High Prevalence of Suicide and Self-Harm among Adolescent Mental Disorders in Huangshi during the COVID-19 Pandemic Era, China
- 1. Hubei Key Laboratory of Renal Disease Occurrence and Intervention, Medical School, Hubei Polytechnic University, China
- 2. Psychological children’s Ward, Mental Health Center of Huangshi, China
ABSTRACT
This study aimed to explore the influence of the COVID-19 pandemic on mental health among adolescents and the associated factors that caused high suicide and self-harm rates among adolescents. A comprehensive statistical analysis based on clinical interviews and self-reports from patients or their parents was performed. DSM-5, ICD-11, and the National Institute Mental Health Research Domain Criteria were used as criteria for the diagnosis of mental disorders. SPSS 26.0 software was used for statistical analysis. This study included 742 adolescent patients; the gender ratio was 1.54 (female to male), and their ages ranged from 5 to 18. The majority of cases are in high school (625/742, 84.23%), and the highest prevalence occurred at 16 years. Family-related factors, academic stress, genetic factors, and school violence were the main reasons for adolescent mental disorders. A high prevalence of suicide (or suicidal attempts) and self-harm was observed in depressive and bipolar disorder among adolescents during the COVID-19 pandemic. Statistical analysis reveals that the COVID-19 pandemic has strained family relationships and increased academic stress. An increasing trend of mental disorders among adolescents has been observed since 2018, particularly in 2021. The COVID-19 pandemic directly or indirectly increased the suicide and self-harm prevalence among adolescents.
KEYWORDS
- Adolescent
- COVID-19
- Mental disorders
- Self-harm
- Suicide
CITATION
Xie J, Hong Y, Yang J, Zhang X (2024) High Prevalence of Suicide and Self-Harm among Adolescent Mental Disorders in Huangshi during the COVID-19 Pandemic Era, China. Pediatr Child Health 12(4): 1344.
CORE TIP
More adolescents have suffered from mental disorders, and the morbidity has increased annually. Suicide and self-harm rates have surged due to the COVID-19 pandemic. In this study, there was a significant increase in the number of cases between during and before the COVID-19 pandemic, and the pandemic may lead to an increase in suicide and self-harm by intensifying family conflict and promoting academic stress. Our study aimed to draw the attention of society, families, and schools to the importance of mental health among adolescents, providing guidance and references for the prevention, diagnosis, and treatment of adolescents.
INTRODUCTION
Based on a comprehensive analysis conducted by the GBD 2019 Mental Disorders Collaborators, a report was issued regarding the worldwide, regional, and national impact of 12 mental disorders across 204 countries and territories [1]. Approximately 9.7% of the population with an age < 20 years suffered from mental disorders, worldwide, based on the Global Health Data Exchange (2019 data). Globally, it is estimated that one in seven 10-19-year-olds experiences a mental disorder, accounting for 13% of the global burden of disease, yet these remain largely unrecognized and untreated [2]. More than 970.1 million estimated mental disorders were reported by GBD 2019, with an increase of 48.1% between 1990 and 2019 [1]. According to a survey conducted by the China Mental Health Survey, the weighted prevalence of mental disorders among adolescents in China was 17.5% [3].
Depression is increasingly prevalent among mental disorders, and has emerged as a prominent cause of disability and a significant contributor to the global burden of disease [1]. Mental disorders are clinically characterized by significant impairments in cognitive function, emotional regulation, and behavior that may ultimately lead to physical dysfunction and even suicidal ideation in severe cases [4].
The causes of mental disorders remain uncertain, and are largely due to biological, genetic, environmental, and psychological factors. The swift advancement of the economy has augmented societal rivalry and diverse psychological pressures, thereby substantially elevating the incidence of mental disorders among adolescents. One example would be the imposition of rigorous academic standards on students, or the onset of a complex array of physiological, emotional, and social transformations during adolescence that can significantly exacerbate psychological stress [5]. In 2020, due to the COVID-19 pandemic and prolonged home quarantine, the incidence and risk of mental disorders among adolescents increased remarkably [6]. Despite the advantages of sports participation, adolescent athletes still exhibit elevated levels of depression and anxiety during the COVID-19 pandemic. This indicates that addressing mental health concerns remains a crucial priority even for this demographic [7]. A comprehensive systematic review and meta-analysis of 134 cohorts has determined that when comparing the levels of general mental health, anxiety symptoms, or depression symptoms during the pandemic to pre-COVID-19 outcomes within the same participant cohort, there were no discernible negative changes in mental health at a population level for general mental health or anxiety symptoms. Nonetheless, a marginal intensification in depressive symptomatology was noted, with women or female groups bearing an inequitable burden from the pandemic [8].
