8% |
61.2% |
<0.001 |
|
Obesity and diabetes |
45.7% |
54.3% |
0.06 |
|
Obesity and coronary artery disease/stroke history |
47.0% |
53% |
0.47 |
|
Obesity and renal failure |
43.5% |
56.5% |
0.16 |
|
Obesity and microalbuminuria |
44.4% |
55.6% |
0.001 |
|
Obesity and hypothyroidism |
49.2% |
50.8% |
0.33 |
|
Obesity and apnea syndrome |
40.7% |
59.3% |
0.026 |
|
Obesity and LVH |
46.6% |
53.4% |
0.84 |
HTN: Hypertension, LVH: Left Ventricular Hypertrophy
Figure 4 Subgroup analyses for the uncontrolled HTN in the severe obesity group compared with the normal weight group
Out of the four analyzed groups, the one group of patients with severe obesity had more uncontrolled BP (55.8%, p=0.008).Under each subgroup, in risk factors analysis, diabetes mellitus and heart rate > 80 bpm (why 80 not 120, explain in the methods section) were significant determinant of uncontrolled AHT whatever the obesity patter was. Throughout our study, it seems that diabetes mellitus and age under 60 years are protective factors against uncontrolled AHT (in severe obesity AHT group OR 0.89 CI 0.87-0.91, and OR 0.85 CI 0.83-0.87, respectively) (Table 3).
Table 3: Subgroup analyses for selected variables associated with uncontrolled BP in moderate, morbid and severe obesity groups compared with the normal weight group.
|
|
Moderate obesity |
Normal weight |
OR |
P |
|
Age >60 YO |
45.50% |
54.50% |
1.50 [1.35-1.67] |
<0.001 |
|
Smoking |
11.20% |
20.80% |
0.73 [0.68-0.77] |
<0.001 |
|
diabetes |
46.60% |
36.70% |
1.21 [1.15-1.38] |
<0.001 |
|
Coronary artery disease |
6.30% |
7.90% |
0.89 [0.81-0.98] |
0.022 |
|
HeatRate>80 |
25.10% |
19.70% |
1.18 [1.10-1.26] |
<0.001 |
|
|
morbid obesity |
Normal weight |
OR/CI |
P |
|
Age >60 YO |
43.00% |
57.60% |
0.89 [0.87-0.91] |
<0.001 |
|
Smoking |
5.90% |
17.50% |
0.85 [0.83-0.87] |
<0.001 |
|
diabetes |
46.90% |
36.30% |
1.09 [1.06-1.12] |
<0.001 |
|
Coronary artery disease |
|
|
|
|
|
HR |
22.60% |
115.50% |
1.11 [1.07-1.15] |
<0.001 |
|
|
severe obesity |
Normal weight |
OR |
P |
|
Age >60 YO |
39.00% |
57.60% |
0.94 [0.92-0.96] |
<0.001 |
|
Smoking |
4.60% |
17.50% |
0.94 [0.93-0.95] |
<0.001 |
|
diabetes |
50.70% |
36.30% |
1.05 [1.03-1.07] |
<0.001 |
|
Coronary artery disease |
|
|
|
|
|
HR |
20.40% |
15.50% |
1.03 [1.01-1.05] |
0.008 |
HR: Heart Rate; CI: Confidence Interval, OR: Odds Ratio; YO: Years Old
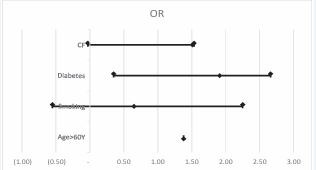
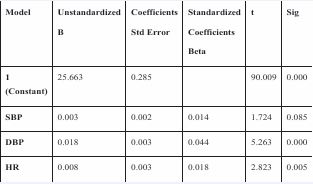
Analyses adjusted for age, diabetes mellitus, smoking and heart rate, identified that heart rate and DBP were independently associated with uncontrolled AHT in obese patients (Figure 5)
Figure 5 Multivariate analysis of factors independently associated with uncontrolled HTN in obese people. HR Heart Rate; DBP: Diastolic Blood Pressure; SBP: Systolic Blood Pressure.
Particularity of obesity arterial hypertension in young adults
Adults between 15 and 64 years are predominant in the Tunisian population [17], We identified 3215 persons, 83.2% had been hypertensive for at least six months; the female predominance was clear, diabetes mellitus affects 33% of this population, 4.2% already had a microalbuminuria and microalbuminuria and 46% had an uncontrolled BP, and 16% of these patients were untreated.Although GLOBORISK is not applicable under the age of 40 years (methods old discussion) but association between uncontrolled AHT and the presence of visceral impact (microalbuminuria and ventricular hypertrophy) made that at least 33.9% of this population is at high cardiovascular risk.
