Impedance Cardiography to Guide Antihypertensive Treatment in a Patient with Difficult-to-Treat Hypertension
- 1. West Palm Beach VA Medical Center, West Palm Beach, USA
Abstract
In this case report, we describe the use of impedance cardiography (ICG) to guide antihypertensive therapy in a patient with difficult-to-treat hypertension illustrating the potential benefit of use in clinical practice. Through the identification of our patient’s hemodynamic phenotype, low cardiac index and elevated systemic vascular resistance index, and medication changes directed toward these patient-specific parameters therapy was streamlined to achieve target blood pressure with a net reduction in medications. Despite decades of research and guideline publications aiming to improve hypertensive control approximately half of hypertensive patients fail to reach BP targets using a stepped-care approach. Recent evidence advocates for more intensive BP goals in select patient populations, which would require therapy intensification for millions of hypertensive adults. Utilizing novel strategies, such as ICG, to personalize antihypertensive regimens has the potential to improve overall BP control without an increase in medications, or in certain cases, a reduction in medication. This case report illustrates the utilization of ICG as a method of providing more effective BP control while potentially decreasing burden on patients, and the healthcare system, through avoiding use of likely ineffective and potentially harmful therapies.
Keywords
• Impedance cardiography
• Hypertension
• Blood pressure
• Non-invasive hemodynamic monitoring
• Precision medicine
Citation
Cave BE, Hough AR (2017) Impedance Cardiography to Guide Antihypertensive Treatment in a Patient with Difficult-to-Treat Hypertension. Ann Clin Exp Hypertension 5(2): 1050.
INTRODUCTION
Hypertension is highly prevalent in the United States and globally, affecting approximately 80 million and 1 billion adults, respectively [1]. If untreated, or poorly controlled, hypertension is a major risk factor for cardiovascular disease, including heart failure, myocardial infarction, chronic kidney disease and stroke [1]. From 2009 to 2012, 76.5% of patients with hypertension received blood pressure (BP) treatment; however 45.9% of patients were not adequately controlled to a BP target of less than 140/90 mmHg [1]. Rates of treatment-resistant hypertension, defined as the inability to achieve BP targets despite three or more antihypertensives prescribed at maximally tolerated doses or the achievement of BP targets with four or more agents, are also on the rise. In clinical trials, rates of treatment resistant hypertension are estimated to be present in 20-30% of patients [2]. The rate of resistant hypertension in clinical practice is largely unknown.
The current paradigm for hypertension control is based on a stepped-care approach in which antihypertensives are added sequentially until a patient’s particular BP targets are achieved. However, unless there is a clear adverse reaction to an agent, no medications are removed from the regimen. The classic example for this type of stepped-care strategy is the Antihypertensive and Lipids-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [3]. In this landmark trial only 66% of patients achieved BP targets of less than 140/90 mmHg. Those that reached target required an average of 2 antihypertensive agents and 23% of patients required 3 or more medications [3]. Given the impact of hypertension and hypertension treatment on the population and the healthcare system, providers should be aware of available alternative treatment strategies which may improve global control rates and/or streamline the use of effective antihypertensive therapies.
Several such alternative strategies for hypertension control have been evaluated and include pharmacologic, such as initiation of multidrug combinations at treatment onset, and non pharmacological approaches, such as renal denervation, plasma renin activity (PRA)-guided therapy, and impedance cardiography (ICG)-guided therapy. The latter strategy is based on the notion that hypertension is the result of a pathophysiological hemodynamic imbalance which is attributed to derangements in cardiac output (CO), systemic vascular resistance (SVR), and/or blood volume [4]. ICG is a non-invasive monitoring tool which establishes a patient’s hemodynamic phenotype, and provides individual hemodynamic measurements (CO, cardiac index (CI), SVR, systemic vascular resistance index (SVRI), stroke volume ratio (SVr), thoracic fluid content (TFC) and total body impedance (Zo) which can be used to determine why a particular patient’s blood pressure may be elevated [4,5]. Measurements can be gathered easily in the ambulatory setting with a monitoring device which uses four sets of dual sensors placed on either side of the neck and chest at the mid-axillary region to deliver a lowamplitude, high-frequency alternating current to sense changes in thoracic fluid volume during the cardiac cycle to provide hemodynamic measurements [4]. Based on ICG measurements, algorithms have been proposed and studied for personalization of antihypertensive regimens [4].
