Analysis of Factors Associated to Ultrasound-Guided Vessel Cannulation in a Pediatric Training Model
- 1. Pediatric Intensive Care Unit, Mother and Child University Hospital of the Canary Islands, Spain
- 2. Interventive Radiology Unit, Mother and Child University Hospital of the Canary Islands, Spain
- 3. Departament of Biostatistics, University of Las Palmas de Gran Canaria, Spain
- 4. Department of Clinical Sciences, Fernando Pessoa Canarias University, Spain
Abstract
Objective: To analyze the factors associated to Ultrasound Guided Vessel Cannulation (UGVC) as conducted by inexperienced operators in a pediatric training model.
Methods: Descriptive observational study carried out by 25 healthcare professionals in the Pediatric Intensive Care Unit (PICU) of a level-III Hospital. After theoretical-practical training session on vascular ultrasound and ultrasound guided vessel puncture, the operators punctured the vascular structure of the simulation model and the success rate, procedural time, number of trials, complication rate were analyzed.
Results: 300 ultrasound guided vessel punctures were carried out (12 punctures per participant), uniformly distributed along the longitudinal axis/in-plane (LA/IP) and the transverse axis/out-of-plane (TA/OP). The success rate was 79.7% and it was associated to: a) larger vessel diameter: 0.42 (0.10) cm vs. 0.37 (0.09) cm, p<0.001; b) less trials required to successful cannulation: 1.49 (0.81) vs. 3.0 (1.72), p<0.001; c) shorter procedural time 87.69 (88.81) sec. vs. 225.09 (138.90) sec. p<0.001; d) better needle visibility (NV): 86.1% vs. 45.8%, p<0.001 and d) lower frequency of vessel perforation/incorrect guidewire positioning (VP/IGP): 34.2% vs. 65.8%, p<0.001.
Conclusion: In this theoretical-practical UGVC training program for inexperienced operators using a simulation model, the success rate increased with the diameter of the vascular structure to be punctured and with needle visibility, thus resulting in less trials needed to successful cannulation and lower complication rate.
Keywords
Ultrasonography; Simulation training; Vascular access; Pediatrics
Citation
López-Álvarez JM, Pérez-Quevedo O, Naya-Esteban J, López-Manteola AG, Ramirez-Lorenzo T, et al. (2022) Analysis of Factors Associated to Ultrasound-Guided Vessel Cannulation in a Pediatric Training Model. Ann Vasc Med Res 9(1): 1139.
INTRODUCTION
Given the increasing use of ultrasound imaging in daily clinical practice, this technique has been implanted in our Anesthesia, Surgery, Intensive Medicine and Emergency services [1-4]. Furthermore, there is a growing tendency to use an ultrasound-guided approach to vascular cannulation, with an increasing amount of related studies and references published in the last decade, on cannulation of peripheral or central vessels, or cannulation of central vessels with peripheral access [2,5].
As compared to traditional cannulation, ultrasound guided vessel cannulation (USVC) reduces failure and complication rates, as well as the number of trials and time required for successful cannulation, especially in case of inexperienced operators, who start using this technique for cannulation of central vessels [6-8].
Training programs in ultrasound-guided vessel cannulation (UGVC) are focused on the acquisition of basic knowledge of vascular ultrasound and its practical application, and generally use simulation models [9-12]. The acquired skills and abilities are expected to accelerate the learning curve associated to the implantation of this technique (something unavoidable at implantation of any novel technique) [11,12].
Whenever a new technique is implanted, operators need to acquire certain skills in order to be qualified to perform it. In pediatric UGVC, such skills include: a) knowledge and understanding of the ultrasound equipment; b) obtaining and optimizing needle and vessel visibility and c) skillful use of ultrasound probe and skillful needle insertion [3,6-8,13-15].
The use of simulation models in training programs for diagnostic or therapeutic procedures plays an important role in the acquisition of relevant skills by: a) improving the quality of patient management, particularly in techniques that are not devoid of risks or complications; b) preventing the stress of performing a novel technique directly on patients and c) allowing procedure repetitions for as many times as the model can be reproduced and helping solve potential in vivo problems in advance [12,16-20].
