Bone and Joint Infections in Children: Features and Outcome at CHU Gabriel Tour
- 1. Department of Pediatrics, CHU Gabriel Toure, Bamako-Mali, Mali
- 2. Department of Pedatric Surgery, CHU Gabriel Toure, Bamako-Mali, Mali
ABSTRACT
Aim: Osteoarticular infections in children are life-threatening and can lead to long-term disability. They require prompt medical care to reduce the risk of complications. The study was conducted in the paediatric department of the Gabriel Touré University Hospital. It was a prospective, descriptive clinical study lasting 18 months, from 1 January 2021 to 30 June 2022. Children aged 1 month to 15 years were included. The aim was to evaluate the features and therapeutic outcomes.
Results: Thirty-four (n=34) cases of osteoarticular infections were included. The hospital frequency was 1.66%. The mean age was 8 years (range 1-15 years). The Sex ratio was 3.25 (M=26; F=6). Eight patients had a history of sickle cell disease (23%). The topography of involvement was as follows: bone (n=19; 56%), joint (n=5; 15%), bone-joint (n=10; 29%). Humeral and femoral involvement accounted for 23.5% and 40% respectively. Blood cultures were performed on 22 samples, of which 8 were positive. The pathogens identified were Staphylococcus aureus (n=7; 32%) and Streptococcus pneumoniae (n=1; 4%). Staphylococcus aureus was proportionally sensitive to Oxacillin, Gentamycin and Ciprofloxacin in 85.7% of cases. Acute osteomyelitis accounted for 44% of cases. The mean duration of antibiotic treatment was 13.76±7.38 days, and 25 patients received appropriate antibiotics for a mean duration of 25.84±18.57 days. A combination of 3rd generation cephalosporin and aminoglycoside was used in 50% of cases. Surgical treatment consisted of flattening in 85% of cases (n=25). Red blood cell transfusion was performed in 82.3% of patients. The average hospital stay was 26 days (range: 10-65 days). Recovery was achieved in 97% of patients (n=33). One patient died due to sepsis.
Conclusion: Osteoarticular infections in children are still common in our teaching hospital. Staphylococcus aureus is the usual aetiology, but the emergence of new germs such as Salmonella and Escherichia coli requires attention.
KEYWORDS
- Osteoarticular infections
- Children
- Mali
CITATION
Traoré F, Maiga B, Amadou I, Keita A, Sacko K, et al. (2024) Bone and Joint Infections in Children: Features and Outcome at CHU Gabriel Touré. Ann Pediatr Child Health 12(4): 1343.
INTRODUCTION
Bone and joint infections in children are potentially life- threatening and can lead to long-term disability. They require prompt treatment to reduce the risk of complications [1,2]. Their incidence is now estimated at between 5.5 to 12 cases per 100,000 children [3]. It is a medical and surgical emergency because of the serious consequences in terms of musculo-skeletal functionality and growth. All age groups are concerned, from newborns to adolescents [4]. Osteoarticular infections in children include several entities (septic arthritis, acute osteomyelitis, osteitis, osteoarthritis, spondylodiscitis). Infection of bones, marrow and/ or joints in children most often occurs via the haematogenous route [5,6]. Diagnosis is generally based on clinical evidence, supported by biology, microbiology and imaging. In sub-Saharan Africa, the incidence of osteoarticular infections fluctuates. According to various studies, rates fluctuate between 6.8% and 26% [7].
In Mali, an initial study performed at the Gabriel Touré University Hospital in 2008 showed the magnitude of the problem. [8]. Early treatment consists of antibiotics, immobilisation of the affected extremity and, if necessary, surgical removal. Long- term antibiotic therapy is necessary to eradicate bone and joint infections. In the paediatric department of the Gabriel Touré University Hospital in Bamako (Mali), we are increasingly faced with the management of bone and joint infections. However, the lack of epidemioclinical and therapeutic data relating to this pathology inspired us to initiate this study in order to update our knowledge and understanding of this pathology.
METHODOLOGY
The research was performed in the paediatrics department of the Gabriel Touré University Hospital. It was a prospective and descriptive study over a period of 18 months, from 1 January 2021 to 30 June 2022.The objectives were to assess the epidemiology and to describe the clinical, bacteriological and therapeutic characteristics and outcome of osteoarticular infections. Children aged between 1 month and 15 years hospitalised for osteoarticular infections were included.