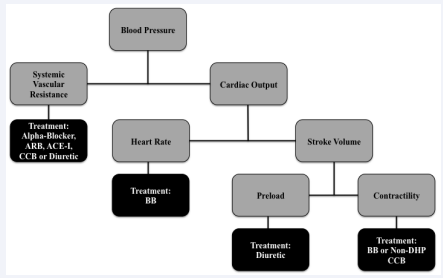
Figure 1 Blood Pressure Physiology and Impedance Cardiography Principles Abbreviations: DHP: Dihydropyridine; ACE-I: Angiotensin-Converting Enzyme Inhibitor; ARB: angiotensin II Receptor Blocker; CCB: Calcium Channel Blocker; BB: Beta-Blocker
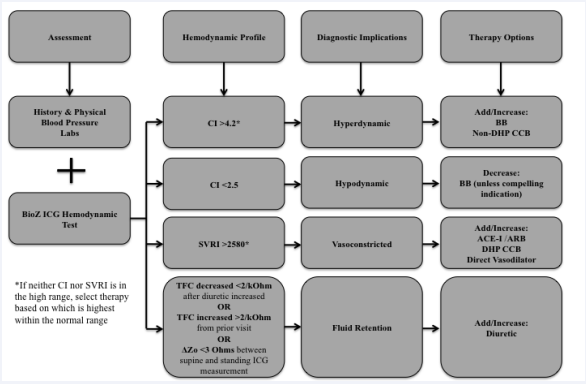
Proposed algorithms follow a general principal Figure 1 of selecting medication(s) that antagonize the underlying pathology expected to be responsible for elevated blood pressure. Medications are chosen based on hemodynamic measures such that centrally acting agents are adjusted based on CI, vasoactive agents are used to target SVRI, and diuretic adjustment based on TFC and Zo Figure 2 [6,7]. Initial medication selection should be directed by whether CI or SVRI are in the ‘high’ range, and in the event that both are in the normal range, the more pronounced metric should be addressed first [4-7]. Conversely, if a given parameter is significantly reduced offending agents responsible for excessive effects may be tapered or stopped (e.g., stopping beta-blocker therapy in a patient with ‘low’ CI). Several studies have demonstrated the superiority of utilizing hemodynamic measurements to guide hypertensive treatment compared to empiric selection using guideline recommendations, both in the general practitioner setting and with hypertensive specialists Table 1 [4,6,7].
Table 1: Previous Impedance Cardiography Trials
| Baseline Office BP | Final Office BP | Change Office BP | |||||||||
| NonICG | ICG | p-valuec | Non ICG | ICG | p-valuec | Non ICG | ICG | p-valuec | |||
| Taler [7] | Hemodynamic care versus hypertensive specialist in resistant hypertension (N=104) | Systolic | 173 | 169 | NS | 147 | 139 | <0.01 | -26a | -30a | NR |
| Diastolic | 91 | 87 | NS | 79 | 72 | <0.01 | -12a | -14a | NR | ||
| Smith[6] | Hemodynamic care versus standard care (N=164) | Systolic | 147 | 148 | NS | 136 | 129 | <0.01 | -11 | -19 | <0.01 |
| Diastolic | 87 | 89 | NS | 82 | 76 | <0.01 | -5 | -12 | <0.001 | ||
| Krzesinski [11] | Hemodynamic care versus standard care in metabolic syndrome (N=82) | Systolic | 145.0 | 150.6 | NS | 135.3 | 132.5 | NS | -10.7 | -18.1 | 0.012 |
| Diastolic | 94.7 | 96.5 | NS | 85.8 | 84.3 | NS | -8.9 | -12.2 | 0.037 | ||
| Krzesinski [12] | Hemodynamic care versus empiric care (N=128) | Systolic | 147.1 | 148.9 | NS | 136.1 | 131.6 | 0.036 | -11.0 | -17.3 | 0.008 |
| Diastolic | 94.8 | 95.9 | NS | 87.0 | 83.7 | 0.013 | -7.7 | -12.2 | 0.0008 | ||
| Krzesinski [13] | Hemodynamic care versus empiric care (N= 241) | Systolic | 143.7 | 145.4 | NS | 129.4b | 127.1b | NR | -14.3 | -18.3 | <0.05 |
| Diastolic | 92.2 | 93.2 | NS | 83.7b | 81.3b | NR | -8.5 | -11.9 | <0.005 | ||
| Krzesinski [14] | Hemodynamic care versus empiric care (N= 121) | Systolic | 140.9 | 142.0 | NS | 120.9 | 120.2 | NS | -19.9 | -21.8 | NS |
| Diastolic | 90.0 | 90.8 | NS | 78.2 | 76.7 | NS | -11.8 | -14.1 | NS | ||
| a Calculated from baseline and final results, not reported by study; b Calculated from baseline and final change in blood pressure, not reported by study; c Comparison of non-ICG to ICG groups; Abbreviations: NS: Not Significant; NR: Not Reported; BP: Blood Pressure; ICG: Impedance Cardiography | |||||||||||
The following case report demonstrates a realworld utilization of ICG-guided therapeutics and serves as an example of how a personalized treatment strategy can improve BP control while curtailing medication use versus the result of stepped-care strategy.
