Scar Pregnancy: A Case Report with Balloon Treatment
- 1. Unit of Obstetrics and Gynecology, Azienda Ospedaliero-Universitaria di Ferrara, Italy
- 2. Unit of Obstetrics and Gynecology, AUSL della Romagna, St. Maria delle Croci Hospital, Italy
Abstract
Background: Cesarean scar ectopic pregnancy is a serious condition requiring prompt intervention. While some patients may be asymptomatic, symptoms can include severe abdominal pain, vaginal bleeding, and, in severe cases, uterine rupture, hemoperitoneum, and Disseminated Intravascular Coagulation (DIC). The primary risk factor is a previous cesarean section, though other factors such as impaired wound healing from preterm cesarean sections or infections like chorioamnionitis can also increase risk. Although less common, this condition can occur following uterine procedures such as myomectomy or curettage. At present, no specific guidelines exist for managing cesarean scar ectopic pregnancies, and treatment strategies are often adapted from protocols for other ectopic pregnancies.
Methods/Results: We present the case of a 29-year-old woman who reported irregular spotting and vaginal bleeding lasting 7 days. Her medical and surgical history was otherwise unremarkable, except for a previous cesarean section at 37 weeks due to fetal distress during induction for an IUGR fetus with trisomy 21. Diagnosis revealed a gestational sac at the site of the previous surgical scar with embryonic echoes. Non-surgical treatments such as intramuscular Methotrexate and a single oral dose of 600 mg Mifepristone were unsuccessful. We then approached the double-balloon technique (CRB balloon, Cook) under spinal anesthesia in the operating theatre, using ultrasound guidance. The procedure was completed without complications.
Conclusion: Follow-up included monitoring serum Beta-human Chorionic Gonadotropin (β-hCG) levels until they returned to non-pregnant levels, and an ultrasound at 30 days confirmed the resolution of the pregnancy. Sharing cases like this, along with the different approaches and outcomes, may help in developing practical guidelines for managing cesarean scar ectopic pregnancies.
Keywords
• Scar pregnancy
• Caesarean section
• Non-surgical treatment
Citation
Rosignoli B, Lostritto F, Piccolotti I, Caroli M, Catania F, et al. (2025) Scar Pregnancy: A Case Report with Balloon Treatment. Ann Pregnancy Care 7(1): 1017.
LITERATURE REVIEW
Cesarean Scar Pregnancy (CSP) is a rare but increasingly recognized form of ectopic pregnancy, with reported incidence ranging from 1 in 1,800 to 1 in 2,500 pregnancies [1-11]. However, its true prevalence is likely underestimated due to frequent misdiagnosis as a cervical pregnancy or incomplete miscarriage. The global rise in cesarean section rates is contributing to a parallel increase in CSP cases [9,10].
Risk Factors- The primary risk factor for CSP is a history of cesarean delivery, particularly when associated with poor healing of the uterine incision. Additional risk factors include:
- Preterm cesarean sections
- Labor dystocia or fetal malpresentation
- Infections such as chorioamnionitis
- Previous uterine surgeries, including myomectomy, curettage, and hysteroscopic procedures [1-8].
Anatomically, CSP involves the implantation of the gestational sac within the myometrial defect at the cesarean scar, often associated with thinning of the myometrium between the sac and the bladder [11].
Treatment Strategies- There are no universal guidelines for CSP management, and treatment is typically individualized based on gestational age, hemodynamic status, and imaging characteristics (e.g., sac size, vascularity, embryonic activity). The 2017 systematic review by Maheux-Lacroix et al. [4], is the most comprehensive to date, analyzing 63 studies and comparing medical, surgical, and combined therapies.
Medical treatment
- Systemic Methotrexate (MTX), often used alone or combined with oral Mifepristone or local injections of MTX or potassium chloride (KCl), is the most common medical approach.
- Success rates reported
o 56% for systemic MTX
o 60% for local injection
o 77% for combined approaches
- Treatment failure is more likely in the presence of cardiac activity or high vascularity on Doppler imaging [11,14].
Surgical treatment
- Includes dilation and curettage (D&C), hysteroscopic resection, laparoscopic or open excision, and in critical cases, hysterectomy.
- Preoperative Uterine Artery Embolization (UAE) is frequently used to reduce hemorrhagic risk.
