Accessory Brachial Artery: A Rare Clinical Finding While Creating a Proximal Arterio-Venous Fistula
- 1. Department of Burns & Plastic Surgery, AIIMS Bhubaneswar, Odisha, India
Abstract
Arterio-venous fistula (AVF) creation is a common operative procedure performed to aid hemodialysis in patients with chronic kidney disease (CKD). While attempting to do so, often we encounter multiple issues like - small vein caliber, thrombosed vein, vascular anomaly, abnormal bleeding etc. Knowledge of anatomy of blood vessels, of the specific sites intended for surgical intervention is imperative as the surgeon may come across abnormal variations, which may cause hindrance in performing the procedure or facilitate it. Here, we describe such an unusual anatomical variation in the arm, where we observed the presence of an accessory brachial artery, while creating a proximal AVF.
Keywords
Accessory Brachial Artery, Proximal Arterio-Venous Fistula, Brachio-Cephalic Fistula, Brachio-Basilic Fistula
Citation
Mallik M, Rout SK (2022) Accessory Brachial Artery: A Rare Clinical Finding While Creating a Proximal Arterio-Venous Fistula. Ann Vasc Med Res 9(3): 1152.
INTRODUCTION
AVF is a surgical procedure commonly practiced to create a peripheral vascular channel with reasonable caliber, pressure and wall thickness to be used for hemodialysis. Radio-cephalic anastomosis in non-dominant distal forearm is the initial procedure of choice, failing which the brachial artery in the distal arm is used to anastomose either with the cephalic or the basilic vein. The knowledge of vascular anatomy in distal arm and forearm is important for the operating surgeon, though he may come across rare anatomical variations. Vascular anomalies in the form of accessory brachial artery, high bifurcation of brachial artery, compressive neuropathies of the median nerve by accessory superficial brachial artery has been described in published literature [1-7].
CASE PRESENTATION
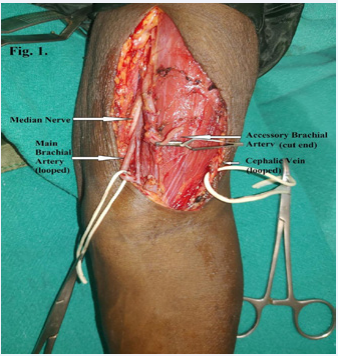
Figure 1: Accessory brachial artery (clamped proximal end), cephalic vein (looped laterally), median nerve and the main brachial artery (looped medially) with vena comitans.
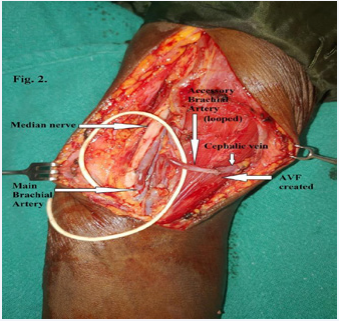
A 55-year-old lady with chronic kidney disease was referred to our department for surgical creation of a permanent AVF for hemodialysis. She was planned for radio-cephalic fistula at distal forearm level of her left (non-dominant) hand under local infiltration anesthesia. On dissection, the lumen of the cephalic vein was found to be substantially narrow. Hence, an on-table decision was made in favor of a proximal AVF (Brachio-Basilic) on the same side. With a J-shaped incision above the cubital crease on the antero-medial aspect of the arm, dissection began to identify the basilic vein. On dissection, 2 vessels were noted, a robust pulsatile one more laterally and a thin non-pulsatile one (the basilic vein) medially. The pulsating vessel was distinct in position, extending proximally, without any interconnection with any other vessels. The medial antebrachial cutaneous nerve was found in between the 2 vessels. Exploring deeper along the axis of main brachial artery, the same was found with its vena comitantes separately, in close proximity with the median nerve. The aberrant artery (found initially) was traced till the proximal and middle third junction of the arm with a distinct separate course from the brachial artery proper. This robust pulsating vessel was clamped to note the persistent pulsations of the brachial, radial and ulnar arteries distally. The decision of using the basilic vein was abandoned as its caliber was substantially small for a successful and patent long-term fistula. The cephalic vein was dissected and found to have an adequate caliber. It was decided to anastomose the cephalic vein end-to-end with the aberrant artery (accessory brachial artery) (Figure 1, Video 1). Anastomosis was completed with interrupted 8-0 monofilament polyamide sutures without disturbing the main brachial artery (Figure 2) and the surgical wound closed in a single layer. The post-operative period was uneventful and the patient was discharged from the hospital next day. On follow-up visits, the thrill of the fistula was well palpable in the proximal territory of the cephalic vein in upper arm. Later on, the channel was used for hemodialysis by our Nephrology team.