This was an exhaustive sampling procedure including all children hospitalised for osteoarticular infections and with a complete medical record. Data were collected from the clinical records of the patients. Each record was analysed using a survey form containing epidemiological, clinical, paraclinical and therapeutic data. The parameters collected were processed using SPSS 25.0 software (SPSS Inc., Chicago, IL). Quantitative variables were calculated as mean with standard deviation, while qualitative variables were expressed as numbers and percentages.
RESULTS
Thirty-four (n=34) cases of osteoarticular infections were included. The hospital frequency was 1.66%. The mean age was 8 years (range 1-15 years). Children aged 10 to 15 years were the most represented (47%). The sex ratio was 3.25 (M=26; F=6). Socioeconomic conditions were unfavourable in 85.3% of cases. Eight patients had a history of sickle cell disease (23%). The most frequent form was the homozygous SS form, accounting for 26.7% of cases. The distribution according to the origin of the infection was as follows (Table 1): post-traumatic (n=13; 38%), cutaneous (n=8; 23%), dental (n=1; 3%).
Table 1: Sources of infection
|
Sources |
Number |
Percent |
|
Unidentified |
12 |
35,3 |
|
Oral-dental |
1 |
2,9 |
|
Cutaneous |
8 |
23,5 |
|
Post-traumatic |
13 |
38,2 |
|
Total |
34 |
100 |
Twelve patients (35%) had an unidentified source of infection. Pain, fever and swelling were the most frequent reasons for consultation, respectively 100%, 88% and 94%. The topography of involvement was as follows: bone (n=19; 56%), joint (n=5; 15%), bone-joint (n=10; 29%). Humeral and femoral involvement accounted for 23.5% and 40% respectively (Table 2).
Table 2: Injury Topography
|
Sites |
Number |
Percent |
|
Upper limb |
|
|
|
Humerus |
8 |
23,5 |
|
Elbow |
7 |
20,6 |
|
Radius/ulna |
5 |
14,5 |
|
Wrist |
2 |
5,9 |
|
Hand |
1 |
2,9 |
|
Lower limb |
|
|
|
Femur |
16 |
40 |
|
Knee |
11 |
32,3 |
|
Tibia/Fibula |
7 |
20,6 |
|
Foot |
2 |
5,9 |
|
Hip |
1 |
2,9 |
|
Dorsal |
1 |
2,9 |
Blood cultures were taken from 22 samples, and were positive in eight of them. The germs identified were Staphylococcus aureus (n= 7; 32%) and Streptococcus pneumoniae (n=1; 4%). Staphylococcus aureus was proportionally sensitive to Oxacillin, Gentamycin and Ciprofloxacin in 85.7% of cases (Table 3).
Table 3: Antibiogram of bacteria identified in blood cultures
|
Detected germs n= 8 |
Antibiogram |
|
|
|
Sensitivity |
MIC (%) |
|
|
Oxacillin |
85,7 |
|
|
Gentamycin |
85,7 |
|
|
Ciprofloxacin |
85,7 |
|
Staphylococcus aureus |
Erythromycin |
57,1 |
|
|
Cefoxitin |
14,2 |
|
|
Amoxi+ac clavulanic |
14,2 |
|
|
Clindamycin |
14,5 |
|
Streptococcus pneumoniae |
|
|
|
|
Fosfomycin |
100 |
|
|
Lincomycin |
100 |
|
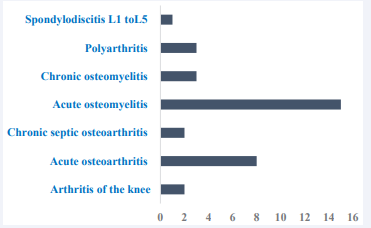
|
Vancomycin |
100 |
Cytobacteriological examination of the joint aspiration fluid revealed the following germs: Staphylococcus aureus (n=21; 72%), Salmonella sp (n=3;10%), Escherichia coli (n=2; 7%). Mean level of hemoglobin was 9 g/dl (range 4-10 g/dl). Neutrophil hyperleukocytosis was reported in 91% of patients. Over 97% of patients had elevated C-reactive protein levels. Standard X-ray imaging was performed for all patients (n=34; 100%). The most frequent findings were soft tissue thickening (n= 11; 37%) and diffuse bone demineralization (n= 6; 20%). Ultrasonographic examination of the knee revealed joint effusion in 41% of cases. Cytobacterial analysis of samples identified Staphylococcus Aureus in 72.4% of cases. The diagnosis is shown in Figure 1.
