Anti-NMDA Autoimmune Encephalitis due to Ovarian Teratoma: A Pediatric Case Report
- 1. Instituto de Saúde São Lucas, Pato Branco, Paraná, Brasil
- 2. Centro Universitário de Pato Branco, Paraná, Brasil
- 3. Ambulatório municipal de saúde, Pato Branco, Paraná, Brasil
Abstract
Encephalitis is a complex condition characterized by dysfunction in brain tissue resulting from infectious or autoimmune causes. Anti-NMDA receptor encephalitis is especially relevant in children and adolescents, often associated with ovarian teratomas. Diagnosis involves imaging exams, cerebrospinal fluid (CFS) analysis and laboratory tests, although differentiating between autoimmune and infectious causes is still challenging.
Objective: To understand the difficulties of diagnosing autoimmune encephalitis through a case report.
Study design: Case report with authorization from the patient’s guardian.
Results and Conclusion: The clinical case presented illustrates this difficulty, where behavioral and neurological symptoms were accompanied by a suspicion of autoimmune encephalitis, corroborated by an identified ovarian teratoma. Diagnostic confirmation, however, was hampered by the availability and cost of serology for anti-NMDA antibodies. Treatment involves early immunotherapy, especially when combined with surgical removal of the teratoma, resulting in a better prognosis. In the case described, immunotherapy was started quickly with methylprednisone and immunoglobulin associated with the removal of the ovarian teratoma; however, complete clinical improvement occurred after administration of rituximab.
Keywords
• Autoimmune encephalitis
• Ovarian teratoma
• Pediatrics
CITATION
de Carvalho Kuntz R, Forselini ALM, Brandes BV, Desconsi K, Saggin SI, et al. (2024) Anti-NMDA Autoimmune Encephalitis due to Ovarian Teratoma: A Pediatric Case Report. Ann Pediatr Child Health 12(3): 1339.
INTRODUCTION
Autoimmune encephalitis is characterized by acute neurological dysfunction with impairment of the brain parenchyma due to the development of autoantibodies against glutamatergic receptors. The condition, initially described in 2007, used to be correlated with the presence of concomitant neoplasia, such as ovarian and testicular neoplasms. Currently, post-vaccination states and viral infectious processes are also considered predictive factors for the development of autoimmune encephalitis [1].
The clinical picture is based on behavioral changes, movement and sleep disorders, changes in the level of consciousness, focal neurological deficits and status epilepticus, in addition to neuropsychiatric manifestations, such as visual and auditory hallucinations [2].
The diagnosis is made based on clinical criteria that direct suspicion towards autoimmune encephalitis, examinations including non-contrast head tomography and magnetic resonance imaging, electroencephalography and lumbar puncture for CSF evaluation, detecting or not the presence of pathogenic antibodies and cellular changes. Resulting [3]. Finally, treatment is based on early immunotherapy with corticosteroids, intravenous immunoglobulin and plasmapheresis; immunobiologicals are also used for cases refractory to initial treatment [4].
CASE REPORT
Patient, female, previously healthy, without the use of continuous medication, accompanied by her mother in consultation, presented behavioral changes, crying spells, fear, anxiety, hallucinations and difficulty sleeping that started a week ago and worsened in the last three days, without previous infectious symptoms, syncope and release of sphincters.
After a consultation at the Psychosocial Care Center, she started using fluoxetine, but without improvement, being referred to a psychiatric consultation, on suspicion of bipolar disorder, fluoxetine was suspended and risperidone was started. Intramuscular midazolam was also administered due to the psychotic episode and neurological evaluation and magnetic resonance imaging were requested, and the patient was referred to the referral hospital.
During the consultation, the patient presented neurological symptoms, such as slurred speech and left eyelid ptosis and anxiety, but was cooperative during the examination. Routine exams, neurosurgery evaluation and head computed tomography (CT) were requested, without any changes. On neurological examination, good general condition, Glasgow 15, isophotoreactive pupils, no motor deficits. Frisium 10 mg at night and haldol 5 drops were prescribed in case of attacks and a skull magnetic resonance (MRI) was requested.
