Massive Streptococcus Pyogenes Pleural Empyema: A Case Report
- 1. Department of Pediatrics, Brussels University Hospital, Belgium
- 2. Molecular Bacteriology Laboratory, European Plotkin Institute for Vaccinology, Faculty of Medicine, Free University of Brussels, Belgium
- 3. Tropical Diseases Research Group, Murdoch Children’s Research Institute, Australia
- 4. Department of Paediatrics, University of Melbourne, Australia
Abstract
Aim and Background: Invasive Streptococcus pyogenes infections pose a significant clinical challenge in terms of diagnostic and optimal therapeutic options.
Case description: We report a case of a healthy, well vaccinated, four-year-old boy presenting with a right pneumonia complicated by a large parapneumonic effusion with negative blood culture. The patient had been treated conservatively by IV penicillin with clinical, biological and radiological improvement allowing discharge at day 21 with oral amoxicillin. At day 27, inflammatory syndrome and fever increased again and were associated with a voluminous mediastinal mass. A thoracoscopy was performed and revealed a massive S. pyogenes empyema that has required drainage. The patient recovered after 6 weeks antibiotics treatment.
Conclusion: This unusual evolution of complicated S. pyogenes pneumonia demonstrated how complex clinical care might sometimes be, especially with children.
Clinical significance: Indications of drainages in severe paediatric pleural effusions, including those due to S. pyogenes, vary according to guidelines and are mainly based on expert opinions. Most cases however have a favourable outcome whatever the management might be. Finally, clinical follow up is often characterised by prolonged fever which may, or not, be indicative of therapeutic failure.
Keywords
• Pleural effusion
• Complicated pneumonia
• Group A Streptococcus
• Invasive infection
• Drainage
Citation
Moortgat J, Jourdain S, Mignon C, Smeesters P (2025) Massive Streptococcus Pyogenes Pleural Empyema: A Case Report. Pediatr Child Health 13(2):1351.
INTRODUCTION
Community-acquired pneumonia (CAP) is a common cause of paediatric hospitalization, especially in children under five years old and is mostly due to Streptococcus pneumoniae, Streptococcus pyogenes (S. pyogenes) and Staphylococcus aureus [1,2]. A recent increase of invasive S.pyogenes infections, including pneumonia, has been noted in Europe and elsewhere (USA, Australia) [2-4].CAP can be complicated by parapneumonic effusion. Among those, empyema due to S.pyogenes seems to be more severe and associated with larger effusion, longer hospital stays and longer time before fever resolution despite appropriate antibiotherapy [5-7].Our case illustrates an unusual evolution of a classic case of complicated pneumonia. It highlights the clinical challenges in terms of both appropriate antibiotic therapy and drainage indications for which recommendations differ from country to country and are mainly based on expert opinions.
CASE DESCRIPTION
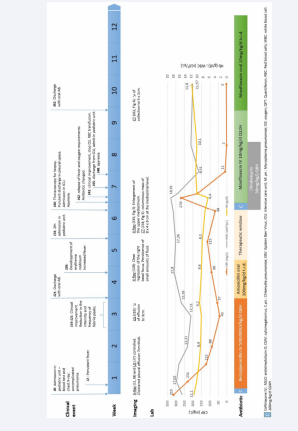
A four-year-old boy, well vaccinated, without any significant medical history presented with fever, abdominal pain and vomiting for 7 days (Figure 1).
Figure 1: Timeline
Neither his non-consanguineous parents nor his one-year-old brother has particular medical history. He had no relevant findings on clinical examination. Additional tests carried out (blood tests, blood cultures, urine, chest X-ray) showed a high inflammatory syndrome with a discrete right basal pulmonary condensation, raising the suspicion of pneumonia. Given the initial diagnostic doubt, broad-spectrum antibiotic coverage with ceftriaxone was initially started, but reduced after 24 hours to penicillin, in line with local antibiotic recommendations for community-acquired pneumonia. Blood cultures were negative. A chest-X-ray was controlled 48 hours after the start of antibiotic due to persistent fever and lack of clinical recovery. A parapneumonic effusion of moderate size had developed.
An ultrasound made one week after the admission showed a large, cloistered effusion measuring 7.86cm thick at the basal level in the sitting position. A conservative treatment with antibiotic alone was decided because of improved clinical status, decreases CRP levels and lack of oxygen requirement.The clinical evolution continued to be favourable over the next two weeks and the patient was discharged from hospital after three weeks of intravenous penicillin and a shift with oral amoxicillin was started.