Suicide is the fourth leading cause of death in people aged 10- 24 years [9]. Some studies have reported a surge in the incidence of suicidal ideation and attempts among both adolescents and adults amidst the COVID-19 pandemic, thereby underscoring the dire state of mental health and suicide crisis [10-13]. The other reports indicated a consistent prevalence of mental disorders, which could be attributed to varying policies and precautions implemented across diverse countries and territories [14-17].
In the present study, an epidemiological analysis of the collected cases was performed and summarized based on the time of visit, gender, educational distribution, and family-related risk factors. Moreover, abnormal illness behaviors, especially prevalence of self-harm and suicide, during and before the COVID-19 pandemic were statistically analyzed. Our findings may provide a reference and clinical guidance for the prevention and intervention of mental disorders among adolescents.
CASE INFORMATION AND METHODS
Cases collection
During the period spanning from January 1, 2018 to December 31, 2022, a comprehensive analysis was conducted on a total of 742 cases involving individuals aged eighteen years or younger.
Inclusion criteria
The diagnostic criteria utilized in this study were based on the DSM-5 Diagnostic and Statistical Manual of Mental Disorders, the ICD-11 International Classification of Diseases, and the National Institute of Mental Health’s Research Domain Criteria [18,19]. We enrolled participants aged 18 years or younger who possessed complete case records and fulfilled the diagnostic criteria. Exclusionary factors comprised individuals who sought medical attention but did not exhibit symptoms of mental disorders, those with incomplete data, and those failing to meet the diagnostic criteria.
Abnormal illness behaviors
According to the Severe Psychiatric Diseases Management and Treatment Norms 2018 published by China’s Health Commission (in Chinese), abnormal illness behaviors were divided into nine subtypes (M1-M9, M7: apathetic, solitary, sluggish, and unable to study, work, live normally, M8: committed suicide and/or attempts, M9: self-harm), which we have illustrated in detail in our previous studies [20, 21].
Assessment of causes
In our previous studies [20,21], we examined the underlying causes of family-related factors, genetic factors, school violence, and academic stress. Family-related factors were assessed using self-report and through discussions with participants and their parents. Genetic factors were identified based on the presence of mental disorders within three generations of both the paternal and maternal lineages. School violence and academic stress were reported by participants, reflecting their experiences of school life, academic pressure, and instances of violence.
Statistical analysis
The data were imported into SPSS 26.0 for statistical analysis, and the resulting numerical values will be presented. *p<0.05, **p<0.01, ***p<0.001, when p<0.05 is considered as a significant difference. To compare the differences in suicide, self-harm, and apathetic, solitary, sluggish, and unable to study, work, live normally number per month between before and during the COVID-19 pandemic, non-normally distributed incontinuous variables were represented by median and tested using Mann- Whitney U test.
To investigate the relationship between suicide/self-harm behaviors and independent variables, including the COVID-19 pandemic, family-related factors, school violence, and academic pressure. Multivariable logistic regression (forward LR) analysis will be employed to test the correlation between each identified variable and suicide/self-harm outcomes. A significance level of P > 0.10 indicates a lack of relevant influence. After excluding non- statistically significant influencing factors, the remaining variable will be tested. P-values and 95% CI of OR will be obtained.
Bivariate logistic regression analyses will be conducted to test the correlation between the COVID-19 pandemic variable excluded by forward LR and family-related factors or academic stress. P-values and 95% CI of OR will be calculated.
RESULTS
Case information on mental disorders among adolescents in Huangshi
A total of 742 individuals with mental disorders were clinically diagnosed and recruited (Figure 1).