In the subsequent 24 hours, during CSF collection, an abdominal mass up to the umbilical scar was noted and a bladder catheterization was performed without improvement. Given the suspicion of ovarian teratoma, the patient was referred for abdominal CT and MRI and pulse therapy with methylprednisone 1g every 24 hours/5 days was started due to suspected autoimmune encephalitis. Also using Haldol, risperidone, clobazam, albendazole and ivermectin.
Table 1: Probable anti-NMDA encephalitis
|
Probable anti-NMDA encephalitis Rapid onset (<3 months) with at least 4 symptoms: - Abnormal behavior or cognitive dysfunction - Altered speech - Movement disorders - Altered consciousness - Seizures - Autonomic dysfunction or central hypoventilation. Abnormal exams: altered EEG: extreme delta brush and/or CSF: lymphocytic pleocytosis Exclusion of other causes
|
Prepared by the author (2023)
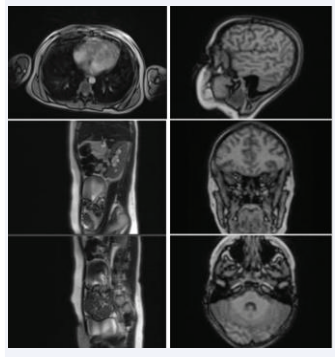
Imaging tests demonstrated a solidocystic pelvic mass compatible with ovarian teratoma and the patient was referred for gynecological consultation. A new lumbar puncture and CSF collection were performed, which indicated significant pleocytosis Leuc 35 Lymph 78% and cranial resonance without significant changes (Figure 1).
Figure 1: MRI abdomen and skull.
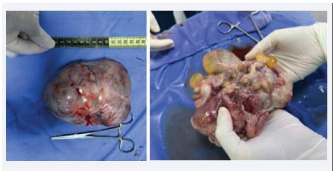
After a gynecological consultation, the patient underwent a left oopherectomy to remove the mass, without complications, being referred to pathology, confirming ovarian teratoma and antibiotic therapy with ceftriaxone was started. After surgery, he presented with chewing movements, staring, movements in the left upper limb and nocturnal agitation, controlled with Diazepam. Electroencephalography was performed which revealed diffuse slowing, prominent delta waves and delta brush impression and anti-NMDA antibody was requested with a subsequent positive result (Figure 2 and Figure 3).
Figure 2: Pre-operative.
Figure 3: Ovarian teratoma.
The patient developed a systemic infectious condition, fever and convulsions and a chest X-ray with a mild diffuse infiltrate. The antibiotic therapy was changed to cefepime, associated with valproic acid to control the crises and risperidone was reduced. Thus, his condition improved and he was discharged from hospital.
She returned for care four days after discharge with an increase in episodes of hallucinations, continuously using Zinat, baclofen, levomepromazine, valproic acid and clonazepam, and was referred to psychiatry for evaluation.
In the following two months, after outpatient follow-up,the patient returned with positive anti-NMDA antibodies and relapses of hallucinations, speech and sleep difficulties and partial improvement in motor skills. After evaluation by the neuroimmunologist, new cycles of immunotherapy with methylprednisone and IV immunoglobulin were performed in both months, with partial improvement, and Rituximab was requested.
After a subsequent return for administration of rituximab, twice, with discharge after infusion, the patient evolved with complete improvement in cognitive and motor symptoms, currently being monitored in a pediatric neurology outpatient clinic.
DISCUSSION
Encephalitis is defined as a dysfunction in the brain parenchyma associated with infectious etiologies and autoimmune processes that lead to behavioral and neurological changes. The disease characteristically presents inflammation in the brain parenchyma, which can be diagnosed histologically based on a brain biopsy compatible with inflammation, edema and neuronophagia. due to acute behavioral and neurological changes [5].