Figure 1 Types of bone infection.
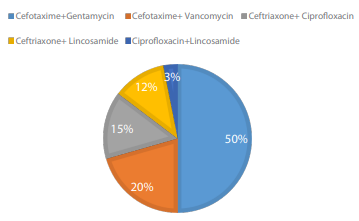
Figure 2 Used antibiotic combinations.
Acute osteomyelitis accounted for 44% of cases. The mean duration of probabilistic antibiotic therapy was 13.76±7.38 days. Twenty-five patients received appropriate antibiotic therapy for a mean duration of 25.84±18.57 days. The combination of cephalosporin and aminoglycoside was used in 50% of cases. Surgical treatment consisted of flattening in 85% of cases (n=25). Red blood cell transfusion was performed in 82.3% of patients. The average hospital stay was 26 days (range: 10-65 days). Recovery was achieved in 97% of patients (n=33). One patient died of sepsis.
DISCUSSION
The retrospective aspect of our study presents certain constraints. Our data were collected exclusively from hospitalization files. In the absence of a digital filing system, patient records are generally poorly managed and incomplete (missing pages, some results disaggregated, some pages stained with fluid, etc.). As a result, certain data could not be specified (compliance with oral treatment and post-hospitalization residual effects). Despite these limitations, these results can be discussed with other studies. The in-hospital frequency of osteoarticular infections was 1.66%. This result is lower than those published by P. Bedji [9], who reported 2.80%. Osteoarticular infections can occur at any age. Children aged between 5 and 15, with a mean age of 8.5, were the predominant group in our study (47.1%). This result is similar to those reported by N. Stoesse et al. [10], (mean age: 7.3), H. Oubejja et al. [11], (mean age: 7.5) and El Hamdi [12] (mean age: 9.7). Children at this age are much more active, and consequently exposed to the risk of injury and trauma. Males prevailed in our study, with a sex ratio of 3.25. Jana FC Neto et al., in their case series of twenty patients with osteoarticular infections, report similar data concerning male predominance [13]. Surveys conducted in the USA on the epidemiology of osteomyelitis and septic arthritis in children have confirmed the male predominance of infection [14]. EL Hamdi reported a sex ratio of 1.57, and the male tendency commonly observed in the literature, can be explained by the boys’ turbulence, which exposes them more to trauma. In our sample, socio-economic conditions were unfavorable in 85.3% of cases, and only 14.7% were favorable or acceptable. This result is similar to that of Jamilla EL HAMRI [15], where patients with a low socio-economic level represented 70.51% of cases and those with a medium or high socio-economic level only 29.49%. In sub-Saharan Africa, sickle cell disease is the main cause of osteoarticular infections in children, particularly osteomyelitis. Infections are generally facilitated by the existence of bone infarction following vaso- occlusive crises [16,17]. In our series, 23.5% of patients had a history of sickle cell disease, while Lamini N’Soundhal et al., found that 44.64% of children had sickle cell disease, attesting to the role of sickle cell disease in the development of osteoarticular infections [18]. Several authors reported the notion of a source of infection. In our study, trauma was founded in 38.2% of cases. In Ferroni case study, trauma was suspected in 44% of cases [19]. Trauma is implicated in 30-40% of osteoarticular infections [20,21]. Trauma, through the micro-haematomas created and the inflammatory processes of post-traumatic repair, is likely to lead to a localized circulatory slowdown in the sinusoidal loops, thus favoring bacterial seeding. Typically, the complaint is pain. In young children, pain may be difficult to localize, with lameness or functional impotence the only clinical sign. According to Juchler Céline, local inflammatory signs (edema, redness, heat and/or joint effusion) are observed in around 70% of cases, and more frequently in arthritis than in osteomyelitis. Fever is a classic but inconstant sign, found in only 60% of cases [22]. In our study, pain was found in all patients (100%), followed by fever (88.2%) and functional impotence (79.4%). In the current study, bone involvement (55.8% of cases) was more frequent than osteoarticular involvement (29.4%) and