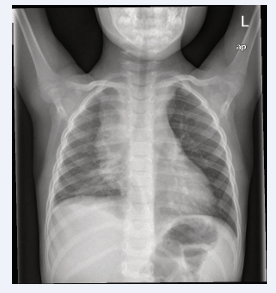
The child had multiple follow-up ambulatory visits. Erythema nodosum appeared on his two legs one week after discharge and he was complaining of intermittent fever until 39°C. During these two weeks after discharge, the inflammatory syndrome progressively increased. Additional blood tests showed negative responses for QuantiFERON, Mycoplasma and Chlamydia while antistreptolysin O were positive 1104UI/ml (N<240), and both EBV and CMV were IgG positive-IgM negative. A chest X-ray showed an enlargement of the upper mediastinum (Figure 2).
Figure 2: Chest X-ray J34, enlargement of the upper mediastinum.
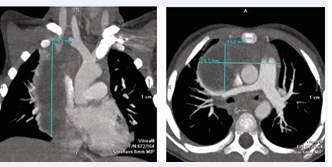
The chest CT demonstrated a voluminous mass of 8x4x9cm at the mediastinal level occupying both the middle, anterior and posterior part of the mediastinum (Figure 3).
Figure 3: Chest CT J34, voluminous mass at the mediastinal level,before drainage.
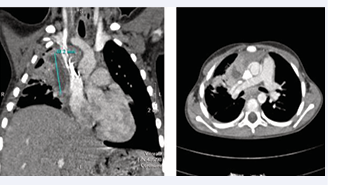
A malignant tumor (lymphoma or germ cell tumor), could not be excluded on the sole basis of radiological images. A right thoracoscopy was then organized for biopsy. During the procedure, an abundant purulent discharge was observed in the pleural space. A chest tube was placed, and the child was admitted to the paediatric intensive care unit. An antibiotherapy was started with IV ceftriaxone and IV clindamycin. Thirty-six hours after surgery, the patient developed high fever, asthenia and oxygen requirements. Antibiotherapy was switched for IV moxifloxacin and IV clindamycin. The child clinically improved from the 3rd day, with discontinuation of oxygen requirement at D3, chest tube removal at D4, and apyrexia at D8. Bacteriological analysis of the peroperative pleural pus showed negative aerobic and anaerobic culture, as well as negative Streptococcus pneumoniae PCR and GeneXpert. On the contrary, a 16S pan-bacterial PCR of this pleural pus came back positive for S. pyogenes.IV moxifloxacin and clindamycin were continued for two weeks and a shift with oral moxifloxacin alone was then started. The patient was discharged three weeks after surgery with a chest CT showing a clear reduction of the mediastinal collection (Figure 4). Oral moxifloxacin was stopped after 6 weeks.
Figure 4: Chest CT J62, reduction in empyema size, 22 days after drainage and resumption of antibiotics.
The child had an overall favourable follow-up outcome, albeit with partial sequellar paralysis of the right diaphragmatic dome and several areas of atelectasis.3 months after stopping all antibiotic therapy, he developed a new right basal pneumonia without effusion, with a good response after 7 days of amoxicillin (including 72 hours IV). Laboratory tests to exclude an immune deficit were performed (immunoglobulin level, lymphocyte typing, complement pathway, vaccine responses) and found to be normal. His 1-year follow-up showed normal pulmonary auscultation and no recurrence of pulmonary infection.
DISCUSSION
We here present a case of a large S. pyogenes loculated empyema, initially treated conservatively with antibiotics just over 4 weeks, but marked with development of a second massive empyema requiring surgical drainage (Figure 1).
As confirmed by available guidelines, different managements for parapneumonic effusion are possible: conservative treatment (antibiotic alone with or without pleural tap), pleural drainage with or without fibrinolytic and finally, surgical intervention (Table 1) [8-12]. Moreover, treatment recommendations are mainly based on expert opinion and not on high quality RCT which explain their divergences [5,13].
|
Drainage (+) or not (-) |
BTS (2005) (8) |
PIDS (2011) (9) |
CPS (2018) (11) |
SBIMC (2020) |
de Benedictis, Lancet (2020)(10) |
|
Respiratory distress, ill- appearing |
+ |
+ |
+ |
+ |
+ |
|
Small effusion |
- |
- |
- |
- |
- |
|
Moderate effusion without loculation |
+ or - |
+ or - |
NS |
- |
- |
|
Large effusion without loculation |
+ or - |
+ |
+ |
+ |
- |
|
Moderate effusion with loculation |
+ |
+ or - |
NS |
- |
+ |
|
Large effusion with loculation |
+ |
+ |
+ |
+ |
+ |
To drain or not to drain?
The concerns about conservative treatment are the risk of respiratory distress and/or pulmonary sequalae, bacterial dissemination and slower clinical recovery [8,14]. However, in contrast to adults where mortality is typically 20%, empyema in children has a very low mortality rate and several studies demonstrated a good outcome regardless of treatment [15,16]. The majority of current guidelines prone pleural drainage for patients with respiratory distress, if there is no improvement with conservative treatment, if empyema is confirmed (parapneumonic effusions with gram/culture +) and, sometimes, in those containing loculation [2,8-12]. Of note, the presence of loculations seems correlated with empyema although high-quality studies assessing the impact on clinical outcome are still missing [16,17].
