Magnitude of Syphilis and Associated Factors among Pregnant Women attending Antenatal Care at Hawassa Zuria Woreda Public Health Facilities, Sidama, Ethiopia, 2024
- 1. School of Public health, Pharma College, Ethiopia
- 2. Sidama regional state health bureau, Ethiopia
- 3. Yirgalem Hospital Medical College, Ethiopia
Abstract
Introduction: Syphilis is a sexually transmitted infection caused by the Bacterium Treponema pallidum, and continues to be a major public health problem worldwide. It can spread through various means such as unprotected sex, mother-to-fetus, and blood transfusion. Mother-to-child transmission of syphilis during pregnancy can result in adverse pregnancy outcomes, such as early fetal death, stillbirth, premature birth, and low birth weight Despite widely available and affordable screening methods and treatment, syphilis infection is a public health problem in pregnant women in sub-Saharan Africa. This study aimed to assess the magnitude of syphilis and its associated factors among pregnant women attending antenatal care at public health facilities in Hawassa Zuria Woreda, Sidama, Ethiopia.
Methods: A facility-based cross-sectional study was conducted in Hawassa Zuria public health facilities from November 1-30, 2024. A total of 482 participants were selected using systematic sampling methods. Data were collected through structured interviews using a pre-tested questionnaire and by reviewing the records. Epi-data version 4.4 was used to code and enter the data, and SPSS version 26 was used for analysis. Bivariable logistic regression was employed to identify candidate variables for multivariable logistic regression with a significance level of ≤ 0.25. A multivariate logistic regression model was used to investigate factors associated with syphilis infection, and a p-value of <0.05 was considered statistically significant.
Results: The magnitude of syphilis among pregnant women attending antenatal care clinics was 3.8% (95% CI: 3.61-3.99). Having multiple sexual partners (AOR = 3.68; 95% CI: 1.22 - 11.11), alcohol use (AOR = 7.34; 95% CI: 2.31 - 23.36), and HIV positive women (AOR = 10.22; 95% CI: 2.03 - 51.53) were significantly associated with syphilis infection.
Conclusion and Recommendation: The magnitude of syphilis was high. Having multiple sexual partners, being HIV-positive, and alcohol consumption were factors significantly associated with syphilis infection. Therefore, substantial efforts have to be made to provide regular health education for pregnant women at antenatal clinics to avoid risky sexual behaviors, raise awareness on the transmission and prevention mechanisms of syphilis, promote safe sexual practices, and strengthen partner testing and treatment.
Keywords
• Syphilis
• Antenatal Care
• Pregnant Women
• Associated Factors
Citation
Aliye A, Doelaso ST, Samuel A (2025) Magnitude of Syphilis and Associated Factors among Pregnant Women attending Antenatal Care at Hawassa Zuria Woreda Public Health Facilities, Sidama, Ethiopia, 2024. Ann Pregnancy Care 7(1): 1020.