Figure 1 Flowchart of the study.
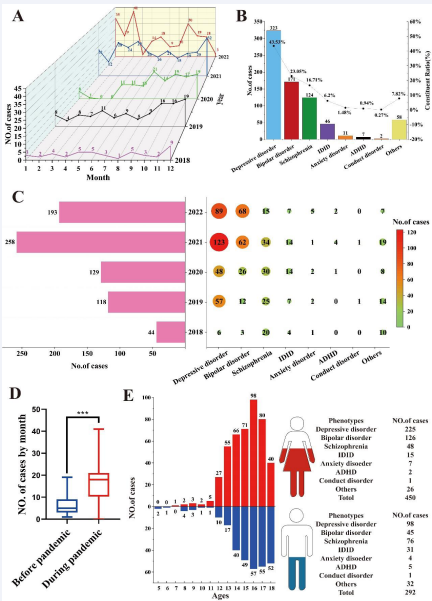
.The distribution of cases across different years and months is presented in (Figure 2A). Owing to the government’s implementation of a home quarantine policy in Huangshi, no cases were reported during March and April 2020 (Figure 2A).
Major types of mental disorders and constituent ratios are listed in (Figure 2B). The top three types of mental disorders in the present study were depressive disorder (323/742, 43.53%), bipolar disorder (171/742, 23.05%), and schizophrenia (124/742, 16.71%) (Figure 2B). The number of bipolar disorders among patients exhibited a gradual upward trend from 2018 to 2022 (Figure 2C). The number of cases markedly increased in 2020-2022, compared with 2018-2019 (Figure 2C).
Before and during the COVID-19 pandemic, the overall median increased from 5 to 18, as evidenced by a p-value<0.001 (Figure 2D). There was a significant difference in the number of cases between the before pandemic (BP) and during pandemic (DP) groups by month (Figure 2D).
The 742 cases comprised 450 girls and 292 boys, with a gender ratio of 1.54:1 (Figure 2E). The age range was 5-18, with an average of 15.25 ± 2.09, and the highest incidence was observed in 16-year-olds (Figure 2E). More girls developed depressive disorder and bipolar disorder than boys, whereas the situation was opposite in schizophrenia and idiopathic developmental intellectual disability (IDID) (Figure 2E).
Figure 2 Case information. (A). Case distribution from January 2018 to December 2022 by month. (B). Constituent ratio of mental disorders among adolescents in Huangshi (N=742). (C). Case distribution by year and different types of mental disorders. (D). Case distribution by month during and before the COVID-19 pandemic. (E). Age and gender distribution with different mental disorders among adolescents in Huangshi.
Possible factors causing mental disorders
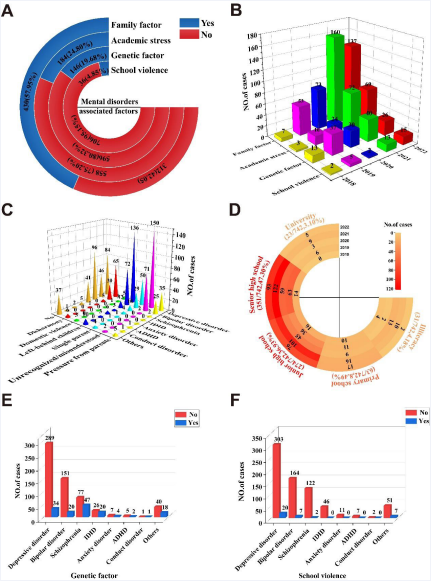
More adolescents have developed mental disorders in recent years. Possible factors causing adolescent mental disorders were investigated in the present study. More than half of the surveyed patients claimed that the causes were family-associated factors (430/742, 57.95%) (Figure 3A). The following causes were identified: academic stress (184/742, 24.80%), genetic predisposition (146/742, 19.68%), and school violence (36/742, 4.85%) (Figure 3A).
According to the case distribution by possible factors and year, the main factors causing mental disorders were family- associated factors and academic stress; however, genetic predispositions and school violence also can’t be ignored in their contribution to mental disorders (Figure 3B).
