Maternal Blood Pressure in Gestational Hypertensive Women and Birth Weight: an Inverse Relationship
- 1. Department of Obstetrics and Gynecology, Polytechnic University of Marche, Italy
Abstract
Objective: The aim of this study was to examine the relationship between maternal ambulatory blood pressure monitor measurements during pregnancy and birth weight in a population of women with gestational hypertension compared to pregnant healthy controls.
Patients and Methods: A prospective observational study was carried out within the obstetric departments of Salesi Hospital (Ancona, Italy). A total of 660 women were found to have hypertension (blood pressure >/=140/90 mm Hg) without significant proteinuria. A 24-hour automated ambulatory blood pressure recording was performed, and the results were compared with the principal outcome measure of birth weight.
Results: A significant inverse association (gradient: -10,274 p < 0.05; 95% IC -22.3 to -3.9) was found between ambulatory diastolic blood pressure measurement and birthweight. An increase of 1 mm Hg in mean diastolic blood pressure was associated with a fall in birth weight of 6 Gms. No such association was found between ambulatory systolic blood pressure mean and birthweight.
Conclusions: The novel of this study is a “pure” correlation between maternal blood pressure and birthweight and we found a significant inverse association between diastolic blood pressure and birthweight in nonproteinuric hypertensive pregnancies.
Citation
Giannubilo SR, Biagini A, Ballatori C, Ciavattini A (2016) Maternal Blood Pressure in Gestational Hypertensive Women and Birth Weight: an Inverse Relationship. Ann Clin Exp Hypertension 4(1): 1036.
INTRODUCTION
Gestational Hypertension (GH), Preeclampsia (PE), and Fetal Growth Restriction (FGR) are major causes of maternal and perinatal mortality and morbidity [1]. Clinical manifestation and progression of GH and preeclampsia are necessarily dependent on concomitance of several pathogenetic factors. Clinical studies have suggested that FGR often precedes the diagnosis of preeclampsia in the same pregnancy [2], consistent with that finding, morphologic studies have suggested that preeclampsia and FGR in general might share primary pathophysiologic mechanisms. Occlusive lesions in the maternal decidual uteroplacental (spiral) arteries, caused by failure of fetal trophoblasts to invade the arteries in early pregnancy, have been associated with the preeclampsia and FGR, suggesting that some cases of FGR differ from preeclampsia only in the maternal response to a shared placental pathology [3].
Placental disease is a characteristic of early preeclampsia [4,5] and that corresponds to the serious reduction in birth weight [2,6,7]. The reduction of birth weight has also been seen later onset preeclampsia [8,9] but other studies did not show differences in growth between mild and severe preeclampsia [10].
Although measurement of blood pressure is the most commonly used antenatal screening test, data on associations between maternal blood pressure and fetal size are limited and inconsistend [11]. By 24-hour automated blood pressure monitoring it is possible to evaluate association between maternal blood pressure and outcome measures, the neonatal size may have an important implication by the Barker hypothesis, which links birthweight with hypertension and other cardiovascular risk factors in adult life [12].
Apart from a preeclamptic background, congenital and chromosomal anomalies and intrauterine infections can cause FGR. Smoke, drug addiction, alcohol consumption, ethnic origin and pre-term birth, have also been implicated in the pathogenesis of FGR excluding those main causes, many cases of FGR still remain of obscure origin.
In the absence of overt hypertension or preeclampsia, pregnant women with FGR not depending on other factors have blood pressure higher than normal, although within clinic normotensive range, slightly higher levels of blood pressure can alter uterine and placental perfusion and determine fetal growth retardation [13].
The Gestational Hypertension is considered a slight disorder of pregnancy but the study of correlation with fetal growth may be interesting to elucidate in a pathophysiological and clinical way disorders more severe such as Preeclampsia.
This work addresses the association between 24-hour ambulatory blood pressure monitor measurements and birthweight in pregnancies complicated by GH compared to pregnant healthy controls.
PATIENTS AND METHODS
We studied 660 nulliparous women with gestational hypertension, consecutively recruited at Department of Obstetrics and Gynaecology of the Polytechnic University of Marche at Salesi Hospital (Ancona, Italy), between January 2005 and December 2015.
All patients recruited were Caucasian and delivered at term (>37 gestational weeks).
Gestational Hypertension was defined as a systolic blood pressure level of 140 mm Hg or higher or a diastolic blood pressure level of 90 mm Hg or higher, for at least two consecutive readings 6 or more hours apart, that occurs after 20 weeks of gestation in a woman with previously normal blood pressure, according to ACOG criteria [14].
In the study group were excluded women with chronic hypertension, those who received antihypertensive medication, multiple gestations, and women with specific pregnancy pathology e/o extra-pregnancy, women with uncertain gestational age and women who delivered before 37 weeks.
The birthweight was recorded and adjusted for sex and gestational age at birth by a software “GROW Program “(Gestation Related Optimal Weight) [15].
Blood pressure measuring
We have used two automatic ambulatory blood pressure recorders (SpaceLabs mod.90207, SpaceLabs Inc, Redmond, WA), programmed by a DOS-PC through a hardware interface (SpaceLabs mod.90209, SpaceLabs Inc, Redmond, WA). Ambulatory blood pressure was recorded by oscillometry every 30 minutes over 24 hours, for a total 48 daily measurements. Diastolic blood pressure recorded by oscillometry corresponds to auscultatory Korotkoff phase V, consistently with the recommendations of the Working group on High Blood Pressure in Pregnancy.