INTRODUCTION
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, and continues to be a major public health concern worldwide. It can spread through various means, such as unprotected sex, mother-to fetus, and blood transfusion [1-3]. During pregnancy, there is a specific concern regarding the potential transmission of infection to the fetus through hematogenous spread [4]. Mother-to-child transmission of syphilis during pregnancy can result in adverse pregnancy outcomes, such as early fetal death, stillbirth, premature birth, and low birth weight [5]. Despite widely available and affordable screening methods and treatments, syphilis infection is a public health problem in pregnant women in sub-Saharan Africa [4,6]. Most pregnant women with syphilis are not identified and treated promptly to prevent adverse effects during pregnancy. There is also discrepancies in antenatal care (ANC) availability and syphilis testing rates [1,7]. Approximately 357 million new cases of STIs were reported worldwide in 2015, syphilis accounting for an estimated 12 million cases, including 2 million in pregnant women. Sub-Saharan Africa accounting for 57% of all cases worldwide [8,9]. Approximately 200,000 stillbirths and infant deaths due to congenital syphilis occurred in 2019, making it the second leading cause of preventable stillbirths worldwide [10]. More than half of untreated maternal syphilis cases lead to adverse pregnancy outcomes, such as spontaneous abortion, stillbirth, preterm birth, low birth weight, neonatal death and congenital syphilis [5,11,12]. The World Health Organization (WHO) surveillance report showed that the global seroprevalence of syphilis among pregnant women attending ANC was 0.8%. The prevalence of syphilis in African region was 2% [13]. The overall syphilis seroprevalence among pregnant women attending ANC was 1.9% in Nigeria [14], 3% in Khartoum [15], and 0.9% in Rwanda [16]. Ethiopia is a sub-Saharan African nation that experiences high levels of maternal syphilis and adverse pregnancy outcomes [17]. Studies conducted in Debre Berhan 5.1% [18], Asella 2.4% [19], Jinka 4.8% [20], and South Gonder 3.7% [21], revealed the prevalence of syphilis infection. A complex relationship exists between HIV and syphilis infection. Ulcers associated with clinical syphilis increase the risk of HIV infection [22], whereas the progression of HIV to AIDS has a significant effect on the prognosis of syphilis management, resulting mainly from immunosuppression [23]. The management of STIs resulted in a 38% reduction in HIV infection rate [24]. Studies indicate that factors such as maternal age, residence, socioeconomic status, education level, prenatal care, prostitution, multiple sexual partners, substance use, knowledge about STIs, partners’ educational status, partner occupation, number of pregnancies, history of abortions, history of STIs, HIV/ AIDS status, and access to STI treatment are associated syphilis infection [25-27]. The WHO has set an ambitious plan to reduce syphilis by 90% by 2030 [28]. This target should be supported by regular epidemiological surveillance in high-burden areas to guide intervention [29]. Early diagnosis and treatment of syphilis during pregnancy are widely acknowledged as successful approaches to reduce syphilis transmission and adverse pregnancy outcomes [30,31]. In endemic countries, conducting ANC screening to detect and treat syphilis can result in 82% decrease in stillbirths, 64% decrease in preterm births, and 80% decrease in neonatal deaths [32]. According to the Ethiopian Demographic and Health Survey, ANC visits accounted for 62%, and syphilis screening accounted for 44.6% [33]. However, there is wide variation in the WHO target of fewer than 50 congenital syphilis cases per 100,000 live births, at least 95% coverage at the first ANC visit, 95% syphilis testing, and 95% case treatment [5,11]. Therefore, the objective of this study was to assess the seroprevalence of syphilis and its associated factors among pregnant women at public health facilities in Hawassa Zuria, Sidama, Ethiopia.
METHOD AND MATERIALS
Study area and Period
A facility-based cross-sectional study was conducted in Hawassa Zuria Woreda, Sidama, Ethiopia. It is located 295 km from the capital, Addis Ababa, and 23 km from Hawassa. According to the 2024 Woreda Health Office’s report, the total population is projected to be 182,215, and about 42,456 falls within the reproductive age (15 49) years. There are five public health facilities in Woreda: Dore Bafano Primary Hospital, Dado Health Center, Mekibesa Health Center, Tenkaka Health Center, and Shamena Health Center. The study was conducted from November 1-30, 2024.
Study Design
- Facility based cross-sectional study
Source and Study Population
Source population: All pregnant women attended public health facilities for ANC in Hawassa Zuria Woreda during the study period.
Study population
- Randomly selected pregnant women attending public health facilities for ANC during the study period.
Eligibility criteria Inclusion criteria
- All selected pregnant women attended public health facilities for ANC services in Hawassa Zuria Woreda during the data collection period.
Exclusion criteria
- Pregnant women with mental impairment or critical illnesses at the time of data collection were excluded from this study.
Sample size determination
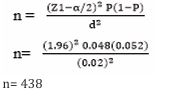
The sample size was calculated using a single population proportion formula, assuming a 95% confidence level,4.8% seroprevalence of syphilis from a study conducted in Jinka Town [20], margin of error 2%, and 10% non response rate.