Training with simulation models enables analysis of variables associated to successful UGVC, thus promoting subsequent applications in patients.
OBJECTIVES
To analyze factors associated to successful UGVC in a pediatric training model, offered to healthcare professionals without previous experience in this technique.
METHOD
During the course of a 4-hour training program (2-hour theoretical plus 2-hour practical training), 25 operators without previous experience in UGVC conducted a total of 300 punctures (12 punctures each) uniformly distributed along the transverse axis/out-of-plane (TA/OP) and the longitudinal axis/in-plane (LA/IP), using the simulation model (figure 1) developed by Pérez-Quevedo et al. [18]. The depth and diameter (figures 2 and 3) of the vascular structures to be cannulated were established on the basis of previous determinations made in pediatric patients [21-23].
Figure 1: UGVC on the transverse axis/out-of-plane (left) and the longitudinal axis/in-plane (right) in the training model.
A Sonosite nanomaxx? ultrasound equipment was used, with a lineal L25n probe and 13-6 MHz frequency. Ultrasound-guided vessel punctures in the model allowed evaluation of: cannulation success rate, procedural time, number of trials required to successful cannulation, maneuvers needed to facilitate UGVC (repositioning of the needle/guidewire (RNG)) and potential complications of the application of this technique.
Qualitative variables were expressed as frequency and percentage. Numerical variables were expressed as mean, standard deviation and median. The normality of continual numerical variables was evaluated with the Kolmogorov-Smirnov test. Possible associations between categorical variables were evaluated with the Chi-square independence test. The means of continuous variables were compared with the Student’s t test.
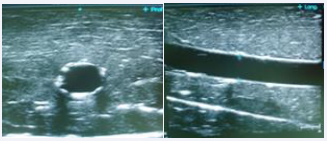
Figure 2: Ultrasound image of the vascular structure of the training model showing the transverse axis/out-of-plane (left) and the longitudinal axis/in-plane (right).
The significance level was p< 0.05.
The statistical analysis was conducted with the Statistical Package for the Social Sciences version 19 for Windows (SPSS Inc., Chicago, IL, USA).
Ethical considerations
This study was designed according to the basic principles of the Declaration of Helsinki of the World Medical Association [24]. The highest levels of professionalism and confidentiality were applied and the national regulations for data protection were observed. Participants’ right to confidentiality was granted and their identities were coded. Only authorized staff had access to identification-related personal information for data verification purposes.
This research project was approved by the Ethics Committee for Clinical Research of the Mother and Child University Hospital of the Canary Islands (Id: CEIm-CHUIMI-2016/883). Participants were voluntarily and anonymously included in the study and they agreed to the publication of the obtained results. All participants were asked to sign an informed consent form.
RESULTS
Twenty five participants (56% physicians; 44% nurses) without previous experience in UGCV carried out a total of 300 vascular punctures (12 punctures per participant) uniformly distributed along the TA/OP and the LA/IP (Figures 1,2) using a training model, after theoretical-practical training session on vascular ultrasound.
Table 1: Main qualitative variables in the UGVC model for inexperienced operators (VP/IGP: vessel perforation/incorrect guidewire positioning; vessel puncture without cannulation; PWC: puncture without canulation).
|
Variables |
% |
|
|
Needle visualization (NV) |
Complete Partial No |
41.7 42.0 16.3 |
|
Repositioning of the needle/guidewire (RNG) |
49 |
|
|
Complications |
VP/IGP PWC |
26.3 4.3 |
|
Success rate |
79.7 |
|
The mean depth and diameter of the vascular structures to be punctured were 0.90 (0.34) cm and 0.41 (0.10) cm, respectively. The mean number of attempts was 1.80 (1.24) and the mean time to cannulation was 115.63 (114.98) seconds. Table 1 describe the main outcomes of the UGVC training: a) in 41.7% of cases, needle visibility (NV) was achieved; b) in 49% of cases, RNG was needed for successful UGVC; c) the major complication encountered was vessel perforation/incorrect guidewire positioning (PV/IGP), which occurred in 26.3% of cases followed by puncture without cannulation (PWC): 4,3% and; d) the success rate was 79.7%.