joint involvement (14.7%). Our results are comparable to those of Bedjj, who reported a bone involvement rate of 61.40% [9]. All bones can be affected, but long bones such as the femur and tibia are the most affected. In our study, the femur alone was affected in 40% of cases. Some authors have reported that the percentage of the lower limb affected varies between 70% and 77% [23-25]. H. Oubejja et al., and El Hamdi reported lower limb involvement in 93% and 91.30% respectively. The metaphysial fertility of the knee and the high frequency of trauma largely contribute to this tendency. Ninety-one percent of patients had hyperleucocytosis. These findings are higher than those of EL Hamdi, L. N’Soundhal and Trigui et al., who found hyperleukocytosis in 75% and 80, 2% [12,18]. C-reactive protein is useful both in diagnosis and in monitoring response to treatment. It is usually elevated at the outset, but C-reactive protein tends to normalize more rapidly with appropriate treatment, indicating good progression [26-28]. In our study, 97% of our patients had high C-reactive protein, and this finding was in agreement with that of N. Le Sau, who had 95% high C-reactive protein at diagnosis [6]. C-reactive protein is an effective biological marker for surveillance of treatment of osteoarticular infections in children. According to the literature, the positivity rate for blood cultures is between 30% and 60%, and for aspiration between 30% and 80% [29-32]. The reasons for these figures are probably numerous: diagnostic criteria for osteoarticular infection may be too extensive, or the infection may have been treated with prior antibiotic therapy. In our study, 64.7% of our patients had performed blood cultures and 36.4% were positive, similar to the results reported in the literature and by Kouame Ygs. Blood cultures were performed in 56.2% of cases, with a positivity rate of 40% [33]. In Senegal, blood cultures were positive in 33.33% of cases [34]. We observed a predominance of Staphylococcus aureus (gram-positive cocci) with 87.5%. Our bacteriological data do not differ from those of the literature and Kouame YGS. The relative frequency of Staphylococcus aureus is between 50 and 90% [35,36]. Staphylococcus Aureus is the germ most frequently isolated in osteoarticular infections. X-rays should be the first-line investigation. The earliest signs are extraosseous [37]. Conventional X-ray is often normal in the early stages, and will be supplanted by ultrasonography to detect sub- periosteal abscesses or intra-articular effusion. With regards to the diagnosis of osteoarticular infections, our results are inferior to those of Kouamé YGS et al., who found 58.5% osteomyelitis and 42.5% osteoarthritis. J El Hamri, who reported arthritis (39.7%), osteomyelitis (25.64%) and osteoarthritis (34.6%). Antibiotic therapy should be initiated as early as possible [30,39,40]. Initially, it should be probabilistic, then adapted to the germs encountered. Several authors use a combination of oxacillin and an aminoglycoside. A cephalosporin may also be used. The antibiotic is given intravenously, with the duration varying from 10 days to 3 weeks, followed by oral administration to 4-6 weeks. We achieved a complete recovery in 97% of patients. One patient died (3%) in the context of sepsis. Our cure rate is similar to that reported in the literature.
CONCLUSION
Osteoarticular infections remain frequent in our setting, affecting mostly boys aged 5 to 15. In our study, Staphylococcus aureus is the most common aetiology of osteoarticular infections, but particular attention should be given to the emergence of Salmonella and Escherichia coli. A prospective study on the etiology of osteoarticular infections is therefore needed.
ETHICAL CONSIDERATIONS
Upon admission, the patient’s parents or legal guardians approved their participation in a clinical research project. The national ethics committee approved the research protocol.
REFERENCES
- Alvares PA, Mimica MJ. Osteoarticular infections in pediatrics. J Pediatr (Rio J). 2020; 96: 58-64.
- Coulin B, Demarco G, Spyropoulou V, Juchler C, Vendevure T, Habre C, et al. Osteoarticular infection in children. Bone Joint J. 2021; 103- B(3): 578-583.