After adding a 10% non-response rate, the final sample size was 482.
Sampling Methods
The study included five public health facilities offering ANC services in Hawassa Zuria Woreda. By using the previous months ANC flow of pregnant women as a baseline, a total of 975 pregnant women visited public health facilities (Dore Bafano Primary Hospital 284, Shamena Health Center 215, Dado Health Center 133, Tenkaka Health Center 156, and Mekibesa Health Center 187) that fulfilled the eligibility criteria of the study. The number of pregnant women interviewed at each health facility was determined based on proportional allocation to size. Interval (K) was calculated by dividing 975 by a sample size of 482, resulting in two intervals. The lottery method was used to select the first participant for the study at each health facility. Every other pregnant woman was interviewed and a file checkup was conducted.
Data collection and quality control
Data were collected using structured questionnaires, which were prepared by reviewing the relevant literature to address the study objective. Relevant experts reviewed the data collection tool to ensure alignment with the study objectives. Data were collected through exit interviews and document reviews. The data collection tool was pre tested on 5% of the sample at Yirba Primary Hospital one week prior to data collection. Five BSc midwives were appointed as data collectors, and one health officer served as a supervisor. One-day training was provided to the data collectors and supervisor on study purpose, data collection tools, data handling, and maintaining respondents’ confidentiality. Syphilis and HIV serostatus results from the medical records were examined. Pregnant women for whom medical records were unavailable were excluded from the analysis.
Operational Definitions
- Syphilis: - In this study, syphilis was considered when the Rapid Plasma Reagin (RPR) or Venereal Disease Research Laboratory (VDRL) test was reactive for syphilis infection among pregnant women [34].
- Knowledge of STI: - Nine questions were used to assess the level of knowledge. The total score for each study participant was converted to percentage and categorized into those with good knowledge (score ≥50).
- Alcohol drinking: - Consuming alcohol at least once per month in the last 12 months (above the recommended level). This means above 2 bottles for males and one bottle for females [33].
Data Processing and Analysis
Data were coded, entered into Epi-Data version 4.4, and exported to SPSS version 26 for analysis. Data cleaning was performed by running the frequency of each variable to check the accuracy, inconsistency, and missing data values. Variables were checked using the chi-square test to identify the associations between each categorical variable and the dependent variables. Bivariable logistic regression was employed to identify candidate variables for multivariable logistic regression with a significance level of ≤ 0.25. The degree of association between independent and dependent variables was assessed using an odds ratio with a 95% confidence interval and variables with a P-value <0.05 in the multivariable logistic regression model were considered statistically significant. Model fitness was checked using the Hosmer- Lemeshow goodness of fit test, and multicollinearity was assessed using the variance inflation factor method. The value was observed between one and two for all independent variables entered to assess multicollinearity. Descriptive statistics were performed and summarized using text, tables, and graphs based on the type of variable.
Ethical Consideration
Ethical clearance was obtained from the Institutional Research Ethical Review Committee (IRERC) of Pharma College School of Graduate Studies. Permission letters were acquired from the Hawassa Zuria Woreda Health Office and formal letters were written to each health facility from the Woreda Health Office. Informed verbal consent was obtained from each study participant to confirm their willingness to participate, after explaining the objectives of the study. To maintain privacy, each participant was interviewed separately in a quiet room prepared for this purpose. Participants were guaranteed that their responses would remain confidential from both data collectors and supervisor. The collected data were used solely for the purposes of the study, and confidentiality was maintained throughout the study.
RESULT
Socio-demographic characteristics of participants
Approximately 479 pregnant women participated in the study, resulting in a response rate of 99.3%. The mean age of the respondents was 25.95 (± 4.72) years. The majority of the 469(97.9%) participants were married, and 233 (48.6%) attended primary education. More than three-fourths (82.7%) of the pregnant women were rural residents and 288(60.1%) were housewives. More than one-third 173(36.1%) of the participants earned >3000 ETB (Table 1).
