Transplant Renal Artery Stenosis: An Overlooked Cause of Resistant Hypertension in a New Kidney
- 1. Department of Internal Medicine, Oakland University William Beaumont School of Medicine, USA
- 2. Department of Medicine, Siriraj Hospital, Mahidol University, Thailand
- 3. Department of Medicine, University of Hawaii John A. Burns School of Medicine, USA
- 4. Department of Medicine, Northwestern University Feinberg School of Medicine, USA
Abstract
Uncontrolled hypertension is very prevalent even after successful kidney transplantation and may lead to unfavorable renal allograft and patient outcomes. Several factors pre- and post-transplant as well as surgical and non-surgical factors may contribute to post-transplant hypertension. Transplant renal artery stenosis (TRAS) is one of the treatable causes of resistant hypertension. In addition to the common risk factors for renal artery stenosis in non-transplant patients, immunological and surgical factors are potential contributor’s involved in the pathogenesis of TRAS. Imaging modalities, especially color-Doppler ultrasound, that are non-invasive and widely available are the screening method of choice for diagnosis of TRAS. Understanding the pathogenesis of TRAS could lead to prevention, early detection, and treatment strategies to prolong renal allograft and patient survival.
Keywords
• Cardiovascular disease
• Color-Doppler ultrasonography
• Renal artery stenosis
• Resistant hypertension
• Transplant renal artery stenosis
Citation
Tantisattamo E, Ratanasrimetha P, Spanuchart I, Shrivastava P, Samarapungavan D, Gallon L (2015) Transplant Renal Artery Stenosis: An Overlooked Cause of Resistant Hypertension in a New Kidney. Ann Clin Exp Hypertension 3(2): 1030.
ABBREVIATIONS
ACEs: Angiotensin-Converting Enzyme Inhibitors; AI: Acceleration Index; ARBs: Angiotensin II Receptor Blockers; AT: Acceleration Time; AVF: Arterio Venous Fistula; CCBs: Calcium-Channel Blockers; CDUS: Color Doppler Ultra sound; CIN: Contrast-Induced Nephropathy; CKD: Chronic Kidney Disease; CNIs: Calcineurin Inhibitors; CO2 : Carbon dioxide; Cr: Creatinine; CSN: Canadian Society of Nephrology; CTA: Computed Tomography Angiography; CVD: Cardio Vascular Disease; DDRT: Deceased Donor Renal Transplantation; DES: Drug-Eluting Stent; DGF: Delayed Graft Function; EBPG: European Best Practice Guidelines; ESRD: End-stage Renal Disease; GFR: Glomerular Filtration Rate; K+ : Potassium; KDIGO: Kidney Disease: Improving Global Outcomes; K/DOQI: Kidney Disease Outcomes Quality Initiative; LDRT: Living Donor Renal Transplantation; MRA: Magnetic Resonance Arteriography; NSF: Nephrogenic Systemic Fibrosis; PSV: Peak Systolic Velocity; PTA: Percutaneous Transluminal RenalArtery angioplasty; RAR: Renal/aortic Ratio; RAS: Renal Artery Stenosis; RI: Resistive Index; RIR: Renal/iliac Ratio; SGF: Slow Graft Function; TRAS: Transplant Renal Artery Stenosis; UPCR: Urine Total Protein to Creatinine Ratio
INTRODUCTION
Kidney transplantation is the treatment of choice for endstage renal disease (ESRD) patients [1]. It improves patient survival and quality of life. The initial barrier to maintaining renal allograft survival is primarily immunologic, specifically acute rejection. Since the introduction of calcineurin inhibitors (CNIs) in 1980, early renal allograft survival has been tremendously improved; however, long-term renal allograft outcomes have not changed significantly [2,3]. This leads to more focus on the non-immunologic causes of renal allograft dysfunction or loss. Uncontrolled hypertension remains one of the most important non-immunological causes of renal allograft dysfunction and diminished patient survival. In this review, we discuss general aspects of post-transplant hypertension with emphasis on transplant renal artery stenosis (TRAS).
Post-transplant hypertension
Cardiovascular complications during the post-transplant period are among the most common causes of death with a functioning allograft (DWFG) in kidney transplant recipients [4,5]. As cardiovascular disease (CVD) is a systemic condition and involves almost all vascular beds in the vital organs, including the cerebral, coronary, and renal circulations, controlling and modifying cardiovascular risk factors is one of the main strategies to prevent multisystem organ dysfunction including renal allograft loss.
The majority of kidney transplant recipients have multiple traditional risk factors for CVD such as diabetes mellitus, hypertension, and hyperlipidemia [6]. These risk factors remain after transplant and continue affecting the involved vessels. Similar to chronic kidney disease (CKD) patients, kidney transplant recipients encounter ongoing or even new onset hypertension and its complications.