Figure 2 Impedance Cardiography-Based Hypertension Treatment Algorithm Abbreviations: CI: Cardiac Index; SVRI: Systemic Vascular Resistance Index; TFC: Thoracic Fluid Content; ICG: Impedance Cardiography; DHP: Dihydropyridine; ACE-I: Angiotensin-Converting Enzyme Inhibitor; ARB: Angiotensin II Receptor Blocker; CCB: Calcium Channel Blocker; BB: BetaBlocker *If neither CI nor SVRI is in the high range, select therapy based on which is highest within the normal range.
CASE PRESENTATION
A 68 year-old Caucasian male was referred to the pharmacotherapy clinic for uncontrolled hypertension. His medical history was significant for coronary artery disease with a history of myocardial infarction, hypertension, dyslipidemia, obstructive sleep apnea (compliant with continuous positive airway pressure device use), gastroesophageal reflux disease, allergic rhinitis, degenerative joint disease, and obesity. He also complained of shortness of breath, including dyspnea with minimal exertion, which had been an ongoing and unchanged. At the time of care the patient’s BP target was set at less than 140/90 mmHg based on guideline recommendations [8]. The patient was provided recommendations regarding non pharmacological methods to improve BP control. However, no significant lifestyle changes were made during the treatment period that would be expected to have an impact on patient’s treatment course.
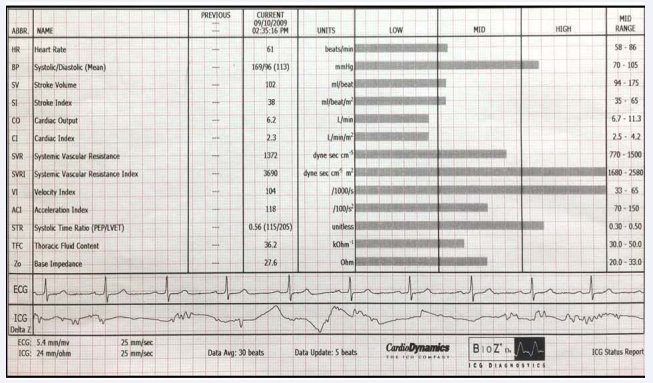
Figure 3 Impedance Cardiography Results.
On referral, the patient’s medication regimen consisted of clonidine 0.2mg by mouth three times daily, furosemide 40mg by mouth once daily, valsartan 160mg by mouth twice daily, amlodipine 10mg by mouth once daily, spironolactone 25mg by mouth once daily, and metoprolol succinate 200mg by mouth once daily. The patient’s BP at first visit was 151/74 mmHg with a pulse of 54 beats per minute. An ICG was performed using BioZ device (Cardiodynamics, CA) with results from ICG shown in Figure 3. The patient’s SVRI was elevated and the CI was reduced suggesting that the patient’s BP elevation was a result of increased vasoconstriction and possibly exacerbated by reduced CO (cardiac output). Given these findings, metoprolol succinate was reduced to 100mg by mouth daily and clonidine reduced to 0.1mg by mouth three times daily to increase CI and amlodipine was changed to nifedipine CC 60mg by mouth twice daily in effort to target the elevated SVRI. In Table 2, we provide a listing of all antihypertensive medication changes and pertinent vital signs by appointment.
Table 2: Therapeutic Course.