- D&C is typically reserved for early gestations (< 7 weeks), while hysterectomy is indicated for hemodynamically unstable patients [4-12].
Combined treatment
- Typically consists of systemic MTX followed by D&C or hysteroscopic resection within a week.
- This approach offers higher efficacy (up to 87% success) and minimizes the need for repeat interventions.
- Potential complications include infection, elevated liver enzymes, uterine perforation, and bone marrow suppression.
Novel/conservative approaches
- Double-balloon tamponade [13], has been proposed as a minimally invasive alternative, especially in stable patients after medical treatment failure. Preliminary reports suggest safety and effectiveness, but data remain limited.
CASE PRESENTATION
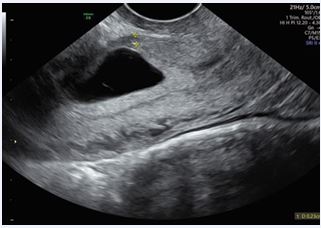
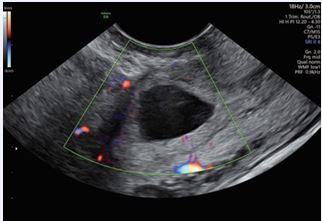
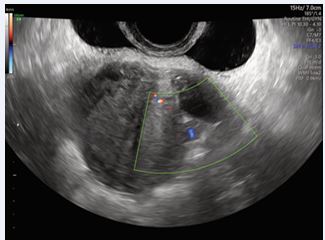
A 29-year-old female presented to our Obstetric Emergency Unit with the main complaint of irregular spotting and vaginal bleeding lasting 7 days. Her medical and surgical history was unremarkable. In her obstetric history, she had undergone a cesarean section at 37 weeks due to fetal distress during induction for an IUGR fetus with trisomy 21. Upon examination, there were no general concerns. At speculum assessment, the cervix appeared normal, with no discharge, and minimal residual uterine bleeding was noted in the vagina. On bimanual examination, the cervix was upward-pointing, the uterus was bulky and anteverted, and the bilateral fornixes were free and non tender. Laboratory tests revealed normal results, with hemoglobin levels within the reference range. A positive β-hCG test indicated a level of 7118 IU/L, which rose to 14,452 IU/L after 48 hours, showing less than a doubling effect. Transvaginal ultrasound performed in the emergency unit showed an empty uterine cavity with clearly defined endometrium. A small, irregular gestational sac-like structure corresponding to five weeks was identified in the lower uterine segment anteriorly, with a vitelline sac and a small embryo without cardiac activity. Both adnexa were normal, and no free fluid was observed in the Douglas pouch. Doppler imaging confirmed the diagnosis of a cesarean scar ectopic pregnancy, revealing excessive vascularity in the hyperechoic rim of the choriodecidual reaction. Ultrasound findings were later corroborated by expert sonographers, with no signs of uterine dehiscence or rupture. Initial management involved monitoring clinical signs and serial β-hCG levels. The patient was asymptomatic, and after thorough counseling regarding pregnancy outcomes (expectant management versus pregnancy interruption), she decided for interruption. Intramuscular Methotrexate was then administered (50 mg/ im). By Day 3, a significant increase in β-hCG levels (22,797 IU/L) and enlargement of the gestational sac (19x17 mm) prompted the decision to administer a single oral dose of 600 mg Mifepristone. Unfortunately, this approach failed to terminate the pregnancy (Figures 1-3). By Day 5, ultrasound imaging confirmed the presence of an embryo with cardiac activity. After additional counseling, the patient consented to a further intervention.
Figure 1: Transvaginal ultrasound - Anteverted and anteflexed uterus, normal in size and regular in morphology with heterogeneous myometrial echotexture consistent with diffuse uterine fibromatosis.
Figure 2: Transvaginal ultrasound- Color Doppler imaging shows vascularization surrounding the gestational sac.
Figure 3: Transvaginal ultrasound - on the previous hysterotomy scar, a single gestational sac is confirmed, measuring 19 × 17 mm, containing a yolk sac and a single embryo with a crown-rump length (CRL) of 2 mm and positive cardiac activity (FHR present).