Epidemiology and risk factors for post-transplant hypertension
Uncontrolled hypertension is a very common nonimmunological co-morbid condition in kidney transplant recipients with a prevalence of more than 80% [7-9]. Risk factors associated with post-transplant hypertension include: deceaseddonor renal transplantallografts (particularly those from a donor with a family history of hypertension), chronic renal allograft dysfunction, presence of native kidneys, use of CNIs (cyclosporine and tacrolimus) or glucocorticoids, weight gain, and renal artery stenosis (RAS) [10-15].
Kidney dysfunction can be responsible for the development of hypertension. Evidence from one study demonstrated that transplantation with kidneys from normotensive donors into recipients with ESRD secondary to essential hypertension could correct hypertension in the kidney transplant recipients [16].
In addition to the condition of donor organs, genetic risk factors play a role in post-transplant hypertension. One study showed that kidney transplant recipients with normotensive families who received kidneys from donors with a family history of hypertension had less withdrawal from and more introductions of antihypertensive medications than recipients receiving kidneys from donors without a family history of hypertension. Moreover, in order to achieve similar blood pressure control, kidney transplant recipients without a family history of hypertension receiving kidneys from donors with hypertension demonstrated a tenfold greater increase in a requirement for antihypertensive therapy than the recipients who received kidneys from donors without hypertension [17].
Apart from genetic factors, several associated risk factors for post-transplant hypertension can contribute to the development of hypertension at different time points post-transplant, which is generally divided into 3 periods: immediate, early, and late post-transplant (Table 1) [18-27].During the immediate posttransplant period (the first 3 months post-transplantation), surgical-related factors such as postoperative pain or hypervolemic status resulting from high volume intra operative fluid administration are the major causes of hypertension. In addition, the majority of ESRD patients have underlying hypertension requiring multiple blood pressure medications. Discontinuation of antihypertensive medications, especially clonidine, during the perioperative period often leads to rebound hypertension and blood pressure medications may need to be restarted during the immediate post-transplant period. High dose intravenous glucocorticoids as a part of an immunosuppressive regimen could contribute to hypertension, but are generally not the main factor as intravenous glucocorticoids are typically restricted to the first 3 post-transplant days. Renal allograft dysfunction may become an important cause of uncontrolled hypertension during this period, especially in the setting of deceased donor renal transplantation (DDRT) with a higher incidence of slow graft function (SGF) or delayed graft function (DGF) than in living donor renal transplantation (LDRT). This is a common scenario where diuretics may not be effective and posttransplant dialysis may be required to control volume status as well as blood pressure.
Immunological factors causing renal allograft dysfunction start to play an important role in hypertension during the early post-transplant period (3 – 12 months post-transplantation). Acute renal allograft dysfunction from acute rejection and acute CNIs nephrotoxicity are the common causes.
Similar to the early post-transplant period, renal allograft dysfunction during the late post-transplant period (> 1 year posttransplantation) may cause uncontrolled hypertension. Chronic CNIs nephrotoxicity is one of the most common causes of chronic renal allograft dysfunction and subsequent chronic kidney disease in kidney transplant recipients. Recurrent native kidney disease and complicated urological problems may contribute to hypertension.
Renovascular hypertension, specifically TRAS, is usually suspected as a cause of uncontrolled or new-onset hypertension after the immediate post-transplant period, especially when ultrasound with color-Doppler (CDUS) demonstrates some evidences of stenosis in the transplant renal arteries, external iliac artery, or at the anastomotic site. In addition, CDUS performed for other reason such as acute renal allograft dysfunction may incidentally detect TRAS.
Pathogenesis of post-transplant hypertension
The pathogenesis of hypertension during the post-transplant period is likely multi factorial and could result from several risk factors, given the potential for complex underlying medical and surgical sources as well as immunological causes (Table 1) [18- 27]. The majority of these factors are reversible and some are preventable. In this review, we discuss on TRAS, one of the most important causes of reversible resistant hypertension.
TRANSPLANT RENAL ARTERY STENOSIS (TRAS)
Epidemiology and risk factors for TRAS
The incidence of TRAS is unclear. A wide range of incidence from 1% to 23% has been reported in different studies, partly due to variations in definitions and the methods used to diagnose TRAS [28]. The onset of TRAS can occur at anytime posttransplant, but it is commonly diagnosed between 3 months and 2 years post-transplant [29]. Several medical and surgical-related risk factors have been associated with TRAS (Table 2) [15,30-32].