Table 1: Socio-demographic characteristics of study participants in Hawassa zuria woreda public health facilities, Sidama, Ethiopia, 2024.
|
Variables |
Category |
Frequency |
Percent |
|
Age category |
18-24 |
201 |
42 |
|
25-29 |
156 |
32.6 |
|
|
30-42 |
122 |
25.5 |
|
|
Marital status |
Married |
469 |
97.9 |
|
Divorced |
3 |
0.6 |
|
|
Widowed |
4 |
0.8 |
|
|
Single |
3 |
0.6 |
|
|
Religion |
Protestant |
439 |
91.6 |
|
Muslim |
23 |
4.8 |
|
|
Orthodox |
12 |
2.5 |
|
|
Residence |
Rural |
398 |
82.7 |
|
Urban |
83 |
17.3 |
|
|
Education |
Non |
91 |
19 |
|
Primary |
233 |
48.6 |
|
|
Secondary |
123 |
25.7 |
|
|
Collage and above |
32 |
6.2 |
|
|
Occupation |
Housewife |
288 |
60.1 |
|
Merchant |
98 |
20.5 |
|
|
Private employee |
30 |
6.3 |
|
|
Government employee |
28 |
5.8 |
|
|
Other |
35 |
7.3 |
|
|
Partners occupation |
Farmer |
294 |
61.4 |
|
Merchant |
63 |
13.2 |
|
|
Private |
48 |
10 |
|
|
Government |
60 |
12.5 |
|
|
Other |
14 |
2.9 |
|
|
Monthly Income (ETB) |
500-1000 |
47 |
9.8 |
|
1001-2000 |
100 |
20.9 |
|
|
2001-3000 |
159 |
33.2 |
|
|
Above 3000 |
173 |
36.1 |
Behavior related characteristics
Approximately 397 (82.9%) study participants had one sexual partner in their lifetime. Fifty-two (10.9%) respondents had a history of alcohol consumption and 13(2.7%) had a history of cigarette smoking (Table 2)..
Table 2: Behavior related characteristics of study participants in Hawassa zuria woreda public health facilities, Sidama, Ethiopia, 2024.
|
Variable |
Category |
Frequency |
Percent |
|
Lifetime sexual partners |
Multiple |
82 |
17.1 |
|
One |
397 |
82.9 |
|
|
Last 12-month sexual partners |
Multiple |
34 |
7.1 |
|
One |
445 |
92.9 |
|
|
Alcohol drinking |
Yes |
52 |
10.9 |
|
No |
427 |
89.1 |
|
|
Cigarette smoking |
Yes |
13 |
2.7 |
|
No |
466 |
97.3 |
Knowledge related characteristics
Among 479 study participants, 261(54.5%), 252(52.2%), 156 (32.6%), and 92(19.2%) of the study
participants got information about STIs from School, Health facilities, Media, and peers/families respectively. About 291 (60.7%) of the study participants were aware of STI transmission, while 362 (75.6%) were unaware of the symptoms of STI. Nearly one-third of the 150 (31.3%) study participants were aware of common types of STI. About half of 239 (49.9%) participants were aware of the prevention of mother-to-child transmission. Approximately 334 (69.7%) participants knew that STIs could be prevented through the use of a condom. About 164 (34.2%) study participants had good knowledge of STI.
Obstetric characteristics of study participants
The majority of study participants 321 (67%) were multigravida and 356 (74.3%) were screened for syphilis in the first trimester. Approximately 265 (55.3%) study participants started ANC visits during the first trimester, and 165 (34.4%) of them had their first ANC visit. About 53 (11.1%) participants reported a history of abortion (Table 3).