Among family-related risk factors, being unrecognized or misunderstood by their families and left-behind children are the two most significant causes of mental disorders among adolescents, especially depressive disorder and bipolar disorder (Figure 3C).
The educational background of the collected cases is illustrated in (Figure 3D), and 625 patients, accounting for 84.23% of the total, were derived from high school, which proved the fierce academic stress.
Genetic predisposition constitutes a significant risk factor for the development of mental disorders, particularly in schizophrenia (47/77, 61.04%) and IDID (20/26, 76.92%) (Figure 3E). Additionally, the role of school violence as a contributing factor to mental disorders should not be disregarded (Figure 3F).
Figure 3 Possible factors causing mental disorders. (A). Four main reasons causing adolescent mental disorders. (B). Case distribution by different factors annually. (C). Family-associated factors. (D). Educational distribution and academic stress. (E). Genetic factor. (F). School violence..
High prevalence of suicide and self-harm among adolescents
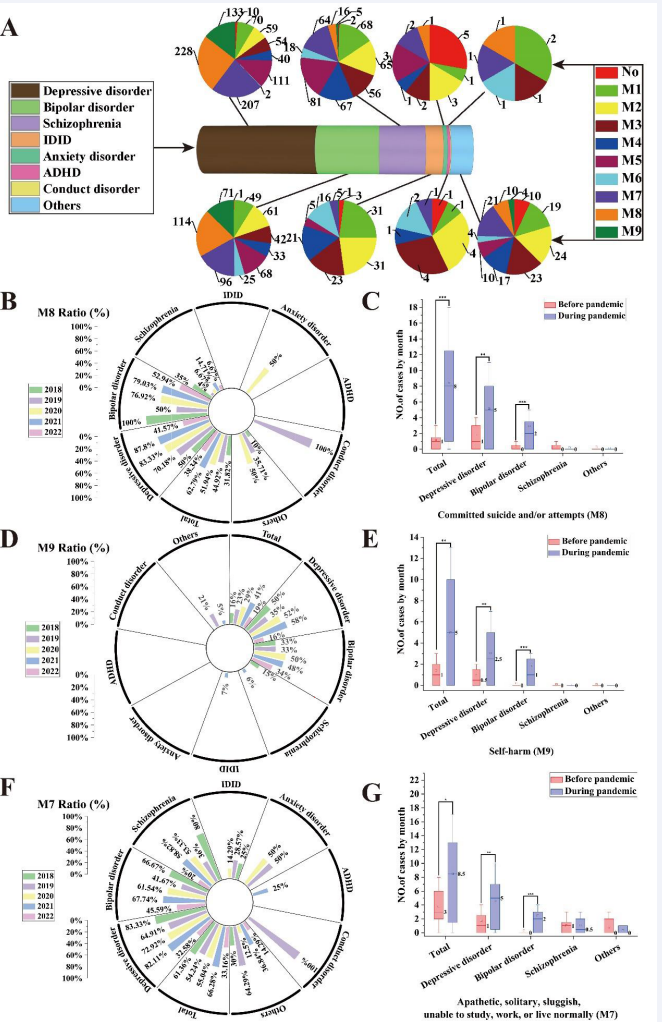
Abnormal illness behaviors refer to a range of unfavorable clinical manifestations that stem from mental disorders. Among these, the most severe are committed suicide and/or attempts (M8) as well as self-harm (M9). Of the 323 cases of depression examined, 228 individuals exhibited suicidal ideation and/or attempts, while 133 patients engaged in self-harm, accounting for 70.59% and 41.18% respectively (Figure 4A). Moreover, in cases of bipolar disorder, 66.67% (114/171) of patients committed suicide or attempted suicide, and 41.52% (71/171) of individuals engaged in self-harm (Figure 4A). In schizophrenia, the rates of committed suicide and/or attempts (M8) and self-harm (M9) exhibited a decrease, with proportions of 12.90% (16/124) and 4.03% (5/124) respectively (Figure 4A).