Medical risk factors for renal artery stenosis in kidney transplant recipients are similar to those that occur in non-transplant patients. Atherosclerotic disease remains the most common cause of TRAS and vascular lesions are usually found in the anastomotic vessels of the recipients who have underlying atherosclerotic risk factors. Atherosclerotic plaques in the donor renal arteries and aorta can be detected during organ procurement. These plaques are graded as mild, moderate, or severe and also scored as soft or hard plaques. Donor kidney organs with moderate to severe and hard arterial plaques can potentially cause complications or difficulty during the anastomosis and these organs are usually discarded. Therefore, atherosclerotic disease causing TRAS usually arises from the recipient iliac arteries. Conflicting transplant-related risk factor data have been reported. Recent studies suggest that cytomegalovirus (CMV) infection and DGF are independent risk factors for TRAS, possibly by causing endothelial dysfunction [15].
Surgical risk factors involve the interplay between donor, recipient- and other surgical-related factors. Since the anastomotic site is the most common location of TRAS, surgical trauma during harvesting kidney organs, traumatic clamping of the recipient external iliac artery, or suturing the donor renal arteries to the recipient artery are the major causes of early posttransplant TRAS.
Pathogenesis of TRAS
Similar to the non-transplant population, common traditional risk factors of CVD lead to unfavorable effects on blood vessels in the majority of kidney transplant recipients [6]. The renal artery is often one of the major affected vessels, leading to worsening renal allograft function if the change in vessel structure subsequently causes RAS. The pathogenesis of RAS in renal transplant recipients may differ from non-transplant patients due to surgical factors including donor renal vascular manipulation or reconstruction in the preparation of renal vessels for anastomosis to recipient vessels [28,29,33], as well as immunological factors from exposure to immunosuppressive medications that may potentially cause endothelial damage [15,30-32] (Table 2).
Pathologic lesions of TRAS
In the non-transplant population, several renovascular pathologies can lead to RAS including atherosclerosis, fibromuscular dysplasia (FMD), aortic dissection, abdominal aortic coarctation, vasculitides (polyarteritis nodosa, Takayasu arteritis, radiation), neurofibromatosis type 1, and segmental arterial mediolysis [30]. In kidney transplant recipients, any arteries involved in the anastomosis, including donor and recipient arteries, could be involved in physiological stenosis [34].
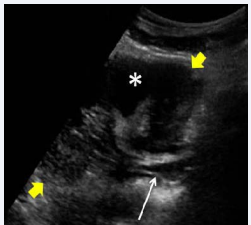
Figure 1 Longitudinal gray scale sonographic scan of the right lower quadrant of a transplanted renal allograft (yellow arrows) shows a dissection flap in the recipient distal external iliac artery adjacent to the anastomotic site of the donor renal artery (white arrow). The dissection flap caused physiologic stenosis and compromised blood flow from the recipient external iliac artery to the donor renal artery
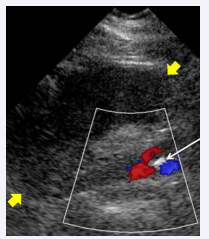
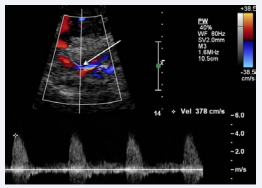
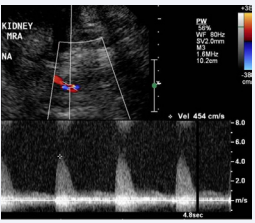
In the experience of the authors, a case was noted where fragile intraluminal tissue in the recipient external iliac artery adjacent to the anastomotic site of the donor renal artery resulted in an intraluminal flap and subsequent stenosis that compromised blood flow from the recipient external iliac artery to the donor renal artery (Figure 1). CDUS in this patient revealed an elevated peak systolic velocity (PSV) at the anastomosis of 454 cm/sec. The PSV in the native right external iliac artery proximal and distal to the anastomosis were 13.9 and 27.8 cm/sec, respectively. Distal to the anastomotic site, the PSVs in the hilar portion and mid-portion of the main renal artery were 86 and 82 cm/sec, respectively. The high PSV at the anastomosis supported physiological stenosis. The resistive index (RI) in the superior, mid, and inferior portions were all normal at 0.50, 0.63, and 0.63, respectively (Figures 2-4).
Figure 2 Longitudinal color-Doppler sonographics can of the right lower quadrant of the transplant renal allograft (yellow arrows) shows bidirectional flow above and below the dissection flap (white arrow).