A retrospective study from the Seattle Children’s Hospital including 182 previously healthy patients with moderate to large pleural effusion has conservately treated 52% of their patients [14]. Selective criteria for such conservative management was clinical stability at admission with improvement within 72 hours of intravenous antibiotics. Among them, a single patient (1/95) required readmission for drainage. On the contrary, major predictors for pleural drainage were: severely ill patients with intensive care unit needed (OR 9.7;95% CI 3.2-29.1), mediastinal shift (OR 5.7;95% CI 2.6-12.1) and large pleural effusions (>½ thorax) (OR 5;95% CI 2.6-9.2). Nevertheless, 34% of patient treated conservatively had a large effusion. Given that the size of the effusion is correlated with the presence of symptoms, most effusions drained for respiratory distress are large, but size alone is not always a criterion for drainage [9]. The presence of loculation was not a predictor for pleural drainage in this study (OR 1.2;95% CI 0.97-1.4).
A prospective paediatric trial in Toronto analysed the long-term outcome of empyema on 82 patients among which 38% (31/82), were treated conservatively [15]. A single patient (1/31) required readmission for drainage. Among the 51 patients initially drained, 6 (12%) were re-hospitalized during the first month (half for pneumothorax and half for persistent pleural effusion). The 12 months follow-up period highlighted that the excellent long-term results were independent of the initial therapeutic approach. It also confirmed that persistent fever and cough were frequent during the first month.
Our patient presented a large loculated effusion at day 7, and since all guidelines usually recommend drainage in such case, we question whether the clinical evolution of our patient might have been better with initial drainage. However, the actual state of the art shows the complexity of such decision process in which all treatment options are overall associated with favourable outcome. Moreover, drainage remains an invasive procedure that can be associated with side effects.
Optimal antibiotic regimen in empyema?
Concerning antibiotics, all guidelines agree that antibiotic regimen should be guided by clinical aspect (mainly whether to cover Staphylococcus aureus) and local epidemiology with focus on penicillin-resistant Streptococcus pneumoniae and MRSA prevalence [8-11]. Guidelines usually do not comment much on S.pyogenes related antibiotic questions due to lower incidence of this bacterium compared to Streptococcus pneumoniae. This may need revision in the light of current upsurge of invasive S. pyogenes infections [2-4].
Penicillin is the drug of choice for S.pyogenes and the recommendation for severe S. pyogenes infection is the use of beta-lactams in combination with clindamycin [18,19]. No resistance of S. pyogenes against penicillin has currently been found. Nevertheless, when there is a massive inoculum, which was undoubtedly present in our clinical case, a lot of bacteria are in a stationary state, therefore reducing beta-lactams efficacy [19]. Clindamycin, which in our case was added directly after drainage, acts in synergy to beta-lactam to reduce the bacterial load and the inoculum effect. Moreover, clindamycin has a good tissue penetration and inhibits proteic virulence factors such as DNases and superantigens [19,20]. In our case, it is however possible that the aetiologic S.pyogenes was clindamycin resistant since around 5% are clindamycin resistant in Belgium [21]. Immunoglobulin has been shown to reduce mortality in S. pyogenes toxic shock syndrome but no data are available regarding their effect of empyema [19].
At first admission, our patient might have evolved better if either clindamycin or immunoglobulin were added as adjunctive therapies but we did not expect S.pyogenes to be the probable aetiology and microbiological workout was negative. At the time of readmission, we may have been too prompted in switching cephalosporin by quinolones at D2 post drainage since the patient clinical improved at D3. On the contrary, the excellent tissue penetration of the quinolone may explain the improvement as well after the introduction of Moxifloxacin in this large empyema [22,23].
CONCLUSION
This unusual evolution of complicated S. pyogenes pneumonia demonstrated how complex clinical care might sometimes be, especially with children.
Clinical Significance
This case reminds us that, even in a common pathology such as pneumonia, patient follow-up is essential to ensure complete recovery. When pneumonia evolves with empyema, it is common for children to remain febrile despite adequate antibiotics. Other clinical and/ or biological criteria need then to be monitored to differentiate between a normal evolution and a potential therapeutic failure. In addition, this case highlights the fact that, although recommendations are a guide to ensure that our management is as evidence-based as possible, they must always be critically appraised, and that a patient centred approach should prevail.
List of abbreviations
CAP:community-acquired pneumonia;CT: computed tomography;IV: intravenous; PCR: polymerase chain reaction
Declaration page
Patient consent for publication: Consent was obtained from the parent for the purpose of publication.