Furthermore, it is important to acknowledge the presence of unfavorable clinical manifestations such as apathetic, solitary, sluggish, and unable to study, work, live normally (M7). Among individuals with depressive disorder, there were 207 cases, while bipolar disorder and schizophrenia had 96 and 64 cases respectively, experiencing symptoms categorized as M7. These figures corresponded to percentages of 64.09% (207/323), 56.14% (96/171), and 51.61% (64/124) respectively (Figure 4A).
The proportion of completed suicides and/or suicide attempts (M8) was calculated and presented in (Figure 4B). A notable increase in the ratio of M8 was observed in total, as well as in depressive disorder and bipolar disorder during the time period of 2020-22 compared to 2018-19, demonstrating extreme significance (Figure 4C).
Regarding self-harm (M9), significant increases in the ratio of M9 during 2020-22 were observed compared to 2018-19 across all categories: total, depressive disorder, and bipolar disorder (Figure 4 D&E).
A significant difference was observed in the incidence of suicide and/or attempts between the before-COVID-19 period and the during-COVID-19 pandemic among adolescents. Furthermore, a remarkably significant disparity was observed among patients who engaged in self-harm between the pre- pandemic and pandemic periods, whereas the findings remained consistent for cases with depressive disorder and bipolar disorder (Figure 4 C&E). The ratio of M8 and M9 reached its highest level in 2020-21, when the COVID-19 pandemic impacted the entire world.
Furthermore, in the context of apathetic, solitary, sluggish, and unable to study, work, live normally (M7), there was a significant increase in the ratio of M7 during the COVID-19 pandemic in comparison to the period prior to the COVID-19 pandemic (Figure 4 F&G).
Figure 4 High prevalence of suicide and self-harm among adolescents. (A). Abnormal illness behaviors distribution in various mental disorders. (B)
Committed suicide and/or attempts (M8) ratio distribution from 2018 to 2022 among different mental disorders. (C) Case with M8 distribution by month before and during the COVID-19 pandemic. (D) Self-harm (M9) ratio distribution from 2018 to 2022 among different mental disorders. (E) Case with M9 distribution by month before and during the COVID-19 pandemic. (F) Apathetic, solitary, sluggish, and unable to study, work, live normally (M7) ratio distribution from 2018 to 2022 among different mental disorders. (G) Case with M7 distribution by month before and during the COVID-19 pandemic.
Through multivariable logistic regression (forward LR) analysis, it was determined that both family-associated factors and academic stress exerted significant effects on suicide and self- harm (P<0.05). Conversely, school violence did not demonstrate a statistically significant impact on suicide and self-harm (P>0.1), thus rendering it an excluded influence factor.
Bivariate logistic regression analysis showed that the pandemic had a statistically significant impact on family factors (P<0.001, OR=2.995, 95% Cl 2.088-4.289), and the influence of the pandemic on academic stress was statistically significant (P<0.001, OR=2.992, 95% Cl 1.794-4.990) (Table 1).
Multivariable logistic regression analysis revealed that family-associated factors had a statistically significant influence on suicide (P<0.001, OR=4.881, 95% CI 3.517-6.775). Furthermore, the effect of academic stress on suicide was also found to be statistically significant (P<0.01, OR=1.651, 95% CI 1.134-2.404). The influence of family-related factors on self-harm was found to be statistically significant (P<0.001, OR=3.866, 95% CI 2.626-5.693). Additionally, academic stress was also found to have a statistically significant association with self-harm (P<0.05, OR=1.597, 95% CI 1.104-2.309) (Table 1).
Table 1: Univariate and multivariable logistic regression analysis exploring the relationship between the COVID-19 pandemic, and family-related factors, academic stress, suicide and self-harm.
|
Independent variable |
Dependent variable |
B |
S.E. |
Wald |
P |
OR |
95%CI |
|
Family-related factor (1) |
Suicide |
1.585 |
0.167 |
89.820 |
0.000 |
4.881 |
(3.517, 6.775) |
|
Academic stress (1) |
0.501 |
0.192 |
6.842 |
0.009 |
1.651 |
(1.134, 2.404) |
|
|
Family-related factor (1) |
Self-harm |
1.352 |
0.197 |
46.931 |
0.000 |
3.866 |
(2.626, 5.693) |
|
Academic stress (1) |
0.468 |
0.188 |
6.178 |
0.013 |
1.597 |
(1.104, 2.309) |
|
|
Pandemic (1) |
Family-related factor |
1.097 |
0.184 |
35.464 |
0.000 |
2.995 |
(2.088, 4.298) |
|
Academic stress |
1.096 |
0.261 |
17.643 |
0.000 |
2.992 |
(1.794, 4.990) |
DISCUSSION
The COVID-19 not only caused huge damage to the global economy and human deaths but also exacerbated mental health crises. More people have developed mental disorders globally [22]. Our analysis indicates that the weighted prevalence of mental disorders among adolescents in Huangshi ranges between 15% and 20%.