PROCEDURE
We performed a non-surgical treatment using the double-balloon technique (CRB balloon, Cook) under spinal anesthesia in the operating theatre, with ultrasound guidance. The expert surgeon and blood bank were pre alerted in case of massive hemorrhage or uterine rupture. Vaginal disinfection was achieved using Betadine surgical solution. A speculum was inserted to expose the cervix,and a catheter was placed in the uterine cavity using ring forceps. The first balloon was positioned in the uterine fundus and inflated. During inflation of the second balloon, the gestational sac was compressed. Both balloons were inflated with 20 mL of saline. A small extrusion of the balloon distended the uterine surface at the scar zone, so the balloon was deflated by 10 mL. The patient was monitored for 24 hours with no symptoms or discomfort reported. β-hCG levels dropped significantly to 8133 IU/L, and the CRB balloon was removed under ultrasound guidance. The gestational sac was no longer visible, and no free fluid was noted in the Douglas pouch. Follow-up included monitoring β-hCG levels until they reached non-pregnant levels. An ultrasound at 30 days showed a normal uterine cavity with a regular endometrial lining (Figures 4,5).
Figure 4: A stable area of myometrial heterogeneity is visualized in the anterior wall compared to the previous examination. No intrauterine gestational sac is identified.
Figure 5: The vascularity appears reduced in comparison to earlier scans, suggesting decreased trophoblastic activity.
DISCUSSION
Caesarean scar pregnancy (CSP) refers to placental implantation on or in the scar of a previous caesarean section and represents [1] potentially life-threatening situation for the woman who is affected and should be treated as early as possible. In most of the cases, patient is asymptomatic, but often she may present with severe abdominal pain, vaginal bleeding and, more severely, with sudden rupture of the uterus, hemoperitoneum and disseminated intravascular coagulation (CID) [1-4]. The actual incidence of this rare condition is not well known, as a significant number of cases are misdiagnosed (confused with cervical ectopic pregnancy or ongoing miscarriage of a proper intrauterine pregnancy).Diagnosis is primarily made via ultrasound, revealing a gestational sac [11] implanted in the lower uterine segment at the site of a previous caesarean scar, with intramural development. This condition may be associated with thinning of the myometrium between the gestational sac and the bladder [5]. Diagnostic accuracy is highest in the early first trimester, and color Doppler imaging can be particularly useful in confirming the presence of peritrophoblastic blood flow along the anterior uterine wall [3]. Although the main risk factor associated with the onset of this situation is a previous cesarean section [10,11], there are also other identified risk factors. Any situation that involves impaired healing of the hysterotomy wound, such as a preterm cesarean section, surgery for breech presentation, or after the arrest of the first stage of labor or in the presence of infections (such as chorioamnionitis), can increase the risk. It is less common following interventions on the uterus, such as myomectomy, curettage, or hysteroscopies [1]. There are no specific guidelines outlining the management of cesarean scar ectopic pregnancy [1] many of the methods described in the literature have been adapted by considering various treatment protocols for other ectopic pregnancies. However, in 2017, a systematic review of the literature was conducted to describe the efficacy and safety of treatment options. The review considered one treatment effective if no further treatment were required subsequently. Out of 1,257 identified citations, 63 studies were deemed eligible and analyzed [4].Medical treatment: It evaluated the systematic injection of MTX, the injection of MTX and KCL into the gestational sac, and less commonly, oral mifepristone. Medical therapy was considered for hemodynamically stable patients with a success rate of 56%, 60%, and 77% for systemic, local, and combined treatment, respectively. The most common indication for additional treatment was insufficient decrease in BetaHCG levels. Local KCL injection and/or aspiration of the ectopic pregnancy were also described in cases of heterotopic pregnancy.Surgical treatment includes D&C, hysteroscopy, and vaginal, laparoscopic, or open excision of Cesarean Scar Pregnancy (CSP), and finally hysterectomy. D&C is usually performed under ultrasound guidance, as is hysteroscopy. Hysterectomy is indicated in cases of hemodynamically unstable patients. To reduce the risk of bleeding, additional measures such as Foley catheter insertion into the uterine cavity, local injection of vasopressin or anesthetic before excision can be employed. The primary cause for further treatment is bleeding, except for hysteroscopy where it is the persistence of trophoblastic tissue. Uterine Artery Embolization (UAE) is usually performed before surgical treatments to minimize the risk of bleeding and is associated with a success rate around 93%.Combined treatment: Typically involves systemic MTX followed, after about a week, by D&C or hysteroscopic or laparoscopic resection. Some side effects may include infections and fever, elevated liver enzymes, uterine perforation (< 1%), and bone marrow suppression. Success rates hover around 87%.Finally, expectant management can expose the woman to a high risk of bleeding and subsequent hysterectomy. Although medical treatment with methotrexate may be the preferred option [14], it often faces failure, frequently requiring a second dose of the treatment, which comes with a higher quantity of side effects and an equal rate of failure [4,6,7].Increased vascularity on Doppler, a large gestational sac, and the presence of cardiac activity are indicators for higher treatment failure. Curettage has been associated with greater success in cases of early pregnancies before 7 weeks. The combined treatment of curettage (C) and uterine artery embolization (UAE) has a higher success rate and a lower risk of bleeding compared to D&C alone [1].Several treatments are possible for CSP, and the choice depends on the type of CSP [12], hemodynamic stability, vascularity, gestational age, and the skills of the medical team. Patients should be informed that continuing the pregnancy can pose a risk to their lives. Surgical treatment has a high success rate but increases the risk of side effects such as bleeding and even hysterectomy. Therefore, careful counseling and a thorough assessment of the woman’s characteristics and the environment providing care are recommended.