- Montgomery NI, Rosenfeld S. Pediatric osteoarticular infection update. J Pediatr Orthop. 2015; 35: 74-81.
- Jeyanthi JC, Yi KM, Allen JC Jr, Gera SK, Mahadev A. Epidemiology and outcome of septic arthritis in childhood: a 16-year experience and review of literature. Singapore Med J. 2022; 63: 256-262.
- Timsit S, Pannier S, Glorion C, Chéron G. Infections bactériennes ostéoarticulaires du nourrisson et de l’enfant : expérience sur un an. Archives de Pédiatrie 2005 ; 12: 16-22.
- Le Sau N. Le diagnostic et la prise en charge des infections ostéoarticulaires aigües chez l’enfant. Paediatrics and Child Health. 2018; 23: 344-352.
- Ngaroua, Joseph Eloundou Ngah, Yacouba Djibrilla Et Al. Incidence des infections du site opératoire en Afrique subsaharienne : Revue systématique et méta-analyse. Pan Afr Med J. 2016; 24: 171.
- Sangare A, Alwata I, Sidibe S, Macalou M, Toure AA. Les osteites dans le Service d’Orthopedie et de Traumatologie de l’Hopital Gabriel Toure de Bamako [Osteitis at the service of orthopedics and traumatology at the Hopital Gabriel Toure in Bamako]. Mali Med. 2008; 23: 27-30.
- Pierre Bedji. Infection ostéoarticulaires dans le service de chirurgie orthopédique et traumatologique de centre hospitalier universitaire Gabriel Touré. Mémoire : Bamako Mali. 2021 ; 37.
- Stoesser N, Pocock J, Moore CE, Sona S, PutChhat H, Poda S, et al. The epidemiology of pediatric bone and joint infections in Cambodia, 2007-2011. J Trop Pediatr. 2013; 59: 36-42.
- Oubejja H, sadki H, Lahlou I, erraji M, Rozine R, Ettayebi F, soulaymani A. Infection ostéoarticulaires chez l’enfant de plus de 3 ans profil épidémiologique International journal of innovation and applied studies. 2016 ; 16 : 226.
- El hamdi fatima zahrae. Les infections ostéoarticulaires de l’enfant caractéristique bactériologique des isolats au centre hospitalier universitaire hassan ii de fès juillet. 2022
- Jaña fc neto, ortega cs, goiano eo. Epidemiological study of osteoarticular infections in children. Acta ortop bras. 2018; 26: 201- 205.
- Okubo Y, Nochioka K, Testa M. Nationwide survey of pediatric acute osteomyelitis in the USA. J Pediatr Orthop B. 2017; 26: 501-506.
- Jamila el hamri. Les infections ostéoarticulaires de l’enfant expérience de service de traumatologie pédiatrique au centre Hospitalier Universitaire de Marrakech. Thèse de Méd. No 50 : 2012
- Alima Yanda AN, Nansseu JR, Mbassi Awa HD, Tatah SA, Seungue J, Eposse C, et al. Burden and spectrum of bacterial infections among sickle cell disease children living in Cameroon. BMC Infect Dis. 2017; 17: 211.
- Mouafo Tambo FF, Ngowe MN, Andze OG, Sosso MA. Aspects of the epidemiology, diagnosis and management of sickle cell osteomyelitis in children in Africa. Sante. 2010; 20: 221-224.
- Lamini N’soundhat NE, Ondima IPL, Moyikoua RF. Les Infections Ostéoarticulaires de l’Enfant: Étude Rétrospective Monocentrique de 112 Cas Suivis au Centre Hospitalier Universitaire de Brazzaville (Congo). Health Sci Dis. 2019; 20: 37-42.
- Ferroni A, H Al Khoury, Dana C, Quesne G, Berche P, Glorion C, Péjin Z. Prospective survey of acute Osteoarticular infections in a French paediatric orthopedic surgery unit. 2013; 19: 822-882
- Grimprel E, Cohen R. Epidémiologie et physiopathologie des infections ostéoarticulaires chez l’enfant (nouveau-né exclu). Archives de pédiatrie. 2007; 14: 81-85.
- Ross Cronin, Anne-Marie McMahon. Bone and joint infections. Symposium: connective tissue and bones. Paediatrics and Child Health. 2015 ; 25 : 561-566.