In the current investigation, a total of 742 valid cases were enrolled, with a higher proportion of female participants observed in both depressive and bipolar disorders. This finding may be attributed to the influence of sensitive emotions, sex hormones, and pubertal development. Notably, the vulnerable age group was identified as ranging from 13 to 18 years old, which highlights the significant academic pressure experienced by Chinese adolescents.
The statistical significance observed between the pre-COVID-19 and COVID-19 pandemic periods indicates a discernible shift in patient distribution, with an apparent surge in patients attributed to the pandemic.
Based on the current survey, four primary potential factors were identified, ranked in order of family-related factors, academic stress, genetic factors, and school violence. The significant causes of mental disorders related to family factors were often unrecognized/misunderstood by their families and left-behind children. This highlights the crucial role that parents and families play in the physical and mental development of adolescents.
Genetic predisposition plays a critical role in the development of mental disorders, particularly schizophrenia and IDID. While school violence poses a global challenge to adolescents, its impact in China appears to be comparatively lower than that observed overseas.
The nine classified abnormal illness behaviors serve as a better guide for identifying destructive behaviors among adolescents with mental disorders. The most severe and prominent abnormal illness behaviors include committed suicide and/or attempts (M8) and self-harm (M9). The prevalence of suicide and self-harm among adolescents has surged during the COVID-19 pandemic period.
Additionally, there was a significant increase in the number of cases experiencing symptoms of apathetic, solitary, sluggish, and unable to study, work, live normally (M7) during the COVID-19 pandemic. This observation highlights the detrimental impact of the pandemic on adolescents, particularly their mental health.
A significant difference was observed in the distribution of suicide and/or attempts (M8) and self-harm (M9) cases by month between the pre-COVID-19 and COVID-19 pandemic periods. Multivariate logistic regression analysis confirmed that the COVID-19 pandemic had a notable impact on the surge of suicide and self-harm ratios among adolescent mental disorders, which were attributed to family-associated factors and academic stress.
The escalating mental health issue among Chinese adolescents has emerged as a crucial public health concern with implications for the future of the country and its population. On December 8, 2019, the Chinese Center for Disease Control and Prevention unveiled the Action Plan for Children and Adolescents’ Mental Health. This initiative aims to promote mental health services between 2019 and 2030, enhance intervention strategies, and bolster adolescents’ understanding of core mental health concepts.
Likewise, on January 26, 2020, the Bureau for Disease Control and Prevention of the National Health Commission issued the Guiding Principles for Emergency Psychological Crisis Intervention in the Novel Coronavirus Pneumonia Epidemic. This document aims to expand mental health services and mitigate severe outcomes like suicide and impulsive behavior. It also outlines specific intervention points for individuals infected with the new coronavirus, as well as their families, friends, and other affected groups.
Furthermore, on March 11, 2021, the Fourth Session of the 13th National People’s Congress approved the adoption of the 14th Five-Year Plan for National Economic and Social Development and the Outline of the 2035 Vision Goals. In Chapter 44, Section 1, the focus is on establishing a robust public health system, which includes improving mental health and mental health services. Chapter 50, Section 2 aims to enhance care and services for minors, ensuring equitable access to education for children and strengthening mental health education and services specifically tailored to children.
According to the sub-report B2 of China’s National Mental Health Development Report 2021-2022 and the 2022 survey report on adolescent mental health status, it is recommended to enhance the significance of screening for adolescent mental health, establish a hierarchical management system, and emphasize the dissemination of mental health knowledge. These measures aim to achieve early detection, early intervention, and early treatment.