Clinical manifestation of TRAS
Renovascular hypertension is one of the most common causes of resistant hypertension in the non-transplant population. However, kidney transplant recipients with TRAS may present with clinical manifestations that are different from nontransplant patients. Presentation could include typical resistant hypertension, renal allograft dysfunction from ischemic renal allograft nephropathy, or even asymptomatic RAS incidentallydetected during abdominal/pelvic imaging [30]. The first two presentations are most common [35]. Other manifestations include an acute elevation in blood pressure or flash pulmonary edema [36]. Similar to the non-transplant population, a reversible reduction in glomerular filtration rate (GFR) from angiotensinconverting enzyme inhibitors(ACEs) or angiotensin II receptor blockers (ARBs) are clues suggesting TRAS [29,37].
Figure 3 Spectral Doppler image shows an elevated peak systolic velocity within the true lumen (white arrow) near the dissection flap, reflecting reduced lumen diameter.
Screening and diagnosis of TRAS
Since the prevalence of RAS is much higher in patients with clinical presentations suggesting some evidence or characteristic of renovascular hypertension, such as hypertension in the young, abdominal bruits on physical exam, malignant hypertension, hypokalemia, recurrent acute decompensated heart failure, or flash pulmonary edema, screening for RAS in hypertensive patients without these clinical presentations is recommended only after other secondary causes of hypertension are excluded [38,39].The typical scenario that should lead to evaluation for TRAS include uncontrolled hypertension with antihypertensive agents, hypertensive patients with audible bruits over the renal allograft or with unexplained renal allograft dysfunction. Isolated moderate to severe hypertension is not a significant clinical indicator by itself for evaluation for TRAS [40].
Figure 4 Spectral Doppler image of the main renal artery distal to the dissection flap shows an elevated peak systolic velocity of up to 454 cm/second.
Renal artery angiography remains the gold standard for the diagnosis of TRAS and can detect other lesions that may mimic clinical presentations of TRAS such as intrarenal arteriovenous fistula (AVF), a common complication causing an acute rise in serum creatinine after transplant renal biopsy. In addition, vascular interventions with renal artery balloon angioplasty with/without renal artery stenting can be performed at the same time if stenotic lesions amenable to treatment are detected. However, renal artery angiography is an invasive procedure with rare but potentially significant complications such as contrastinduced nephropathy (CIN), arterial dissection, or cholesterol embolism [30]. To minimize iodinated iso-osmolar contrast material use during transplant renal artery angiography, our institute routinely uses carbon dioxide (CO2 ) angioplasty as an alternative non-nephrotoxic contrast agent. Due to the invasive nature of renal artery angiography, imaging modalities especially CDUS, magnetic resonance arteriography (MRA), and computed tomography angiography (CTA) are increasingly performed as initial studies to screen and diagnose TRAS [29,32].
Imaging studies that can identify the stenotic sites, localize the main renal artery and its branches, measure hemodynamics of the arteries, and determine other related pathology such as abdominal aortic aneurysm or mass seem to be the ideal investigational tools for screening for RAS [30]. Table 3 summarizes imaging modalities utilized to screen and/ or diagnose TRAS [32, 34, 41-45]. In this review, we will focus on CDUS since this imaging modality meets the criteria of ideal investigational tools above.
Color-Doppler ultrasound (CDUS)
Among the imaging techniques used to screen for RAS, CDUS is widely utilized as an initial screening tool since it is non-invasive, reproducible, and inexpensive. However, the accuracy varies depending on the skill of the ultrasonographer. In addition, given variations in transplant renal artery anatomy, the information from CDUS needs to be interpreted with caution.
In non-transplant patients, two pieces of information commonly used to determine the degree of RAS are PSV and RI. The normal PSV in the main renal artery and its branches is < 120 cm/second [46]. RI is a parameter calculated by the formula: {(PSV – End-diastolic velocity) / PSV} and indicates the degree of intrarenal arterial impedance. It is variable per the patient age and area of measurement. Average RI values from different areas of the renal artery are shown in (Table 4) [46-52].
To diagnose RAS by CDUS, there are main diagnostic criteria used to evaluate evidences of artery stenosis.
1) Proximal criteria:These criteria directly evaluate the stenotic area and diagnose proximal stenosis of the renal artery (Table 5) [53-60].
1. PSV
2. Velocity gradient between stenotic and prestenotic segments
3. Renal artery Doppler signal
4. Color artifacts and turbulence
Among of these, the abnormalities detected in criteria 3 and 4 are the immediate and first signs of RAS.
2) Distal criteria: These criteria are used to indirectlyevaluate the stenotic area by detecting the alteration of flow at the renal vasculature distal to the site of stenosis (Table 5) [53-60].
A discrepancy of RI between 2 kidneys is another criterion that has been used to diagnose RAS, but this is uncommonly used in clinical practice and is not relevant to kidney transplant recipients with a single functioning renal allograft [61-63].