Table 3: Obstetric characteristics of study participants in Hawassa zuria woreda public health facilities, Sidama, Ethiopia, 2024.
|
Variable |
Category |
Frequency |
Percent |
|
Pregnancy |
Nulliparous |
158 |
33 |
|
Multigravida |
321 |
67 |
|
|
Syphilis test time |
First trimester |
356 |
74.3 |
|
Second trimester |
81 |
17 |
|
|
Third trimester |
42 |
8.7 |
|
|
First ANC visit |
First trimester |
265 |
55.3 |
|
Second trimester |
159 |
33.2 |
|
|
Third trimester |
55 |
11.5 |
|
|
Number of ANC visit |
First |
165 |
34.4 |
|
Second |
134 |
27.9 |
|
|
Third |
104 |
21.7 |
|
|
Fourth and above |
76 |
15.8 |
|
|
History of Abortion |
Yes |
53 |
11.1 |
|
No |
426 |
88.9 |
Medical characteristics of study participants
About 19(4%) of the study participants had a history of STI, and 11 (2.3%) of the study participants were reactive for HIV. Approximately 16(84.2%) of the study participants were diagnosed with STI before one year (Table 4).
Table 4: Medical-related characteristics of study participants in Hawassa zuria woreda public health facilities, Sidama, Ethiopia, 2024.
|
Variable |
Category |
Frequency |
Percent |
|
History of STI |
Yes |
19 |
4 |
|
No |
460 |
96 |
|
|
Year of diagnosis |
Last 12 months |
3 |
15.8 |
|
Before one year |
16 |
84.2 |
|
|
Treatment |
Oral |
7 |
36.8 |
|
Injection |
12 |
63.2 |
|
|
HIV Sero-status |
Reactive |
11 |
2.3 |
|
Non-reactive |
468 |
97.7 |
|
|
Syphilis |
Reactive |
18 |
3.8 |
|
Non-reactive |
461 |
96.2 |
Factors Associated with Syphilis Serostatus
The magnitude of syphilis determined using the VDRL test was 3.8% (95% CI: 3.61 - 3.99%). In the binary logistic regression analysis, variables such as Age, HIV positivity, multiple sexual partners, and alcohol consumption were candidate variables for multivariable logistic regression analysis. In the multivariate logistic regression analysis, after controlling for possible confounders, pregnant mothers with multiple sexual partners, alcohol consumption, and HIV positivity were significantly associated with syphilis infection.
This study indicated that pregnant mothers with multiple sexual partners were almost four times more likely to have syphilis infection than their counterparts (AOR=3.68, 95%CI: 1.22 - 11.11). Pregnant women who were HIV positive were ten times more likely to have syphilis infection than those who were HIV negative (AOR =10.22, 95%CI: 2.03 - 51.53). The findings also showed that pregnant women who were alcohol users had significantly higher odds of being seropositive for syphilis than those who were non-alcohol drinkers (AOR= 7.34, 95%CI: 2.31- 23.36) (Table 5).
Table 5: Factors associated with seroprevalence of syphilis among of study participants in Hawassa zuria woreda public health facilities, Sidama, Ethiopia, 2024.
|
Variables |
Category |
Syphilis |
COR (95%CI) |
AOR (95%CI) |
|
|
R |
NR |
||||
|
Age |
<25 |
4 |
197 |
1 |
1 |
|
25-29 |
5 |
151 |
1.63(0.43 - 6.18) |
2.00(0.49 - 8.13) |
|
|
30-42 |
9 |
113 |
3.92(1.18 - 13.03) |
3.03(0.82 - 11.17) |
|
|
Alcohol drinking |
Yes |
7 |
45 |
5.88(2.17 - 15.93) |
7.34(2.31 - 23.36) * |
|
No |
11 |
416 |
1 |
1 |
|
|
Number of sexual partners |
One |
9 |
388 |
1 |
1 |
|
Multiple |
9 |
73 |
5.32(2.04 - 13.84) |
3.68(1.22 - 11.11) * |
|
|
HIV Status |
Reactive |
4 |
7 |
18.53(4.86 - 70.67) |
10.22(2.03 - 51.53)* |
|
Non-reactive |
14 |
454 |
1 |
1 |
|
DISCUSSION
This study aimed to assess the magnitude of syphilis and its associated factors among pregnant women attending ANC in Public health facilities in Hawassa Zuria Woreda, Sidama, Ethiopia. The overall seroprevalence of syphilis among pregnant women attending antenatal care was 3.8% (95% CI, 3.61-3.99). This finding was comparable with those of studies conducted in Northwest Gonder (3.7%) [21], and South Africa (3.4%) [35]. However, the findings of this study were lower than those in Southern Ethiopia (4.8%) [20], Zambia (9.3%) [36], and Yirgalem-Ethiopia (5.1%) [37]. This finding is higher than that reported in sub-Saharan Africa (2.3%) [35], Nigeria (1.98%) [38], Bahirdar Ethiopia (2.6%) [39], Yaya Gulele, Oromia Ethiopia (2.6%) [40], and systematic review and meta-analysis, Ethiopia (2.3%) [41]. The difference in the magnitude of syphilis infections may be due to variations in the laboratory diagnostic techniques used. Moreover, a possible reason for the differences in the seroprevalence of syphilis might be the difference in sociodemographic characteristics, study period, sexual practice, and cultural difference across the study population.