The severity of adolescent psychological issues is progressively escalating due to various factors, including family- related factors, academic stress, environmental changes, school violence, and uncontrollable external influences. The incidence of these problems is increasing annually. Furthermore, the number of suicides and instances of self-harm among adolescents resulting from psychological problems has been consistently rising, becoming the primary factor affecting the healthy development, mortality, or disability among teenagers.
In conclusion, we assert that lowering the suicide and self- harm rates among adolescents with mental disorders necessitates a comprehensive approach, encompassing:
- Early Identification and Intervention: Proactively identify adolescents at risk for suicide and self-harm, offering prompt intervention and support. Parents, educators, and healthcare professionals must monitor behavioral shifts and emotional fluctuations in youths for early problem detection.
- Mental Health Education: Enhance the dissemination of mental health knowledge within schools and communities, empowering teens to grasp mental health’s significance and equip them with skills to recognize and address their emotional issues.
- Psychological Support and Treatment: Deliver specialized psychological counseling and treatment services to needy adolescents, incorporating cognitive-behavioral therapy, family therapy, and pharmacotherapy, ensuring they receive requisite assistance.
- Support Networks: Foster the creation of supportive networks among families, educational institutions, and communities, ensuring a nurturing and safe space for youngsters. Facilitate constructive interactions and mutual support among peers.
- Healthy Lifestyle Promotion: Encourage adolescents to cultivate beneficial lifestyle habits, such as balanced diets, sufficient sleep, and regular physical activity, aiding in stress reduction and enhancing overall well-being.
- Crisis Intervention: Offer crisis intervention services to adolescents, including emergency hotlines and online counseling, to furnish immediate aid and support during crises.
The comprehensive implementation of these measures can effectively reduce the incidence of suicide and self-harm among adolescents with mental disorders, thereby enhancing their overall mental health.
Our study has several primary limitations which are as follows: Firstly, the case information relied on self-reporting or parental descriptions, introducing the potential for subjective biases that could influence our diagnostic accuracy. Secondly, our sample information did not adhere to a normal distribution, necessitating the use of non-parametric rank sum tests to analyze differences in the total number of cases, as well as M7, M8, and M9 before and after the COVID-19 pandemic. This statistical approach may introduce certain degrees of deviation. Thirdly, our study lacked comprehensive data on the impact of lockdown measures on adolescents’ mental health during the COVID-19 pandemic. Consequently, our focus was not solely on the influence of the epidemic on adolescents’ mental health. However, this approach allowed for a more objective and realistic statistical analysis of the COVID-19 pandemic’s impact on adolescent suicide and self- harm behaviors.
CONCLUSION
The COVID-19 pandemic has led to an increase in the prevalence of mental disorders among adolescents, particularly with regards to suicide and self-harm. This can be attributed to heightened family tensions and academic pressures. Our study aims to raise awareness amongst government bodies, society at large, families and schools regarding adolescent mental health issues, as well as provide preliminary guidance on diagnosis, prevention and treatment of psychiatric illnesses.
ACKNOWLEDGEMENTS
Thanks to all the participants in this study for their kind support and coordination.
FUNDING
This study was supported by Local special projects in major health of Hubei Provincial Science and Technology Department (2022BCE054), Key scientific research projects of Hubei polytechnic University (23xjz08A) and Hubei polytechnic University. Huangshi Daye Lake high-tech Zone University Science Park joint open fund project (23xjz04AK).
DATA AVAILABILITY
The processed data was available in the paper, and raw data is freely serviced from first and corresponding author.
DECLARATIONS
Ethics approval and consent to participate
All procedures involving human subjects/patients were approved by the Bioethical Safety Committee of Hubei Polytechnic University (with the license number: BSCHBPU-2023001). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All patients in this study had been informed, and they consented to sharing the data. All participants in this study provided written informed consent or parental consent if under the age of 18.
Informed consent
All participants in this study provided written informed consent or informed parental consent if they were under 18 years of age. The participants in this study who had limited educational background were adequately informed and provided written informed consent through their designated surrogate decision- maker or legally authorized representative (LAR).
Consent for publication
All participants and the authors consented to publish the paper.