Among the most frequent autoimmune processes, anti-N- methyl-D-aspartate (NMDA) receptor encephalitis is the most common identifiable cause of brain inflammation in childhood [5]. The condition has a higher incidence in the young population, 80% of which are females and affecting children and adolescents twice as much as the adult population [6,7].
The autoimmune process associated with paraneoplastic syndrome results in the production of specific anti-NMDA antibodies against receptors located on the extracellular surface of the NR1 subunit of glutamate. As a consequence, from the blockade of glutamatergic excitatory activity and the inflammatory process with activation of B lymphocytes, plasma cells and microglia, synapses and neuronal functioning are compromised, triggering the neuropsychiatric clinical picture [1].
Furthermore, previous viral infectious conditions, mainly resulting from herpes simplex viruses, are also correlated with the development of the autoimmune process through the formation and release of specific neoantigens to brain cell receptors resulting in acute inflammation of the brain parenchyma [8].
In childhood, the clinical picture consists of neuropsychiatric symptoms with acute or subacute onset in previously healthy children with no family history of psychiatric disorders. Thus, behavioral changes, movement, sleep and speech disorders, as well as visual and auditory hallucinations may be present initially, progressing to recurrent seizures, changes in the level of consciousness and neurological deficits. Therefore, when faced with suspected psychosis in children and adolescents, autoimmune etiologies such as anti-NMDA encephalitis should be remembered [9].
In accordance with the criteria proposed in 2013 by the International Encephalitis Consortium for diagnosing the clinical condition, one main criterion is necessary: change in mental state due to reduced level of consciousness or personality changes and lethargy for more than 24 hours, without other explainable causes. Still, two additional criteria are needed for possible encephalitis and three or more for probable or confirmed, including: fever greater than 38ºC in the last 72 hours or after the onset of symptoms, generalized or focal seizures without previous epileptic disorders, new neurological symptoms focal lesions, leukocytes greater than 5 mm3 in the cerebrospinal fluid and changes in neuroimaging and/or encephalography exams suggestive of encephalitis [10]. Additionally, the need for, in cases of suspected autoimmune etiology, a definitive diagnosis established by detection of autoantibodies was established [2]. However, the criteria proposed in 2013 are not capable of differentiating autoimmune and infectious etiologies of encephalitis. Thus, based on the need for criteria aimed at autoimmune processes, Graus et al in 2016 established clinical diagnostic criteria for autoimmune encephalitis [11].
In this sense, possible autoimmune encephalitis is characterized by acute or subacute onset with a course of less than three months and rapid progression of symptoms such as short-term memory deficits, altered mental status or psychiatric symptoms and at least one of the following: focal manifestations of the systemic central nervous system, unexplained seizures, cerebrospinal fluid pleocytosis, magnetic resonance imaging suggestive of encephalitis and exclusion of other etiologies [12]. Furthermore, based on the assumption that tests for specific antibodies are less available, the clinical criteria for autoimmune encephalitis proposed by Graus et al waive the requirement for these tests to be confirmed.
Specific criteria for anti-NMDA autoimmune encephalitis have also been developed, with the diagnosis being defined as probable when the following criteria are met: rapid onset of symptoms with at least four of the six groups (abnormal behavior or cognitive dysfunction, speech changes, seizures, of movement and dyskinesia, decreased level of consciousness, autonomic dysfunction, and central hypoventilation), plus at least the next laboratory results: abnormal EEG with focal or diffuse, slow or disorganized activity or extreme delta brush or cerebrospinal fluid with pleocytosis or oligoclonal bands . Finally, it is also necessary to exclude alternative etiologies [12].
Clinical investigation initially aims to confirm the presence of a focal or multifocal brain abnormality suggestive of encephalitis and possible differential diagnoses [13]. Electroencephalography is indicated when encephalitis is suspected for the differential diagnosis of a primary psychiatric disorder, exclusion of subclinical status epilepticus and for brain monitoring after the start of treatment. In anti-NMDA autoimmune encephalitis, findings such as: background slowness, rhythmic delta activity and epileptiform discharges are common, with the extreme delta brush wave pattern being found in 56-100% of cases [14].