Pregnant women with multiple sexual partners were four times more likely to have syphilis infection than their counterparts. This finding is consistent with those of studies conducted in Zambia [36], Bahir Dar, Ethiopia [39], Southwest Shoa, Ethiopia [42], and Southern Ethiopia [20], Shashemene Town, Southern Ethiopia [43]. A possible reason might be that having multiple sexual partners increases vulnerability to STIs, owing to unsafe sexual practices and low-level awareness of STI transmission and prevention methods.
This study showed that pregnant women who had a history of alcohol consumption were approximately seven times more likely to be infected with syphilis than their counterparts. This finding is supported by studies conducted in Southwest Shoa, Ethiopia [42], and Southern Ethiopia [20]. This might be explained by alcohol intake exposing women to unsafe sexual practices, including concomitant multiple sexual partnerships that predispose them to the acquisition of STIs, including syphilis. Furthermore, HIV positive pregnant women were ten times more likely to be infected with syphilis than HIV negative women. This finding is consistent with those of studies conducted in Ethiopia [41], Zambia [36], and Uganda [44].
LIMITATIONS OF THE STUDY
The use of VDRL tests for syphilis screening may have underestimated the results of this study because of their low sensitivity and specificity. The history of sexual habits reported by respondents may have been underestimated or overestimated because of recall bias and cultural taboos. Facility-based design limits generalizability to broader communities.
CONCLUSION
This study showed that the magnitude of syphilis infection among pregnant mothers attending ANC at the Hawassa Zuria Woreda public health facility was 3.8%, which was higher than the national prevalence of syphilis (2.3%). This finding highlights the importance of routine syphilis screening for ANC to prevent adverse outcomes. Our finding indicates that multiple sexual partners, HIV status, and alcohol consumption were significantly associated with syphilis infection. Healthcare workers should provide regular comprehensive health education to pregnant women at ANC clinics to avoid risky sexual behaviors, the impact of syphilis on pregnancy, and awareness of the transmission and prevention mechanisms of syphilis. Appropriate strategies should be developed to prevent and control maternal syphilis infection.
AUTHOR CONTRIBUTIONS
Conceptualization: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel.
Data curation: Akililu Aliye, Amanuel Samuel
Formal analysis: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel
Funding acquisition: Akililu Aliye
Investigation: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel,
Methodology: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel
Project administration: Akililu Aliye, Solomon Tesfaye Doelaso
Resources: Akililu Aliye, Solomon Tesfaye Doelaso
Software: Akililu Aliye, Solomon Tesfaye Doelaso
Supervision: Akililu Aliye, Amanuel Samuel
Validation: Akililu Aliye, Solomon Tesfaye Doelaso,Amanuel Samuel.
Visualization: Akililu Aliye, Solomon Tesfaye Doelaso
Original draft Writing: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel
Review & editing: Akililu Aliye, Solomon Tesfaye Doelaso, Amanuel Samuel
REFERENCES
- Guideline on syphilis screening and treatment for pregnant women. World Health Organization. 2017.