REFERENCES
- Collaborators GBDMD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022; 9: 137-150.
- Thornicroft G. Most people with mental illness are not treated. Lancet. 2007; 370: 807-808.
- Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry. 2022; 63: 34-46.
- McIntyre RS. Cognition in psychiatry: population health, clinical, and research implications. CNS Spectr. 2019; 24: 2-3. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019; 6: 211-224.
- Taquet M, Geddes JR, Husain M, Luciano S and Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021; 8: 416-427.
- Watson A, Haraldsdottir K, Biese K, Schwarz A, Hetzel S, Reardon C, et al. Impact of COVID-19 on the physical activity, quality of life and mental health of adolescent athletes: a 2-year evaluation of over 17 000 athletes. Br J Sports Med. 2023; 57: 359-363.
- Sun Y, Wu Y, Fan S, Dal Santo T, Li L, Jiang X, et al. Comparison of mental health symptoms before and during the covid-19 pandemic: evidence from a systematic review and meta-analysis of 134 cohorts. BMJ. 2023; 380: e074224.
- Collaborators GBDAM. Global, regional, and national mortality among young people aged 10-24 years, 1950-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021; 398: 1593- 1618..
- Anderson KN, Swedo EA, Trinh E, Ray CM, Krause KH, Verlenden JV, et al. Adverse Childhood Experiences During the COVID-19 Pandemic and Associations with Poor Mental Health and Suicidal Behaviors Among High School Students - Adolescent Behaviors and Experiences Survey, United States, January-June 2021. MMWR Morb Mortal Wkly Rep. 2022; 71: 1301-1305.
- Cozzi G, Grillone A, Zuliani E, Giangreco M, Zanchi C, Abbracciavento G, et al. Suicide attempts and eating disorders in adolescents, the mental health wave of the second year of the COVID-19 pandemic: A paediatric emergency department perspective. Front Pediatr. 2023; 11: 1078274.
- Jones SE, Ethier KA, Hertz M, DeGue S, Le VD, Thornton J, et al. Mental Health, Suicidality, and Connectedness Among High School Students During the COVID-19 Pandemic - Adolescent Behaviors and Experiences Survey, United States, January-June 2021. MMWR Suppl. 2022; 71: 16-21.
- Liu L, Pollock NJ, Contreras G, Tonmyr L, Thompson W. Prevalence of suicidal ideation among adults in Canada: Results of the second Survey on COVID-19 and mental health. Health Rep. 2022; 33: 13-21.
- Viner R, Russell S, Saulle R, Croker H, Stansfield C, Packer J, et al. School Closures During Social Lockdown and Mental Health, Health Behaviors, and Well-being Among Children and Adolescents During the First COVID-19 Wave: A Systematic Review. JAMA Pediatr. 2022; 176: 400-409.
- Orui M, Saeki S, Harada S, Hayashi M. Practical Report of Disaster- Related Mental Health Interventions Following the Great East Japan Earthquake during the COVID-19 Pandemic: Potential for Suicide Prevention. Int J Environ Res Public Health. 2021; 18.
- Liu J, Chai L, Zhu H, Han Z. COVID-19 impacts and adolescent suicide: The mediating roles of child abuse and mental health conditions. Child Abuse Negl. 2023; 138: 106076.
- Penninx B, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022; 28: 2027-2037.
- Di Vincenzo M. New research on validity and clinical utility of ICD-11 vs. ICD-10 and DSM-5 diagnostic categories. World Psychiatry. 2023; 22: 171-172.
- Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, Reed GM. Three Approaches to Understanding and Classifying Mental Disorder: ICD- 11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychol Sci Public Interest. 2017; 18: 72- 145.
- Xie J, Yan Y, Hong Y, Yang J, Bai M, Xia W, et al. Descriptive and associated risk factors analysis of mental disorders among adolescents in Huangshi, China. Asian J Psychiatr. 2023; 79: 103405.
- Zhang X, Yan Y, Ye Z, Xie J. Descriptive analysis of depression among adolescents in Huangshi, China. BMC Psychiatry. 2023; 23: 176.
- Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021; 398: 1700-1712.