The instrument is self-calibrating, so that, when artefacts occur, measurements are repeated after 2’; this allows achieving almost 100% successful readings. Data recorded were automatically inserted in the hardware, saved on characteristic files and qualitatively analyzed.
We considered two groups of measures: centrality and rhythm analysis. The 24-h mean was chosen as the measure of centrality: it expresses the average level of BP and describes quantitative differences. The analysis of day-night and activityrest rhythm was performed by the cosinor method [16,17]. This is the most frequently used strategy for smoothing or modelling the 24-h BP curve, and is the equivalent to a Fourier periodic series with only one harmonic with a period of 24 h. The equation which describes the sinusoidal rhythm is Yt = M+A. cos (ω . t + Φ), where M (MESOR) is the rhythm-adjusted 24-h mean, A (amplitude) is the extent of the oscillation from M, ω is the angular frequency (2 P/ t), Φ (acrophase) is the time (clock hours) of the oscillation peak, and t is the temporal fraction of the period (t). Moreover, we also analyzed the statistical significance of the rhythm that shows the presence of a diphasic blood pressure pattern.
Statistical analysis
The relation between birthweight and maternal blood pressure was investigated by linear regression analysis, birthweight was analysed by multivariate analysis for variables such as maternal weight, maternal diastolic Mesor and maternal systolic Mesor. Differences were considered significant with p < 0.05
RESULTS
Among the 660 women recruited into the study 25 (3.78%) could not be included in the analysis because of missing values. Of the remaining 635 women, 75 (11.81%) women were receiving antihypertensive medication in pregnancy, and were also excluded. Table 1 show characteristics of the women and babies in the study.
The mean 24-h diastolic blood pressure on 635 women examined has shown a range of 52.8 - 95 mmHg (Mean ± DS: 69.9 ± 8.08; Median: 69), the mean 24-h systolic has range between 89-142 mmHg (Mean ± DS 114,8 ± 10,0; Median: 114).
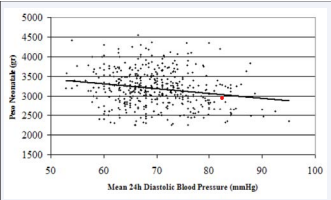
We have found a significant association between birth weight in grams and diastolic ambulatory blood pressure measurements for millimetre of mercury pressure in correlation analysis (Figure 1).
Figure 1
An increase in ambulatory diastolic blood pressure measurement of 1 mmHg was associated with a decrease in birth weigh of 6 gms, the gradient was -10,274 (p < 0.05; 95% IC -22.3 to -3.9).
The association between ambulatory blood pressure and others maternal or fetal indexes were not significant.
Table 1: show characteristics of the women and babies in the study.
| Gestational Hypertension | n = 635 |
| Maternal age (yrs) | 30.4 ± 3.2 |
| Parity | 1.22 ± 0.21 |
| Gestational age at delivery (wks) | 39.8 ± 1.1 |
| Birthweight (gms) | 2938 ± 123 |
| % of smoking | 26 |
| Placental Weight (gms) | 487.1 ± 121.3 |
CONCLUSION
The placenta is a perfusion-dependent organ and that impaired cardiovascular function may cause placental dysfunction and birthweight correlate to hypertension and other cardiovascular risk factors in adult life.
Fetal growth is subject to genetic variation but the intrauterine environment also exerts a dominant influence. Preeclampsia is known to cause fetal growth restriction [2,18]. This is believed to be due to shallow invasion by fetal trophoblasts in maternal spiral arteries in early pregnancy, which may cause occlusion of the vessels [19,20]. Intrauterine growth restriction and preeclampsia are closely linked with abnormal placentation. Reduced uteroplacental perfusion has been shown to induce a rise in maternal blood pressure through increased production of vasoconstrictive agents [21-23].
There are reports that hypertension of pregnancy is a compensatory mechanism to ensure an adequate blood supply to the placenta when the physiological changes fail [24], other Authors described that maternal hypertension cause a placental damage, there is also a demonstration that treatment-induced falls in maternal blood pressure may adversely affect fetal growth [25] and ß-blockers and atenolol is associated with an increase in fetal growth restriction. The vascular pathogenesis of FGR and their relationship with maternal blood pressure [26], has an interesting clinical relevance.
Ambulatory blood pressure monitoring (ABPM) has been used in pregnancy for just over a quarter of a century now and is generally accepted in many countries [27]. ABPM is a better predictor than conventional blood pressure (BP) for the development of preeclampsia and adverse pregnancy outcome [28,29]. Has been demonstrated that the ABPM can identify women’s at risk of hypertension in pregnancy as early as in the first trimester of pregnancy, before the clinical diagnosis of gestational hypertension or preeclampsia takes place for the women investigated [30].
In our study only the maternal diastolic blood pressure seems to be related to fetal growth by birthweight. Steer et al. reported an increase in fetal and neonatal death rate associated with low diastolic BP during pregnancy [31]. Waugh et al, reported that fetal growth is affected when the diastolic BP is above 90 or below 65 mmHg [32], on the other hand an extremely low blood pressure is associated with lower birth weight [33].
In conclusion, even though the datum of 6 Gms for 1 mmHg of diastolic BP may be considered “artificial”, the interesting implication of our hypothesis is that the beginning of maternal hypertension may influence birthweight depending on the gestational age and, therefore, depending on the fetal growth rhythm, in every period of pregnancy.
REFERENCES
1. HMSO. Report on confidential enquiries into maternal deaths in the U.K. 1988-1990. Department of Health. London. 1994.
3. Roberts JM. Endothelial dysfunction in preeclampsia. Semin Reprod Endocrinol. 1998; 16: 5-15.