- Kojima N, Klausner JD. An Update on the Global Epidemiology ofSyphilis. Curr Epidemiol Rep. 2018; 5: 24-38.
- Lendado TA, Tekle T, Dawit D, Daga WB, Diro CW, Arba MA, et al. Determinants of syphilis infection among pregnant women attending antenatal care in hospitals of Wolaita zone, Southern Ethiopia, 2020. PLOS ONE. 2022; 17: e0269473.
- Khan S, Menezes GA, Dhodapkar R, Harish BN. Seroprevalence of syphilis in patients attending a tertiary care hospital in Southern India. Asian Pac J Trop Biomed. 2014; 4: 995-997.
- The global elimination of congenital syphilis: rationale and strategy for action. World Health Organization: Geneva. 2007.
- WHO. Global Incidence and Prevalence of Selected Curable Sexually Transmitted Infections. 2012.
- Cooper JM, Sánchez PJ, Congenital syphilis. Semin Perinatal. 2018; 42:176-184.
- Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2017; 312: 1905-1917.
- Dodds F, Donoghue AD, Roesch JL. Negotiating the sustainable development goals: a transformational agenda for an insecure world. Taylor & Francis. 2016: 240.
- Hoque M, Hoque ME, van Hal G, Buckus S. Prevalence, incidence and seroconversion of HIV and Syphilis infections among pregnant women of South Africa. S Afr J Infect Dis. 2021; 36: 296.
- Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes. Estimates for 2016 and progress since 2012. PloS one. 2019; 14: e0211720.
- Befekadu B, Shuremu M, Zewdie A. Seroprevalence of syphilis and its predictors among pregnant women in Buno Bedele zone, southwest Ethiopia: A community-based cross-sectional study. BMJ Open. 2022; 12: e063745.
- WHO. Report on global sexually transmitted infection surveillance 2018. World Health Organization. 2018.
- Isa MA. Prevalence of syphilis among pregnant women attending state specialist hospital Maiduguri, borno, Nigeria. Int J Res. 2014. 1: 523-530.
- Abdelmola AO, Prevalence and factors associated with syphilis among pregnant women attending antenatal care, Khartoum State, Sudan. Int J Adv Med. 2018; 5: 218-223.
- Mutagoma M, Remera E, Sebuhoro D, Kanters S, Riedel DJ, NsanzimanaS. The prevalence of syphilis infection and its associated factors in the general population of Rwanda: a national household-based survey. J Sexually Transmit Dis. 2016; 2016: 4980417.
- Kebede A. Report on the 2014 Round Antenatal Care based Sentinel HIV Surveillance in Ethiopia. The Ethiopia public health institution. 2015.
- Zinabie S, Belachew E, Yidenek T, Lewetegn M, Asfaw T. Sero- Prevalence of Syphilis and HIV and Associated Factors in Pregnant Women Attending Antenatal Care Clinics in Debre Berhan Public Health Institutions, Ethiopia. AJBLS. 2018; 6: 56-62.
- Schönfeld A, Feldt T, Tufa TB, Orth HM, Fuchs A, Mesfun MG, et al. Prevalence and impact of sexually transmitted infections in pregnant women in central Ethiopia. Int J STD AIDS. 2018; 29: 251-258.
- Enbiale M, Getie A, Haile F, Tekabe B, Misekir D. Magnitude of syphilis sero-status and associated factors among pregnant women attending antenatal care in jinka town public health facilities, Southern Ethiopia, 2020. PLOS ONE. 2021; 16: e0257290.
- Yideg Yitbarek G, Ayele BA. Prevalence of Syphilis among Pregnant Women Attending Antenatal Care Clinic, Sede Muja District, South Gondar, Northwest Ethiopia. J Pregnancy. 2019; 2019: 1584527.
- Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004; 4: 456-66.
- Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004; 189: 369-376.
- Ng BE, Butler LM, Horvath T, Rutherford GW. Population-based biomedical sexually transmitted infection control interventions for reducing HIV infection. Cochrane Database Syst Rev. 2011; 3: CD001220.