DISCUSSION
Through NATURE HTN register of Tunisian hypertensive patients, our study highlights a linear association between obesity and hypertension HTN, where higher BMI correlates with more uncontrolled blood pressure [6,7]. Obesity is now recognized as an independent risk factor for high BP, high cholesterol, type 2 diabetes and coronary artery diseases. Several pathophysiological mechanisms may contribute to the development of hypertension in obesity including insulin resistance, inflammation, the renin-angiotensin-aldosterone system and oxidative stress.Obesity induced hypertension is also linked to significant systemic and cardiac inflammation, it is initially characterized by volume overload increased cardiac output, LV dilation and concentric hypertrophy which predispose individuals to a severe diastolic dysfunction loading to HFpEF [15]. The predominance of hypertension in females can be partially explained by hormonal status. During the post menopausal stage, estrogen production declines, leading to a subsequent decrease in nitric oxide availability and increased vasoconstriction. As a result, women lose the cardiovascular protection they previously had against hypertension. Additionally, the higher prevalence of obesity among females may be attributed to an imbalance between excessive caloric intake and insufficient physical activity. A concerning issue is the rising trend of obesity-related hypertension in younger women, who, compared to men, should still benefit from hormonal protection. This phenomenon is likely linked to a sedentary lifestyle, often associated with domestic roles (e.g., housework) and a lack of encouragement for physical activity, along with increased consumption of processed and prepared foods.Furthermore, over 70% of our study population have a low educational level, which may serve as a significant a barrier for to effective therapeutic education and the adoption of healthier lifestyles. This finding aligns with a large-scale study conducted by Kan Sun et al., involving 101959 Chinese participants, which demonstrated that a lower educational level is associated with poor blood pressure control. These results highlight the importance of improving educational access and attainment in countries where education remains limited, emphasizing the role of public policy in supporting effective hypertension management [18,19]. There is a strong association between obesity, tobacco use and uncontrolled hypertension as confirmed by numerous studies. Mirzaei et al., demonstrated that tobacco smoking is one of the main predictors of uncontrolled blood pressure particularly among obese individuals [20]. the univariate analysis of the three obesity subgroups regarding factors influencing blood pressure control, tobacco appeared to be a protective factor (OR 0.85 CI 0.83 0.87). However, this result may be influenced by a bias as individuals diagnosed as uncontrolled hypertension may consciously quit smoking following medical intervention or due to self-motivation. Additionally, individuals over 60 years of age appear to be less affected by the combination of obesity and poor blood pressure control, possibly because obesity disproportionately impacts younger populations. Our study focused on the strong association between DBP, cardiac frequency and obesity. Actually, subcutaneous fat tissue, particularly in cases of central obesity, releases vasoactive and inflammatory mediators that stimulate peripheral α1 and β adrenergic receptors while inhibiting baroreflex sensitivity. Furthermore, hyperleptinemia observed in individuals with obesity promotes conversion of norepinephrine and increases sympathetic nervous system activity [21]. Appel et al., reported that behavioral interventions including increased physical activity, reduced salt and alcohol consumption, and weight loss, systolic BP by 12.5 mmHg and diastolic BP by 5.8 mmHg [22]. This led us to consider the following question: is there a specific BMI threshold that could predict the risk of uncontrol blood pressure failure and at which more aggressive interventions should be implemented? Although the AUC of BMI was not statistically significant in our analysis, we observed that a BMI of 27.2 kg/m² appears to be a potentially alarming value. In a cross-sectional study conducted by Xiaohan Lee et al., involving 2,801 adults, the authors compared the predictive performance of several parameters. They identified the optimal BMI cut-off points for detecting hypertension as 25.72 kg/m² for men and 23.46 kg/m² for women [23]. We draw attention to obese hypertensive young adults, a population subgroup in our study, who warrant detailed characterization in order to initiate urgent treatment This severe condition imposes a significant physical burden and, more importantly, an economic one.The majority of obese hypertensive adults in our cohort had essential hypertension, while 16.8% were newly diagnosed with hypertension, which may be either essential or secondary. It is also important to consider that a considerable proportion of this population may fall into the category of high-normal blood pressure Patients with essential HTN often had a family history of the condition, indicating that obesity is not the sole contributing factor. Environmental and genetic influences are likely involved, and more detailed information on lifestyle factors such as methamphetamine use or oral contraceptive intake is needed to better understand the underlying causes. Despite a female predominance of obese young adults who are generally thought to be protected by hormonal factors, organ damage was still observed. This included left ventricular hypertrophy (9.8%), renal failure (3.3%), microalbuminuria (4.2%), and coronary artery disease (1.6%), largely due to the coexistence of diabetes. Unfortunately, a significant number of these patients are not receiving treatment. This may be due to reluctance regarding the early initiation of antihypertensive therapy, fear of chronic disease labeling, or in young women, concerns related to future pregnancy and the desire to conceive. The globorisk score among of young hypertensive adults is already elevated, even in those with normal weight, suggesting that additional factors such as waist circumference may contribute to this increased cardiovascular risk.
STUDY LIMITATIONS
Although we conducted a detailed analysis of the effects of different obesity patterns on BP control, several limitations should be acknowledged. First we did include the waist circumference (WC) in our analysis which could have been a valuable parameter particularly in women for predicting uncontrolled blood pressure. Second, despite adjusting for multiple covariates, we cannot completely rule out the influence of residual confounding factors on our findings.