Spiral computed tomography (CT) scan
A spiral (helical) CT scan with intravenous contrast (CT angiography or CTA) is diagnostic study with a high accuracy for detecting renal artery stenosis from atherosclerotic disease. It is not as accurate for the detection of fibromuscular dysplasia because the nature of fibromuscularinvolvement in the distal arterial segment causes difficulty in the visualization of stenosis [64-66]. Even though CTA is a noninvasive test, it could potentially cause CIN especially in patients with renal impairment. There is no data to evaluate its use in kidney transplant patients [32,43].
Magnetic resonance angiography (MRA)
MRA is another noninvasive study commonly performed to screen for renal artery stenosis. Similar to CTA, MRA is associated with the study-related complication nephrogenic systemic fibrosis (NSF) from gadolinium exposure, especially in patients with renal dysfunction. Gadolinium should be avoided in the patient with eGFR< 30 mL/min. However, due to a very high sensitivity and a specificity of up to 100% in one study, MRA may be the preferred screening imaging in patients with very high suspicion for renal artery stenosis, even before CDUS [44].
Radioisotope renography
This modality is rarely used to screen for or diagnose renal artery stenosis. It is more useful for detecting the physiologic significance of a moderately severe stenosis. A negative result may predict unresponsiveness to treatment [45,67].
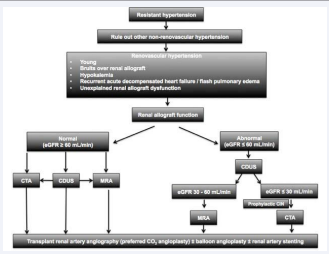
Since the above screening and diagnostic imaging studies are not risk-free, especially in a patient with impaired renal allograft function, we suggest an algorithm to screen and diagnose for TRAS in kidney transplant recipients (Figure 5). As mentioned above, causes of non-renovascular hypertension should first be excluded in patients with resistant hypertension. Kidney transplant recipients with clinical symptoms or signs of renovascular hypertension requiring further investigation should be divided into 2 groups: patients with normal and abnormal renal allograft function. In patients with normal renal allograft function, CDUS, CTA, or MRA may be performed. CDUS is the most common initial imaging study and is usually followed by CTA or MRA and finally renal artery angiography with / without interventions. In patients with renal allograft dysfunction, CDUS should be the first screening study, followed by either CTA or MRA depending on the degree of renal allograft dysfunction. Since NSF is one of the serious complications of gadolinium, MRA should be avoid in the patient with eGFR< 30 ml/min and CTA may be considered with prophylaxis for CIN.
Figure 5 Suggested algorithm for screening and diagnosis of transplant renal artery stenosis.
Management of TRAS
Similarly as in non-transplant patients, treatment for TRAS includes medical and non-medical intervention: either percutaneous transluminal renal artery angioplasty (PTA) with or without stenting, or surgery.
Table 1: Common risk factors contributing to hypertension during different post-kidney transplant periods [18-27].
| Post-transplant period | Risk factors | Pathogenesis | Comments |
|
Immediate
|
Genetic predisposition Volume overload
Surgical procedure
Renal allograft dysfunction
Glucocorticoids |
Unknown Intraoperative volume management Ischemia Salt and water retention |
Treatment by volume removal including diuretics and/or dialysis especially in DGF Increased systemic and renal vascular resistance especially in the afferent arteriole |
|
Early
|
Genetic predisposition Acute renal allograft dysfunction CNI nephrotoxicity TRAS |
Unknown Medical and/or Surgical risk factors |
|
|
Late
|
Genetic predisposition Recurrent native renal diseases Urinary tract obstruction Chronic renal allograft dysfunction Failed prior renal allograft Hypo perfused end-stage native kidneys CNIs Glucocorticoids TRAS |
Unknown
|
|
| Abbreviations: CNIs: Calcineurin Inhibitors; DGF: Delayed Graft Function; TRAS: Transplant Renal Artery Stenosis. | |||
Table 2: Risk factors associated with transplant renal artery stenosis [15, 30-32].
| Risk factors | |
|
Medical
|
Traditional risk factors Transplant/Immunological related risk factors [15,31,32] |
|
Surgical
|
Donor-related Recipient-related Surgical-related |
| Abbreviations: DCD: Donation after Cardiac Death | |
Table 3: Imaging modalities utilized to screen and/or diagnose TRAS [32,34,41-45].