| Visit 1 (Initial appointment) | Visit 2 | Visit 3 | Visit 4 | Visit 5 (Final Appointment) | |
| Office BP | 151/74 | 144/90 | 140/90 | 105/71 | 121/84 |
| Pulse | 56 | 56 | 56 | 91 | 84 |
| Medication Regimen |
a. Valsartan 160mg BID b. Metoprolol Succinate 200mg daily c. Spironolactone 25mg daily d. Amlodipine 10mg daily e. Clonidine 0.2mg TID f. Furosemide 40mg daily |
a. Valsartan 160mg BID b. Metoprolol Succinate 100mg daily c. Spironolactone 25mg daily d. Nifedipine CC 60mg BID e. Clonidine 0.1mg TID f. Furosemide 40mg daily |
a. Valsartan 160mg BID b. Metoprolol Succinate 100mg daily c. Spironolactone 25mg daily d. Nifedipine CC 60mg BID e. Clonidine 0.1mg TID f. Furosemide 40mg daily g. Modafinil 100mg daily |
a. Valsartan 160mg BID b. Metoprolol Succinate 100mg daily c.Spironolactone 25mg daily d. Nifedipine CC 60mg BID e.Chlorthalidone 25mg daily f. Modafinil 100mg daily |
a. Valsartan 160mg BID b. Metoprolol Succinate 100mg daily c.Spironolactone 25mg daily d. Nifedipine CC 60mg BID e.Chlorthalidone 25mg daily |
| Changes to regimen |
1. Metoprolol succinate decreased 2. Clonidine decreased 3. Amlodipine converted to Nifedipine CC |
1. No changes due to pending pulmonology evaluation that initiated: Modafinil 100mg daily for dyspnea and lethargy | 1. Furosemide converted to chlorthalidone 2. Clonidine tapered off over a week | 1. Modafinil discontinued | 1. No changes; BP controlled |
| Abbreviations: Nifedipine CC: Nifedpine Extended-Release; BID: Twice Daily; TID: Three Times Daily; BP: Blood Pressure; BPM: Beats Per Minute | |||||
At the second appointment, office BP had decreased to 144/90 mmHg, however patient had continued symptoms of dyspnea and lethargy. No changes were made at this visit as patient was pending pulmonology evaluation of symptoms. At that visit, pulmonology initiated modafinil 100mg by mouth daily to target patient’s significant lethargy.
BP remained unchanged at the time of the third appointment (140/90 mmHg) and decision was made to resume medication optimization. Pulse remained unchanged (54 BPM). Clonidine was tapered off in effort to continue to improve the reduced CI (metoprolol succinate was not stopped or further reduced given perceived compelling indication for therapy based on acute coronary syndrome history) and furosemide was converted to chlorthalidone for more effective and sustained antihypertensive effect in part through further reduction in SVRI [6,7,9].
By the fourth appointment, BP had been substantially reduced (105/71 mmHg) and HR increased (90 BPM). Lethargy and dyspnea symptoms previously reported had now resolved and modafinil was discontinued. These symptoms were ultimately attributed at least in part to iatrogenic CO reductions from clonidine and metoprolol succinate.
Upon the fifth and final visit, BP was controlled (121/84 mmHg) and with reduced HR (84 bpm). Patient remained asymptomatic, so no medication changes were made. Throughout several visits, using an ICG as a means to guide medication cessation and selection, BP was eventually controlled with a reduction in medication burden of one medication and also the discontinuation of an unnecessary medication, modafinil.
DISCUSSION
In this case report, we describe the use of ICG findings as a means to guide antihypertensive therapy in a patient with difficult-to-treat hypertension and illustrate the potential benefit of integrating of this tool into clinical practice. The result included improved BP control, a net reduction in medications and global symptom improvement. Through the identification of our patient’s hemodynamic phenotype, low CI and elevated SVRI, we were able to streamline hypertensive therapy through dose reduction of metoprolol succinate and cessation of clonidine to increase CI, and change to high dose nifedipine versus amlodipine and to chlorthalidone versus furosemide in effort to further lower SVRI.
During the treatment adjustment period, the patient made no significant changes in lifestyle modifications, there for it is unlikely that non pharmacological interventions factored into improved BP control. Our patient had a compelling indication for beta-blocker use; however without hemodynamic monitoring, it would be unlikely that the dose would have been reduced. It is possible that excessive CI reduction could trigger a further increase SVRI and greater elevations in BP [6,7]. Our patient’s initial antihypertensive regimen at consult was an atypical empiric regimen by guideline standards; however we made a conscious effort to implement changes in favor of evidence-based medications when tailoring therapy to individual hemodynamic parameters. Our patient likely would have benefited to ICG testing earlier in therapy as the empiric trials of medications resulted in a longer period of uncontrolled BP and drug-related adverse events.
Antihypertensive changes in this case were guided by SVRI and CI measures however other algorithms and evaluations for ICG-based therapy have also integrated assessment of supine versus standing Zo changes to guide diuretic therapy. Specifically, if standing Zo does not rise by >3 ohm, a fluid overload state is suggested and signals potential benefit from diuretic therapy initiation or intensification. This strategy has been integrated into our current ICG-guided therapy practices but was not used in this case specifically. The diuretic change in this case (loop to thiazide conversion) was done to utilize evidence based, long acting antihypertensives but also had benefit for this patient as it helped address the patient’s elevated SVRI [9]. A noted caveat with ICGguided antihypertensive therapy is that ICG results should not serve as an indication to forgo or remove anti-hypertensive medications with compelling indications based on presence of certain disease states (e.g., post myocardial infarction, heart failure with reduced left ventricular ejection fraction).
