Atypical Presentation of Langerhans Cell Histiocytocis
- 1. Pediatrics Infectious Diseases Unit, Centro Hospitalar Universitário de Lisboa Central – EPE, Portugal
- 2. Pathological Anatomy Unit, Centro Hospitalar Universitário de Lisboa Central – EPE, Portugal
CITATION
Marujo F, Oliveira MI, Martins M, Brito MJ (2019) Atypical Presentation of Langerhans Cell Histiocytocis. Ann Pediatr Child Health 7(1): 1162.
ABBREVIATIONS
EBV: Epstein-Barr virus; CT: Computed Tomography; IGRA: Interferon-Gamma Release Assay; HIV: Human Immunodeficiency Virus; PPD: Purified Protein Derivative; VCA: Viral Capsid Antigen
CLINICAL IMAGE
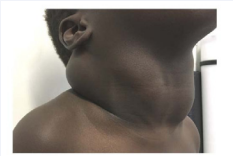
A 4-year-old male from Guinea-Bissau presented with a 3-year history of a painless, progressively enlarging bilateral cervical mass (Figure 1).
Figure 1 Bulky bilateral mobile cervical mass, painless and without inflammatory signs. Palpable angle of the jaw.
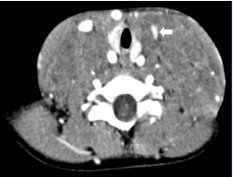
There was no failure to thrive, fever or any constitutional symptom. Dyspnea, dysphonia, sialorrhea and dysphagia were absent. Besides a bulky, tender bilateral cervical mass, physical exam was otherwise normal. There were no skin lesions, palpable lymphadenopathies or hepatosplenomegaly. Cervical ultrasonography showed an extensive, lobulated, solid, heterogeneous cervical mass involving cervical structures but not invading them. Contrast-enhanced cervical CT scan revealed a multicompartmental captive lesion involving the neck, with extension to the upper and anterior mediastinum (Figure 2).
Figure 2 Axial image from a contrast-enhanced cervical CT scan showing a multicompartmental, solid and captive lesion involving the neck, with extension to the upper and anterior mediastinum and left jugular vein compression. No evidence of calcification or compression of the airway. There were no other cervical or mediastinal adenopathies.
Skeletal survey, chest X-ray and abdominal ultrasound were normal. Complete blood count, erythrocyte sedimentation rate, C-reactive protein, liver and kidney function and urinalysis were normal. HIV, cytomegalovirus, bartonellosis were excluded. The PPD test had no induration and IGRA-QuantiFERON® was negative. VCA-IgG and EBNA antibodies for Epstein-Barr virus were positive and VCA-IgM was negative.
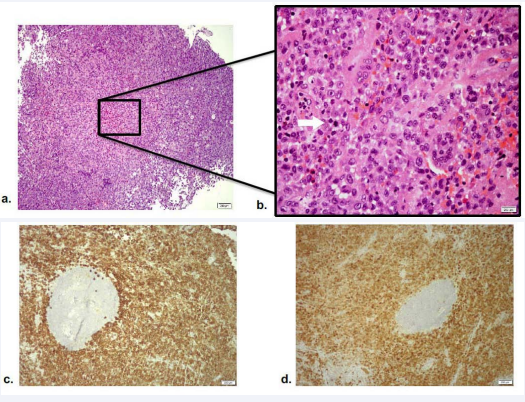
Excisional biopsy of the mass was performed and anatomopathological examination demonstrated partial effacement of lymph node with preservation of some follicular centers and an extensive infiltrate composed of sheets of histiocytes, with morphology of Langerhans cells (Figure 3).
Figure 3 (A) – [HE 100x - Distension of nodal sinuses by Langerhans cells, which are large cells with abundant, pale eosinophilic cytoplasm, irregular and elongated nuclei with prominent nuclear grooves and folds, fine chromatin and indistinct nucleoli. Focal necrosis and some eosinophils are observed.] (B) - [HE 400x - Langerhans cells have irregular and elongated nuclei with prominent nuclear grooves and folds, fine chromatin and indistinct nucleoli. Some are multinucleated. There are occasional mitotic figures.] (C) - [Langerhans cells are immunoreactive with CD1a.] (D) - [Langerhans cells are immunoreactive with S100]
Immunohistochemical staining showed positivity for S100 protein, CD68 and CD1a, confirming the diagnosis of Langerhans cell histiocytosis (LCH).
Also, EBV virus DNA was detected in biopsy by polymerase chain reaction. Etiology of neck masses in children typically fall into one of three categories: developmental, inflammatory/ reactive or neoplastic. Most cervical masses are infectious or reactive in origin. Enlarged lymph nodes that are firm and immobile, persist longer than six weeks or enlarge during a course of antibiotics should be evaluated and a biopsy is recommended [1].
LCH is a rare disease with unknown etiology characterized by abnormal proliferation of Langerhans cells [2]. Lymphadenopathy is seen in approximately 20% and in pediatric patients, cervical lymph nodes are the most frequently involved with known multisystemic disease [3]. Presentation of LCH as a cervical mass with lymph node involvement in a primary isolated form, without cutaneous or bone involvement, as the case we present, is extremely rare [3]. The diagnosis is based on histopathological examination [4,5].
Some reports indicate a higher detection of EBV in lymph nodes of patients with LCH [6,7]. It is tempting to establish a causal association between EBV and the pathogenesis of LCH. But recent publications indicate that this higher frequency is accounted for by the infection of by stander B lymphocytes and macrophages in LCH granuloma. This fact could be attributed to the immunossupressive micro environment found in the LCH granuloma [8,9].