| Imaging Modality | Sensitivity | Specificity | Limitations/ Complications / Contraindications |
| Color-Doppler ultrasonography | 58-100% [34] (100% with PSV >2.5 m/second) [41] |
87-100% [34] (100% with PSV >2.5 m/second [41] |
Commonly used for screening[32,34,41,42]; but operator-dependent |
| Spiral CT angiography (CTA) | Data in non-transplanted kidneys [32,43] | Noninvasive | |
| Magnetic resonance angiography (MRA) | 100% with gadolinium-enhanced MRA and three-dimensional phase contrast post-gadolinium [44] | Nephrogenic systemic fibrosis especially when GFR < 30 ml/min | |
| Renal artery angiography | Gold standard | Invasive | |
| Radioisotope renography | Not sensitive in patients with a history very suggestive for TRAS [45, 67] | Useful for predicting the physiologic significance of a moderately severe stenotic lesion | Negative renogramunlikely to respond to correction of the stenosis [67] |
| Abbreviations: GFR: Glomerular Filtration Rate; PSV: Peak Systolic Velocity; TRAS: Transplant Renal Artery Stenosis | |||
Table 4: Normal resistive index measured by color-Doppler ultrasound in different areas of the renal artery [46-52].
| Arterial site and utility | RI | Comments |
| Renal artery (hilar region) | 0.65 +/- 0.17 | |
| Interlobar artery | 0.54 +/- 0.20 | |
| Discriminating value between normal and pathologic resistance | 0.7 | The large arterial segment of interlobar arteries producing the best signals toward the transducer probe is the optimal areas for evaluation [46,47,49]. Peripheral or arcuate arteries with weak signals should not be used [50,51] |
| Not recommend for renal artery stenting | > 0.8 [52] | |
| Abbreviations: RI: Resistive Index | ||
Table 5: Color-Doppler ultrasound criteria for diagnosis of renal artery stenosis in non-transplanted and transplanted kidneys [53-60].
| CDUS criteria | Abnormal value of the CDUS criteria | ||
| Native kidney | Transplanted kidney | ||
| 1. Proximal criteria | 1.1PSV (the first and most important sign) | > 180 cm/sec | > 250 cm/sec |
| 1.2 Velocity gradient between stenotic and prestenotic segments > 2:1 (PSV ratio of the renal artery to the pre renal artery) | RAR (PSV ratio of the renal artery to the pre renal abdominal aorta in native kidney)> 3.5 | RIR (PSV ratio of the donor renal artery to the pre renal recipient iliac artery in transplant kidney)> 3.5 | |
| *1.3Renal artery Doppler signal [55] | No signal if occlusion | ||
| *1.4 Color artifacts and turbulence [55] | Significant upstream stenosis | ||
| 2. Indirect criteria | Tardus-parvus [56] | Flow at the renal hilum downstream of a significant stenosis is damped and slowly rises to the peak. AT > 0.07 seconds and AI < 3 m/s2 | |
| Abbreviations: AI: Acceleration Index; AT: Acceleration Time; PSV: Peak Systolic Velocity; RAR: Renal/aortic Ratio; RAS: Renal Artery Stenosis; RIR: Renal/iliac Ratio *The immediate and first signs of RAS [55] |
|||
Table 6: Recommended blood pressure goals in kidney transplant recipients from different guidelines [69-72].
| Comorbid condition | Medical society guideline | Goal blood pressure (mmHg) |
| Non-proteinuric | CSN | < 140/90 [69] |
| K/DOQI and KDIGO | < 130/80 [70, 71] | |
| Proteinuric (spot UPCR 500 to 1000 mg/g of Cr) | < 130/80 | |
| EBPG | 125/75 [72] | |
| Abbreviations: Cr: Creatinine; CSN: Canadian Society of Nephrology; EBPG: European Best Practice Guidelines; KDIGO: Kidney Disease Improving Global Outcomes; K/DOQI: Kidney Disease Outcomes Quality Initiative; UPCR: Urine Total Protein to Creatinine Ratio | ||
Table 7: Suggested antihypertensive medications for kidney transplant recipients [12,13].
| Recipients with | Antihypertensive medications | Pros | Cons | Comments |
| CNIs | CCBs | Preferred antihypertensive agents [12, 13] Decreases CNIs dose used Decreases renal allograft loss Increases GFR | ||
| ACEIs | Decreases proteinuria | Decreased GFR interferes with interpretation of renal allograft function Hyperkalemia (decreases urinary K+ excretion by CNI and decreases angiotensin II production and subsequent aldosterone secretion by ACEIs/ARBs) Decreases hemoglobin |
Wait 3-6 month posttransplant to initiate ACEIs/ARBs
|
|
| ARBs | Decreases serum uric acid Decreases proteinuria | |||
| Non-CNI | CCBs ACEIs/ARBs β-blockers Diuretics |
|||
| Abbreviations: ACEIs: Angiotensin-Converting Enzyme Inhibitors; ARBs: Angiotensin Receptor Blockers; CCBs: Calcium-Channel Blockers; CNIs: Calcineurin Inhibitors; GFR: Glomerular Filtration Rate; K+ : Potassium | ||||
MEDICAL MANAGEMENT
Blood pressure control
TRAS with stable renal allograft function and no hemodynamically significant stenosis can be medically managed to control blood pressure [29]. Different medical societies have developed different blood pressure goals depending on the presence or absence of proteinuria and/or comorbid conditions, such as diabetes mellitus or atherosclerotic cardiovascular disease [9, 68]. (Table 6) [69-72].