CONCLUSIONS
Caesarean scar ectopic pregnancies can have very fatal and poor outcomes, including uterine rupture, massive hemorrhage and maternal death [1-4]. Thus, it is important that early and accurate diagnosis of Caesarean scar pregnancy is obtained in order to avoid complications and preserve fertility. Reporting successful balloon treatments is useful to increase awareness [13] and obtain data for larger studies.
Author Contributions: B.R., F.C., M.C and T.A. clinically managed the patient; B.R. wrote the manuscript—original draft, preparation; I.P. contributed to the drafting of the manuscript and the collection of data, T.A reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Data Availability Statement: The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding authors.
Conflicts of Interest: The authors declare no conflict of interest.
REFERENCES
- Sadeghi H, Rutherford T, Rackow BW, Campbell KH, Duzyj CM, Guess MK, et al. Cesarean scar ectopic pregnancy: case series and review of the literature. Am J Perinatol. 2010; 27: 111-120.
- Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R, Elson CJ. First- trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 2003; 21: 220-227.
- Seow KM, Huang LW, Lin YH, Lin MY, Tsai YL, Hwang JL. Cesarean scar pregnancy: issues in management. Ultrasound Obstet Gynecol. 2004; 23: 247-253.
- Maheux-Lacroix S, Li F, Bujold E, Nesbitt-Hawes E, Deans R, AbbottJ. Cesarean Scar Pregnancies: A Systematic Review of Treatment Options. J Minim Invasive Gynecol. 2017; 24: 915-925.
- Bignardi T, Condous G. Transrectal ultrasound-guided surgical evacuation of Cesarean scar ectopic pregnancy. 2010.
- Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol. 2012; 207: 44.e1-13.
- Timor-Tritsch IE, Monteagudo A, Calì G, D’Antonio F, Kaelin AgtenA. Cesarean Scar Pregnancy: Diagnosis and Pathogenesis. Obstet Gynecol Clin North Am. 2019; 46: 797-811.
- George Valasoulis, Ioulia Magaliou, Dimitrios Koufidis, Antonios Garas, Alexandros Daponte. Caesarean Scar Pregnancy: A Case Report and a Literature Review. 2022; 58: 740.
- Fylstra DL. Ectopic pregnancy within a cesarean scar: a review. Obstet Gynecol Surv. 2002; 57: 537-543.
- Gizzo S, Patrelli TS, Di Gangi S, et al. Cesarean scar pregnancy: A systematic review of treatment options. J Minim Invasive Gynecol. 2020; 27: 327-339.
- Timor-Tritsch IE, Monteagudo A. Diagnosis and management of cesarean scar pregnancies in the early first trimester. Am J Obstet Gynecol. 2021; 224: 545-557.
- Knez J, Herzog M, Taka? I. Multidisciplinary management of cesarean scar pregnancy: a review. Eur J Obstet Gynecol Reprod Biol. 2021; 256: 145-152.
- Li Y, Wang J, Yang Y. Double-balloon tamponade treatment for cesarean scar pregnancy: a novel conservative approach. Int J Gynaecol Obstet. 2022; 158: 92-97.
- World Health Organization. Medical management of ectopic pregnancy: WHO clinical guideline. Geneva: WHO; 2022.