Lumbar puncture with cerebrospinal fluid collection is indicated in all patients with suspected encephalitis in the absence of contraindications, and may initially be the first parameter changed. Therefore, CSF analysis should include differential cell, protein and glucose counts, oligoclonal bands, viral studies and bacterial cultures to exclude infectious etiologies. In the context of autoimmune encephalitis, frequent changes include mild to moderate lymphocytic pleocytosis and hyperproteinorrhaquia [15].
Furthermore, if anti-NMDA autoimmune encephalitis is suspected, patients should undergo screening for associated neoplasms in the possibility of paraneoplastic syndrome, especially in the young female population in which 50% of cases are diagnosed with ovarian teratoma [13].Therefore, tests such as tomography or magnetic resonance imaging of the abdomen and pelvis, as well as pelvic ultrasound can help and confirm the suspected diagnosis [16].
Specific treatment for autoimmune conditions is based on early and aggressive immunotherapy as the first line, which is associated with a better prognosis [17]. Thus, immunotherapy includes corticosteroids such as methylprednisolone, intravenous immunoglobulin and plasmapheresis and, in cases refractory to initial treatment, rituximab and cyclophosphamide as second line [8]. In the presence of neoplasms such as ovarian teratomas, management is based on timely removal combined with early immunotherapy, also providing a better prognosis [18].
In line with the International Consensus of Recommendations for the treatment of pediatric anti-NMDA autoimmune encephalitis, patients are initially classified according to the severity of the disease, evaluating parameters such as the need for intensive unit therapy and ventilatory support, movement disorders, psychiatric symptoms severe, inability to care for oneself, requiring full assistance, failure in communication, reduced level of consciousness and refractory status epilepticus. Therefore, patients with a mild clinical condition should receive corticosteroid therapy with methylprednisone 30 mg/kg, with a maximum of 1 g per day for 3 to 5 days, associated or not with intravenous immunoglobulin. If there is an inadequate response after one week of treatment, new immunotherapy and/or plasmapheresis should be initiated. Subsequently, after two weeks of treatment and inadequate response, second-line treatment should be initiated, with rituximab being preferable. Finally, if there is no improvement within 1 to 3 months after starting the first second-line immunotherapy, another medication should be administered, such as cyclophosphamide [19].
In this sense, the prognosis varies depending on the time between suspicion and the start of treatment, with late immunotherapy, age under two years and extreme delta brush in electroencephalography being factors for a worse prognosis. In addition, a large part of the pediatric population presents a good evolution, with total or partial recovery in almost 80% of cases, increasing when related to the early start of treatment [20].
CONCLUSION
Encephalitis is a complex brain condition caused by infections or autoimmune processes. Anti-NMDA receptor encephalitis, common in children and adolescents, is linked to ovarian teratomas. Diagnosis involves ruling out other causes through neuroimaging and CSF analysis. Diagnostic criteria struggle to differentiate autoimmune from infectious causes. Clinical symptoms include behavioral changes and movement disorders. Imaging tests reveal ovarian teratomas and characteristic delta waves on EEG. Serology for anti-NMDA antibodies confirms diagnosis but is often delayed due to cost and availability. Early immunotherapy and teratoma removal are crucial for a favorable outcome. In a clinical case, early immunotherapy and oophorectomy led to partial improvement, with complete recovery after rituximab administration.
REFERENCES
- Stawicka E. Anti-NMDA receptor encephalitis – the narrative review of literature with particular regard to pediatric population. Psychiatr Pol. 2022; 56: 1315-1326.
- Rincón López E, Rodríguez Vega H, Pietropaolo D, Mejías A. Anti- NMDA antibody encephalitis in paediatrics: A potentially treatable condition. Anales de Pediatria. An Pediatr (Barc). 2015; 82: e252-254.
- Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: Consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013; 57: 1114-1128.
- Luisa Martins Fernandes B, Webber J, Gonçalves Azevedo Vasconcelos L, Moacyr Vasconcelos M. Encefalites autoimunes Resumo Endereço para correspondência. Residência Pediátrica. 2018; 8: 26-34.
- Burrell R, Jones CA, Britton PN, Dale RC, Blyth CC, Clark JE, et al. Altered Behavior in Encephalitis: Insights from the Australian Childhood Encephalitis Study, 2013–2018. Front Pediatr. 2021; 9.
- Yeum TS, Lee J, Park SY, Joen Y, Kim BN. Childhood Onset of Anti- N-Methyl-D-Aspartate Receptor Encephalitis without Teratoma Masquerading as a Psychotic Disorder. J Korean Acad Child Adolesc Psychiatry. 2019; 30: 127-131.
- Pacheco LOPL, Castro K dos SK, Schmitt NM, Linhares MFS, Coelho PVE, Fernandes IMB, et al. Encefalite anti-NMDAr associada a tumores ovarianos: estudo de casos e revisão sistemática. Brazilian J Dev. 2023: 26389-26403.
- Abboud H, Probasco JC, Irani S, Ances B, Benavides DR, Bradshaw M, et al. Review: Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry. 2021; 92: 757.
- AlHakeem AS, Mekki MS, AlShahwan SM, Tabarki BM. Acute psychosis in children: Do not miss immune-mediated causes. Neurosciences. 2016; 21: 252-255.
- Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: Consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013; 57: 1114-1128.
- De Bruijn MAAM, Bruijstens AL, Bastiaansen AEM, Van Sonderen A, Schreurs MWJ, Sillevis Smitt PAE, et al. Pediatric autoimmune encephalitis: Recognition and diagnosis. Neurol Neuroimmunol NeuroInflammation. 2020; 7: 682.
- Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016; 15: 391-404.
- Ramlackhansingh AF, King AC, Maharaj S, King DJ. Clinical approach to the diagnosis and successful management of anti-NMDA receptor encephalitis when antibody testing is not possible. BMJ Case Rep. 2019; 12: 229593.
- Lin J, Elkins K, Bhalla S, Gedela S, Kheder A, Zhang G, et al. Electroencephalography characteristics to predict one-year outcomes in pediatric anti-NMDA receptor encephalitis. Epilepsy Res. 2021; 178: 106787.
- Wang R, Guan HZ, Ren HT, Wang W, Hong Z, Zhou D. CSF findings in patients with anti-N-methyl-d-aspartate receptor-encephalitis. Seizure. 2015; 29: 137-142.
- Yeum TS, Lee J, Park SY, Joen Y, Kim BN. Childhood Onset of Anti- N-Methyl-D-Aspartate Receptor Encephalitis Without Teratoma Masquerading as a Psychotic Disorder. J Korean Acad Child Adolesc Psychiatry. 2019; 30: 127.
- Zheng J, Shen J, Wang A, Liu L, Xiong J, Li X, et al. Clinical characteristics of anti-N-methyl-D-aspartate receptor encephalitis in children. J Cent South Univ. 2020; 45: 47-54.
- Walker CA, Poulik J, D’Mello RJ. Anti-NMDA receptor encephalitis in an adolescent with a cryptic ovarian teratoma. BMJ Case Rep. 2021; 14: e236340.
- Nosadini M, Thomas T, Eyre M, Anlar B, Armangue T, Benseler SM, et al. International Consensus Recommendations for the Treatment of Pediatric NMDAR Antibody Encephalitis. Neurol Neuroimmunol NeuroInflammation. 2021; 8: e1052.
- Yang S, Yang L, Liao H, Chen M, Feng M, Liu S, et al. Clinical Characteristics and Prognostic Factors of Children With Anti-N- Methyl-D-Aspartate Receptor Encephalitis. Front Pediatr. 2021; 9.