- Melku M, Kebede A, Addis Z. Magnitude of HIV and syphilis seroprevalence among pregnant women in gondar, northwest ethiopia: a cross-sectional study. HIV/AIDS. 2015; 7: 175-182.
- Endris M, Deressa T, Belyhun Y, Moges F. Seroprevalence of syphilis and human immunodeficiency virus infections among pregnant women who attend the University of Gondar teaching hospital, Northwest Ethiopia: a cross sectional study. BMC Infect Dis. 2015; 15: 111.
- Tsimis ME, Sheffield JS. Update on syphilis and pregnancy. Birth Defects Res. 2017; 109: 347-352.
- WHO. Global health sector strategy on sexually transmitted infections2016-2021: Toward ending STIs. 2016.
- Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLoS One. 2015; 10: e0143304.
- Wijesooriya NS, Rochat RW, Kamb ML, Turlapati P, Temmerman M, Broutet N, et al. Global burden of maternal and congenital syphilis in 2008 and 2012: a health system modelling study. The Lancet Global Health. 2016; 4: 525-533.
- US Preventive Services Task Force; Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening for syphilis infection in pregnant women: US Preventive Services Task Force reaffirmation recommendation statement. Jama. 2018; 320: 911-917.
- Blencowe H, Cousens S, Kamb M, Berman S, Lawn JE. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health. 2011; 11: S9.
- CSA. Ethiopian Demographic and Health Survey report. 2016. The Central Statistical Agency.
- Balla E, Donders GGG. Features of syphilis seropositive pregnant women raising alarms in Hungary, 2013–2016. Eur J Obstet Gynecol Reprod Biol. 2018; 228: 274-278.
- Hussen S, Tadesse BT. Prevalence of Syphilis among Pregnant Women in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Biomed Res Int. 2019; 2019: 4562385.
- Sakala J, Chizuni N, Nzala S. A study on usefulness of a set of known risk factors in predicting maternal syphilis infections in three districts of Western Province, Zambia. Pan Afr Med J. 2016; 24: 75.
- Amsalu A, Ferede G, Assegu D. High seroprevalence of syphilis infection among pregnant women in Yiregalem hospital southern Ethiopia. BMC Infectious Dis. 2018; 18: 109.
- Opone CA, Abasiattai A, Utuk NM, Bassey EA The prevalence of syphilis in pregnant women in Akwa Ibom State, Southern Nigeria. Trop J Obstet Gynaecol. 2019; 36: 224-231.
- Tareke K, Munshea A, Nibret E. Seroprevalence of syphilis and its risk factors among pregnant women attending antenatal care at Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia: a cross- sectional study. BMC Res notes. 2019; 12: 69.
- Negashu D, Geredew G, Kabe D, Guta A, Gizaw S. Syphlis and associated factors among pregnant women attending ANC at Yaya Gulele district public helath facility Oromia, Ethiopia. HAJHBS. 2024; 1: 31-37.
- Geremew H, Geremew D. Sero-prevalence of syphilis and associated factors among pregnant women in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2021; 10: 223.
- Chuko BM, Kibrat FA, Gari ZS, Tafese A, Girma T, Marami SN, et al. Deteminats of syphlis among pregnant women attending ANC at public hospital in south west shoa, Ethiopia 2023. J Women Health Gynecol. 2024: 4.
- Beriso JA, Kitila FL, Ferede A, Kaso AW. High seroprevalence of syphilis infection among pregnant women in Public Health facilities in Shashemene town, southern Ethiopia. Clin Epidemiol and Global Health. 2023; 21: 101288.
- Simiyu A, Atuheire CGK, Taremwa M, Ssali SN, Mwiine FN, Kankya C, et al. Sero-prevalence of syphilis and associated risk factors among pregnant women attending antenatal care at an urban-poor health centre in Kampala, Uganda: a cross-sectional study. Pan Afr Med J. 2024; 47: 129.