Since CNIs are most commonly used as the backbone of immunosuppressive medication for kidney transplantation, interactions with these drugs should be considered in managing antihypertensive medications. Suggested antihypertensive medications for patients with and without concomitant CNIs use are shown in the Table 7 [12,13].
Non-dihydro pyridine calcium channel blockers are one of the preferred antihypertensive medication classes in kidney transplant recipients with CNIs. The CYP4503A4 enzyme inhibitory effect leads to increased CNIs level and allows a minimized dose of CNIs. In addition, the use of calcium channel blockers has been associated with a decreased incidence of renal allograft loss and increased GFR [12,13].
Since TRAS causes renal allograft hypo perfusion and subsequent activation of the renin-angiotensin-aldosterone system (RAAS) and impaired sodium excretion, angiotensinconverting enzyme inhibitors and angiotensin-receptor blockers (ACEIs/ARBs) should be effective in the control of blood pressure in patients with TRAS. However, ACEIs/ARBs are not commonly used, especially in the immediate or even early post-transplant periods. ACEIs/ARBs are a known cause of increased serum creatinine. Even though this is a physiologic effect of ACEIs/ARBs and a decrease in GFR < 30% of the baseline is an acceptable physiological threshold, this effect could interfere with an interpretation of renal allograft function especially in kidney transplant recipients who are sensitive to volume depletion during the immediate post-transplant period. In addition, the hyperkalemic side effects of ACEIs/ARBs could be additive to that caused by CNIs. Even though these are unfavorable side effects, the antiproteinuric effects of ACEIs/ARBs are beneficial and ACEIs/ARBs remain a commonly used antihypertensive medication in early or late post-transplant periods when kidney transplant recipients have established baseline renal allograft function. This period is also the time when TRAS commonly occurs, and ACEIs/ARBs remain useful as antihypertensive agents as long as there is no acute renal allograft dysfunction. Another potential beneficial effect of ACEIs/ARBs is the treatment of posttransplant erythrocytosis. The mechanism is unclear but likely related to inhibition of erythropoiesis.
For kidney transplant recipients who do not take CNIs, effective control of blood pressure may be achieved using CCBs, ACEIs/ARBs, β-blockers, or diuretics. Mechanisms contributing to hypertension and the specific benefit and side effect profiles should be taken into consideration when selecting any of these antihypertensive agents. In addition to blood pressure control, conservative management indicates that dyslipidemia should be treated with statins even though there is no clear data in kidney transplant recipients [29].
NON-MEDICAL INTERVENTION
Percutaneous transluminal renal artery angioplasty (PTA)
Medical management generally controls blood pressure in patients with TRAS; however, non-medical treatment such as PTA and/or stenting may be indicated especially in resistant hypertension without response to antihypertensive medications and progressive decline in renal allograft function.
The success rate of PTA is up to 80% and the overall rate of restenosis is 20% [73,74]. Short, linear stenotic lesions that are distal from the anastomosis have the highest chance of success[29].Conversely, renal artery anatomy with arterial kinking, anastomotic strictures, and long lesions have a higher risk of unsuccessful intervention and complications [28,75,76].
The recurrence rate for stenosis with PTA alone is 10 – 33% in 6 – 8 months [77];this reduces to < 10% with combined PTA and renal artery stenting [78], making this intervention very useful for patients with recurrent stenosis [79,80]. Restenosis may be further prevented by using radioactive or drug-eluting stents (DES). These stents locally release antiproliferative agents such as rapamicin and enoxaparin, inhibiting intimal hyperplasia [81-84]. However, unlike the efficacy of DES in coronary arteries, data regarding the use of DES in the renal artery in transplant is limited [85].From our experiences, similarly to the nontransplant patient population, PTA with/without renal-artery stenting may not significantly improve renal allograft function or blood pressure control in kidney transplant recipients (unpublished data) [86,87].
Surgery
Surgical intervention for TRAS is uncommon, especially when extensive fibrosis and scarring around the transplanted kidney may make surgical correction of a transplant artery stenosis difficult. Surgical correction is considered in patients with proximal recipient arteriosclerotic disease, stenosis at the anastomosis line, or resistant hypertension [76,88]. The rates of success and recurrent stenosis are 60 -90% and 10%, respectively [28].