Figure 2: AVF created with end-to-end anastomosis between the accessory brachial artery (looped) and the cephalic vein.
DISCUSSION
Variation in anatomy of neurovascular structures in the upper limb has been reported in the literature but hardly detected during AVF creation in arm [1-7]. As such, there have been mentions about superficial brachial artery [1,2,7] or accessory brachial artery [3,4,6] occasionally presenting with features of median nerve compression [1,7]. Transient neuropathies or even arterial insufficiency has also been reported as a result of these anomalies [1,5]. An anatomical study has mentioned the incidence of accessory brachial artery to be as high as 11.43% [4]. A classification system has also been developed to classify the anomalous brachial artery [2] and their embryological basis analyzed [6]. However, our literature search did not reveal such anomaly to be encountered while creating AVF in the arm.
Exact nomenclature of the observed anatomical variation is not possible in our case because, it necessitates either contrast study of the upper limb vasculature or extensive dissection of the abnormal vessel to delineate the proximal as well as the distal extent. In patients suffering from CKD most of the metabolic pathways are adversely affected hence, radio-opaque intravascular contrast injection is usually contraindicated. Similarly, most of them are not good candidates for surgical procedures for various reasons and only subjected to surgeries felt essential for them. In order to explore the entire course of the anomalous vessel, dissection is required to be carried form axilla to cubital fossa or beyond these anatomical landmarks. Also subjecting these patients to general anesthesia put them into higher risk, because of which most of these procedures are performed under local infiltration anesthesia as in our case. These are the factors which prevented us to ascertain the exact extent of the anomalous vessel in our patient hence, the name of this vessel we propose, a presumptive one.
Finding such a variation in the arterial anatomy although accidental, is advantageous for the surgeon if proceeding for creation of an AVF. Because, in usual scenario the anastomosis is performed with end of the vein (cephalic / basilic) to the side of the brachial artery. The artery being single, on which the vascularity of the limb depends solely, bears, the risk of occlusion in case gets thrombosed at the site of anastomosis. Whereas if we have an accessory artery to supply the distal part of limb, we can spare one of them fully intact, and use the other for creating AVF with end-to-end anastomosis. Vascular clamp may be applied to confirm the vascular supply to the distal part, before dividing the vessel for anastomosis. This is well known to microsurgical community that an end-to-end anastomosis is easier to perform, carries less risk of hemorrhage and thrombosis at the anastomotic site and has a superior anastomotic patency rate in comparison to end-to-side one. Hence, these types of anatomical variations may not be considered as bolts from the blue, rather blessings in disguise.
Any of the superficial veins available in that anatomical zone can be used for anastomosis for creation of AVF. The choice depends on the proximity of the vein to the artery, caliber of the vein, the surgeon’s preference and at times preference of the nephrologist who will be using the vessel for hemodialysis. Cephalic vein is used most frequently because of its suitable anatomical location unless contraindicated otherwise. Whereas recent literature favors use of basilic vein for this purpose, showing better long-term patency rate [8]. In this particular case though we planned to use basilic vein for anastomosis to start with, finally decided in favor of cephalic vein because of the better caliber match. The anomalous artery was preferred for end-toend anastomosis, due to its comparatively superficial location.
Knowledge of such anatomical variation in arm, is beneficial for the surgeons. If an artery of significant diameter found in the location, not usual for the brachial artery, effort should be made to explore for the same at its natural site. If no other artery is present, the dissected artery is confirmed to be the brachial artery and an end-to-side anastomosis is contemplated. Whereas f another artery is present as an anatomical variation, then the decision may be made taking into consideration its course, caliber and proximity to the vein proposed for anastomosis, preferably end-to-end.
CONCLUSION
Accessory brachial artery is a rare congenital anomaly/ variation and whenever present, may prove to be advantageous for the surgeon as well as the patient undergoing AV fistula creation. In most of the occasions if present, it may be encountered accidentally unless contrast studies for the upper limb vessels performed for other reasons, while the patient’s condition does not contraindicate for the same. Hence, the surgeons should have the knowledge of these anomalies and be prepared to face the situation any time during their surgical practice.
ETHICAL STATEMENT
An approval was obtained from the Institute Ethics Committee; video reference number – T/IM-NF/Burns.Plastic/22/54/ September 24, 2022
REFERENCES
7. Tsoucalas G, Eleftheriou A, Panagouli E. High Bifurcation of the Brachial Artery: An Embryological Overview. Cureus. 2020; 12: e7097.