ICG is applicable to a wide group of patients but is subject to some technical limitations which can confound and limit interpretation including patient weight less than 66 pounds or more than 341 pounds and heights less than 47 inches or greater than 75 inches, and the presence of minute-ventilation pacemakers, severe aortic insufficiency, recurrent premature ventricular contractions, or atrial fibrillation [5]. The time to complete ICG evaluation is brief at approximately 10 minutes [10].
ICG has the potential to improve rates of patients achieving BP goals and often without the need for additional antihypertensive therapy. In a primary care setting, ICG improved BP control rates (BP <140/90) in the hemodynamic arm versus standard with control rates of 77% vs 57%, respectively (p <0.01) [6]. Even when compared to hypertensive specialists, ICG-guided antihypertensive therapy resulted in more patients achieving BP goals of less than 140/90 mmHg, 33% and 56% respectively (p150 mmHg [13]. The FINEPATH study sought to expand on prior short-term studies and evaluate hemodynamic care versus standard care over one year. ICG-guided therapy resulted in greater BP reduction, although findings did not achieve statistical significance [14]. However similar to previous studies, findings are limited by small sample size which limits statistical power and perhaps with larger sample size the results could have clinically significance based on the findings of The Blood Pressure Lowering Treatment Trialists’ Collaboration associating even slight reductions in BP of -4/-3 mmHg with relative risk reduction in stroke and major cardiovascular events of 23% and 15%, respectively [15]. Details of the clinical evaluations of ICG-guided antihypertensive therapy versus traditional approaches are summarized in Table 1.
The potential benefit of ICG-guided antihypertensive therapy may be of even greater importance in the near future given the results of the SPRINT trial, which showed that among certain patients with or at high risk of cardiovascular disease, intensive systolic blood pressure (SBP) reduction as measured by automated office blood pressure monitoring (<120 mmHg) resulted in a mortality benefit versus a more traditional SBP target (<140 mmHg) [16]. Although not currently reflected in practice guidelines, one would anticipate that given the positive results of SPRINT providers may pursue more intensive SBP goals for selected patients in clinical practice. In the context of the SPRINT trial results, ICG may be extremely useful in achieving more intensive goals in difficult to treat patients such as the one in this patient case. The ability to use ICG to aid in attainment of lower BP targets was seen in Smith, et al. which found a significantly greater percentage of patients achieving both a standard target BP of <140/90 and a more intensive goal of BP <130/85 with ICG-guided therapy versus standard therapy, 77% vs 57% and 55% and 27% respectively [6]. The integration of intensive SBP targets into practice is the source of debate but adoption of aggressive SPRINT based SBP targets into practice could place significant burden on US healthcare system resources as an estimated 16.8 million adults may be eligible for antihypertensive therapy initiation or intensification based adoption of SPRINT based targets [17]. Given these findings, consideration, and possibly further evaluation of, ICG-guided therapy and other possible strategies to help streamline antihypertensive therapies (e.g., PRA guided therapeutics) may be of value to the healthcare system in the future.
Finally, ICG has been determined to be both a shortterm and long-term cost-effective intervention for guiding antihypertensive therapies [10]. The majority of the costs associated with ICG are from up-front equipment purchase but estimates of ICG use suggest a short-term cost-savings of $16 per mmHg SBP reduction and $56 per mmHg diastolic BP reduction versus usual care. A long-term cost-savings of $476 per patient and 0.109 quality-adjusted life-years (QALY) gained per patient (1 QALY gained for every 9 patients treated with ICG) can be garnered by implementation of ICG.
Utilization of ICG to direct antihypertensive therapy has the potential for better BP control in patients with treatmentresistant hypertension, and potentially in pursuing more intensive BP goals. This strategy employs a personalized approach to treatment by targeting the driving force behind BP elevations and presents the opportunity to avoid, or discontinue, medications likely to not provide benefit. Given the current state of blood pressure control any strategy that can foster improved control rates is of value to providers and warrants consideration for integration into practice. This is especially true in the case of ICG as presented in this case, whose use may yield more effective BP control while potentially decreasing burden on patients, and the healthcare system, through avoiding use of likely ineffective and potentially harmful therapies.