- Juchler Céline. Evolution de l’épidémiologie bactérienne dans les infections ostéo-articulaires pédiatriques à Genève. 2018.
- Sonnen GM, Henry NK. Pediatric bone and joint infections. Diagnosis and antimicrobial management. Pediatr Clin North Am. 1996; 43: 933-947.
- Manz N, Krieg AH, Buettcher M, Ritz N, Heininger U. Long-Term Outcomes of Acute Osteoarticular Infections in Children. Front Pediatr. 2020; 8: 587740.
- Agarwal A, Aggarwal AN. Bone and Joint Infections in Children: Acute Hematogenous Osteomyelitis. Indian J Pediatr. 2016; 83: 817-824.
- Alvares PA, Mimica MJ. Osteoarticular infections in pediatrics. Journal de Pediatria. 2020; 96: 58-64.
- Wagner N, Ceroni D, Niederer A, Ritz N, Relly C. Prise en charge des infections ostéoarticulaires aigues de l’enfant : recommandations des Groupes suisses d’infectiologie pédiatrique (PIGS), d’orthopédie pédiatrique et de chirurgie pédiatrique. Paediatrica. 2017; 28: 7-11.
- Akinkugbe O, Stewart C, McKenna C. Presentation and Investigation of Pediatric Bone and Joint Infections in the Pediatric Emergency Department. Pediatr Emerg Care. 2019; 35: 700-704.
- Mouzard A. Bégué P, Astruc J. Infections bactériennes ostéoarticulaires. In: editors. Pathologie infectieuse de l’enfant. Paris: Masson. 1999 ; 503-509.
- François P, Sarlangue J, Grimprel E, Carriere JC, Garnier JM, de Montalembert M, et al. Groupe de pathologie infectieuse et tropicale de l’enfant. Épidémiologie et diagnostic bactériologique des infections osseuses et articulaires de l’enfant. Enquête multicentrique. Med Mal Infect. 1992; 22: 758-762.
- Christiansen P, Frederiksen B, Glazowski J, Scavenius M, Knudsen FU. Epidemiologic, bacteriologic, and long-term follow-up data of children with acute hematogenous osteomyelitis and septic arthritis: a ten-year review. J Pediatr Orthop B. 1999; 8: 302-305.
- Fink CW, Nelson JD. Septic arthritis and osteomyelitis in children. ClinRheum Dis. 1986; 12: 423-435.
- Kouame YGS, Kouamé. DB, Tembely S, Yaokreh JB, Koffi KM, Sounkerem. M, et al. Etude bactériologique des infections ostéoarticulaires de l’enfant au Service de chirurgie pédiatrique du Centre Hospitalier Universitaire de Yopougon. Revues-ufhd-ci. Org
- Camara ES, Sane JC, Bousso A. Les ostéomyélites aigues à Dakar. MedAfr Noire. 2012; 59: 313-321
- Moumile K, Merck J, Glorion C, Pouliquen JC, Berche P, Ferroni A. Bacterial aetiology of acute osteoarticular infections in children. Acta Pædiatrica. 2005; 94: 419-422.
- Saul NF, Clark J, Pallett A, Nicholas MP. Managing bone and joint infection in children. Arch Dis Child. 2012; 97: 545-553.
- Bréhin C, Claudet I, Dubois D, Vial J, Chaix Y, Grouteau E, et al. Assessing the management of pediatric bone and joint infections according to French guidelines. Med Mal Infect. 2020; 50: 515-519.
- Loro A, Fulvio F, Alt V. Treatment of bone infections in children in low-income countries - A practical guideline based on clinical cases. Injury. 2023; 54: 111066.
- Mitchell PD, Abraham A, Carpenter C, Henman PD, Mavrotas J, McCaul J, et al. Consensus guidelines on the management of musculoskeletal infection affecting children in the UK. Bone Joint J. 2023; 105-B: 815- 820.
- Autore G, Bernardi L, Esposito S. Update on Acute Bone and Joint Infections in Paediatrics: A Narrative Review on the Most Recent Evidence-Based Recommendations and Appropriate Antinfective Therapy. Antibiotics (Basel). 2020; 9: 486.