CONCLUSION
In summary, obesity related hypertension is a common phenotype particularly among women. Blood pressure control is closely linked to the severity of obesity with a strong association between DBP, CF and uncontrolled HTN. Among young adults with obesity and uncontrolled HTN, diabetes is also frequently, present, contributing to early organ damage. These findings highlight the urgent need for early intervention strategies in this population, focusing on lifestyle modification to reduce cardiovascular morbidity and mortality associated with this condition.
DECLARATION OF COMPETING INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ACKNOWLEDGMENTS
We would like to thank Ahmed Rebaii for his technical support. We would also like to thank Tunisian society of cardiology as well as data collectors and supervisors for their unreserved contribution.
REFERENCES
- Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017; 5: 161.
- GBD 2015 Obesity Collaborators; Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017; 377: 13-27.
- Tadic M, Cuspidi C. Obesity and resistant hypertension: Never ending story. J Clin Hypertens (Greenwich). 2019; 21: 1516-1518.
- Koliaki C, Dalamaga M, Liatis S. Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten? Curr Obes Rep. 2023; 12: 514-527.
- Landi F, Calvani R, Picca A, Tosato M, Martone AM, Ortolani E, et al. Body Mass Index is Strongly Associated with Hypertension: Results from the Longevity Check-up 7+ Study. Nutrients. 2018; 10: 1976.
- Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987; 16: 235-251.
- Ben Romdhane H, Ben Ali S, Skhiri H, Traissac P, Bougatef S, Maire B, et al. Hypertension among Tunisian adults: results of the TAHINA project. Hypertens Res. 2012; 35: 341-347.
- Abid L, Hammami R, Chamtouri I, Drissa M, Boudiche S, Bahloul M, et al. Epidemiologic features and management of hypertension in Tunisia, the results from the Hypertension National Registry (NaTuRe HTN). BMC Cardiovasc Disord. 2022; 22: 131.
- Abid L, Hammami R, Abdesselem S, Boudiche S, Hédi BS, Sayahi K, et al. Design and Rationale of the National Observational Multicentric Tunisian Registry of Hypertension: Protocol for Evaluating Hypertensive Patient Care in Clinical Practice. JMIR Res Protoc. 2022; 11: e21878.
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71: 1269-1324.
- Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005; 67: 2089-2100.
- Global Recommendations on Physical Activity for Health. RECOMMENDED POPULATION LEVELS OF PHYSICAL ACTIVITY FORHEALTH. Geneva: World Health Organization. 2010; 4.
- Carlson DJ, Dieberg G, Mcfarlane JR, Smart NA. Blood pressure measurements in research: suitability of auscultatory, beat-to-beat, and ambulatory blood pressure measurements. Blood Press Monit. 2019; 24: 18-23.
- Bayram N, Ako?lu H, Sanri E, Karacabey S, Efeo?lu M, Onur O, et al. Diagnostic Accuracy of the Electrocardiography Criteria for Left Ventricular Hypertrophy (Cornell Voltage Criteria, Sokolow-Lyon Index, Romhilt-Estes, and Peguero-Lo Presti Criteria) Compared to Transthoracic Echocardiography. Cureus. 2021; 13: e13883.
- Abid L, Zakhama L, Trabelsi R, Abdesslem S, Alouane L, Bezdah L, et al. Guide de Pratique Clinique. Prise en charge de l’hypertension artérielle chez l’adulte en Tunisie [Clinical Practice Guidelines. Management of Hypertension in Tunisian Adults]. Tunis Med. 2021; 99: 767-846.
- Abid L, Zakhama L, Trabelsi R, Abdesslem S, Alouane L, Bezdah L, et al. Clinical Practice Guidelines. Management of Hypertension in Tunisian Adults. Tunis Med. 2021; 99: 768-846.
- Statistica Research Department.18 Avr.2024
- Mouton AJ, Li X, Hall ME, Hall JE. Obesity, Hypertension, and Cardiac Dysfunction: Novel Roles of Immunometabolism in Macrophage Activation and Inflammation. Circ Res. 2020; 126: 789-806.
- Sun K, Lin D, Li M, Mu Y, Zhao J, Liu C et.al. Association of education levels with the risk of hypertension and hypertension control: a nationwide cohort study in Chinese adults. J Epidemiol Community Health. 2022; 76: 451-457.
- Mirzaei M, Mirzaei M, Bagheri B, Dehghani A. Awareness, treatment, and control of hypertension and related factors in adult Iranian population. BMC Public Health. 2020; 20: 667.
- Gruber T, Pan C, Contreras RE, Wiedemann T, Morgan DA, Skowronski AA, et al. Obesity-associated hyperleptinemia alters the gliovascular interface of the hypothalamus to promote hypertension. Cell Metab. 2021; 33: 1155-1170.e10.
- Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003; 289: 2083-2093.
- Lee X, Gao Y, Zhang Y, Feng Y, Gao L, Wang A, et al. Comparison of 10 obesity-related indices for predicting hypertension based on ROC analysis in Chinese adults. Front Public Health. 2022; 10: 1042236.