Author contribution
JM, SJ and PRS have been involved in patient management. JM wrote the first draft of the report while SJ, CM and PRS substantially improved it. All authors approved the last version of the manuscript.
Conflict of interest:There is no conflict of interest.
Sources of funding
This paper received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- James Cherry GJD-H, Sheldon L. Kaplan, William J. Steinbach, Peter J Hotez. Textbook of Pediatric Infectious Diseases. 8th edition ed: Elsevier; 2019.
- Ibrahim A Janahi KF. Management and prognosis of parapneumonic effusion and empyema in children. 2021
- Liese JG, Schoen C, van der Linden M, Lehmann L, Goettler D, Keller S, et al. Changes in the incidence and bacterial aetiology of paediatric parapneumonic pleural effusions/empyema in Germany, 2010-2017: a nationwide surveillance study. Clin Microbial Infect. 2019; 25: 857- 864.
- World Health Organization. Increase in invasive Group A streptococcal infections among children in Europe, including fatalities: WHO; 2022
- Megged O. Characteristics of Streptococcus pyogenes Versus Streptococcus pneumoniae Pleural Empyema and Pneumonia with Pleural Effusion in Children. Pediatr Infect Dis J. 2020; 39: 799-802.
- Al-Kaabi N, Solh Z, Pacheco S, Murray L, Gaboury I, Le Saux N. A Comparison of group A Streptococcus versus Streptococcus pneumoniae pneumonia. Pediatr Infect Dis J. 2006; 25: 1008-1012.
- Del Rosal T, Caminoa MB, González-Guerrero A, Falces-Romero I, Romero-Gómez MP, Baquero-Artigao F, et al. Outcome of Severe Bacterial Pneumonia in the Era of Pneumococcal Vaccination. Front Pediatr. 2020; 8: 576519.
- Balfour-Lynn IM, Abrahamson E, Cohen G, Hartley J, King S, Parikh D, et al. BTS guidelines for the management of pleural infection in children. Thorax. 2005; 60: i1-21.
- Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011; 53: e25-76.
- de Benedictis FM, Kerem E, Chang AB, Colin AA, Zar HJ, Bush A. Complicated pneumonia in children. Lancet (London, England). 2020; 396: 786-798.
- Chibuk T, Cohen E, Robinson J, Mahant S, Hartfield D. Paediatric complicated pneumonia: Diagnosis and management of empyema 2018.
- Groupe de travail des infections des voies respiratoires inférieures. Epanchement pleural infectieux et empyème thoracique: Société belge d’infectiologie et de microbiologie Clinique. 2019.
- Erlichman I, Breuer O, Shoseyov D, Cohen-Cymberknoh M, Koplewitz B, Averbuch D, et al. Complicated community acquired pneumonia in childhood: Different types, clinical course, and outcome. Pediatr Pulmonol. 2017; 52: 247-254.
- Carter E, Waldhausen J, Zhang W, Hoffman L, Redding G. Management of children with empyema: Pleural drainage is not always necessary. Pediatr Pulmonol. 2010; 45: 475-480.
- Cohen E, Mahant S, Dell SD, Traubici J, Ragone A, Wadhwa A, et al. The long-term outcomes of pediatric pleural empyema: a prospective study. Arch Pediatr Adolesc Med. 2012; 166: 999-1004.
- Calder A, Owens CM. Imaging of parapneumonic pleural effusions and empyema in children. Pediatr Radiol. 2009; 39: 527-537.
- Islam S, Calkins CM, Goldin AB, Chen C, Downard CD, Huang EY, et al. The diagnosis and management of empyema in children: a comprehensive review from the APSA Outcomes and Clinical Trials Committee. J Pediatr Surg. 2012; 47: 2101-2110.
- Johnson AF, LaRock CN. Antibiotic Treatment, Mechanisms for Failure, and Adjunctive Therapies for Infections by Group A Streptococcus. Front Microbiol. 2021; 12: 760255.
- Laho D, Blumental S, Botteaux A, Smeesters PR. Invasive Group A Streptococcal Infections: Benefit of Clindamycin, Intravenous Immunoglobulins and Secondary Prophylaxis. Front Pediatr. 2021; 9: 697938.
- Walker AW, Hoyles L. Human microbiome myths and misconceptions. Nature Microbiol. 2023; 8: 1392-1396.
- Hospital AU. Report 2021. National reference centre for invasive B-hemolytic streptococci non group B. 2021.
- Rodvold KA, Neuhauser M. Pharmacokinetics and pharmacodynamics of fluoroquinolones. Pharmacotherapy. 2001; 21: 233s-52s.
- Jager NGL, van Hest RM, Lipman J, Roberts JA, Cotta MO. Antibiotic exposure at the site of infection: principles and assessment of tissue penetration. Expert Rev Clin Pharmacol. 2019; 12: 623-634.