Outcomes of post-transplant hypertension
Similarly to the non-transplant population, persistent hypertension and wide pulse pressure could lead to several complications both related and non-related to transplantation.
Transplant-related outcomes of post-transplant hypertension
Hypertensive nephrosclerosis can occur or recur in kidney transplant allografts. Hypertension during the post-transplant period shortens renal allograft survival times and post-transplant blood pressure inversely relates to the GFR of the renal allograft [9].
Non-transplant related outcomes of post-transplant hypertension
Approximately half of late renal allograft loss is due to DWFG [89],and CVD is the major cause of mortality in kidney transplant recipients. As is also true of the general population, post-transplant hypertension is still among the most important traditional risk factors for CVD. Chronic uncontrolled hypertension can result in left ventricular hypertrophy, which is an independent risk factor for heart failure and death in kidney transplant recipients [10,90- 93].
CONCLUSION
Even though post-transplant hypertension is very common and has a complex pathogenesis, with medical and surgical as well as transplant-related (immunological) and transplant-unrelated risk factors, the majority of these factors are treatable. TRAS is considered a rare but recognized cause of resistant hypertension during the post-transplant period; however, the incidence may be underestimated. For patients with a typical presentation of especially resistant hypertension and unexplained renal allograft dysfunction, recognition and investigation of TRAS could increase the opportunity for early diagnosis of this underrecognized, threatening, but curable disease in order to preserve renal allograft and patient survival.
ACKNOWLEDGEMENTS
The authors would like to thank Anna Pawlowski and Eric Stanczyk from Northwestern Medicine Enterprise Data Warehouse (NMEDW), Northwestern University Feinberg School of Medicine for data analysis and Dr. Monzer Chehab from the Department of Radiology and Molecular Imaging, Oakland University William Beaumont School of Medicine for his assistance in obtaining images. We appreciate Dr. Steven Cohn, Dr. Vandad Raofi, and Dr. Damanpreet S. Bedi from Multi-Organ Transplant Center, Department of Surgery, Oakland University William Beaumont School of Medicine for their inputon surgical aspects. We would also like to thank Ms. Rose Callahan fromthe Department of Surgery, Beaumont Hospital – Royal Oakfor review of the manuscript. We also appreciate grant support for data management from the Northwestern Medicine Enterprise Data Warehouse (NMEDW) Pilot Data Program, Northwestern University Feinberg School of Medicine.
REFERENCES
1. Suthanthiran M, Strom TB. Renal transplantation. N Engl J Med. 1994; 331: 365-376.
9. Mangray M, Vella JP. Hypertension after kidney transplant. Am J Kidney Dis. 2011; 57: 331-341.
11. Sayegh MH, Lazarus JM. Renal parenchymal disease and hypertension. In: Cooke JP, Frohlich ED, editors. Current Management of Hypertension and Vascular Disease. Philadelphia: Decker. 1992; 76.
23. Watschinger B, Sayegh MH. Endothelin in organ transplantation. Am J Kidney Dis. 1996; 27: 151-161.
35. Luke RG, Curtis J. Biology and treatment of transplant hypertension. In: Laragh JH, Brenner BM, editors. Hypertension Pathophysiology, Diagnosis and Management. New York: Raven Press. 1995; 2471–83.
39. Strandness DE. Doppler and ultrasound methods for diagnosis. Semin Nephrol. 2000; 20: 445-449.
43. Rubin GD. Spiral (helical) CT of the renal vasculature. Semin Ultrasound CT MR. 1996; 17: 374-397.
47. Zubarev AV. Ultrasound of renal vessels. Eur Radiol. 2001; 11: 1902- 1915.
51. Lee HY, Grant EG. Sonography in renovascular hypertension. J Ultrasound Med. 2002; 21: 431-441.
58. Tublin ME, Dodd GD 3rd. Sonography of renal transplantation. Radiol Clin North Am. 1995; 33: 447-459.
60. Kim SH. Vascular diseases of the kidney, WB Saunders, Philadelphia, Pa, USA, 2003. In: Kim SH, editor. Radiology Illus- trated. Philadelphia, PA: WB Saunders. 2003; 429–32.
87. Tantisattamo E, Ratanasrimetha P, Pitukweerakul S, Shetty A, Gallon L. Transplant renal artery stenosis: A treatable cause of resistant hypertension and renal allograft dysfunction. North American Artery Fifth Annual Meeting Hemodynamics & Target Organ Damage: Mechanisms, Measurements, Management; September 11-12, 2015; Chicago, Illinois. Abstract# PO-015.2015; 44.