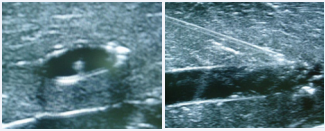
Figure 3: Visualization of the puncture needle in the transverse axis/ out-of-plane (left) and the longitudinal axis/in-plane (right) of the training model.
Complete needle visualization (CNV) (Figure 3) was associated to: a) less trials required to successful cannulation: 1.5 (0.9) vs. 2.1 (1.4), p<0.001; b) shorter procedural time: 75.2 (73.2) sec. vs. 146.9 (130.8) sec., p<0.001; c) puncture on the LA/ IP: 65% vs. TA-OP: 35% (p<0.001).
RNG was more frequently necessary when: a) puncture was made on the TA-OP (as compared to LA-IP; 62.2% vs. 35.8%, p<0.001); b) CNV was not achieved (58.7% vs. 39.0, p<0.01); c) lower diameter vessels were punctured: 0.40 (0.11) cm vs. 0.43 (0.10) cm, p<0.05.
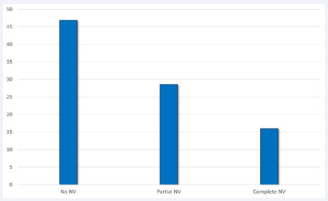
Figure 4: Relationship in percentage, between vessel perforation/ incorrect guidewire positioning (y axis) and the degree of needle visualization (NV) on the x axis.
PV/MPG occurred in association with: a) lower diameter of punctured vessel: 0.38 (0.08) cm vs. 0.42 (0.11) cm, p<0.001; b) larger amount of trials needed for correct UGVC: 2.76 (1.40) vs. 1.46 (0.95), p<0.001; c) longer procedural time: 219.72 (140.34) sec. vs. 78.42 (75.51) sec., p<0.001; d) lower success rate: 34.2% vs. 95.9%, p<0.001; e) lower proportion of CNV: 16% vs. 75.5%, p<0.001 (Figure 4, Table 2).
Table 2: Variables associated to vessel perforation/incorrect guidewire positioning (VP/IGP; s: seconds; SD: Standard Deviation; p: p-value)
|
VP/IGP Yes No |
|||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | P | |
| Depth (cm) | 0.87 | 0.32 | 0.91 | 0.28 | ns |
| Diameter (cm) | 0.38 | 0.08 | 0.42 | 0.11 | <0.001 |
| Nº trials | 2.76 | 1.40 | 1.46 | 0.95 | <0.001 |
| Tº procedure (s) | 219.72 | 140.34 | 78.42 | 75.51 | <0.001 |
The success rate was 79.7% and was associated to: a) larger diameter of punctured vessel: 0.42 (0.10) vs. 0.37 (0.09) cm, p<0.001; b) less trials needed to successful cannulation: 1.49 (0.81) vs. 3.0 (1.72), p<0.001; c) shorter procedural time 87.69 (88.81) sec. vs. 225.09 (138.90) sec, p<0.001; d) higher proportion of needle visualization (NV): 86.1% vs. 45.8%, p<0.001 and d) lower rate of vessel perforation/incorrect guidewire positioning (VP/IGP): 34.2% vs. 65.8%, p<0.001 (Table 3).
Table 3: Variables associated to success in Ultrasound Guided Vessel Cannulation (CVN: needle visualization VP: vessel perforation; IGP: incorrect guidewire positioning; Tº: time; Nº: number; s: seconds; SD: Standard Deviation)
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
DISCUSSION
This article is a continuation of a previously presented project that delves into the factors associated with success in ultrasoundguided vascular cannulation in professionals without experience in this technique [25,26].
USVC-inexperienced operators attained a global success rate of 79.7% using a training model (0.41 cm vessel diameter) similar to that of Thomas et al. [27], who reported 80.8% success with a commercially available model.
Vessel diameter has been associated to USVC success rate. Erickson et al. [28], reported 100% success with 0.56 cm vessel diameter. Lower success rates have been reported for pediatric patients as compared to adult ones, especially for those who weighed less than 10 kg or were younger than 1 year [29].
Panebianco et al. [30], reported 90% mean UGVC success rate in adult patients, with values falling below 56% for vessel diameters smaller than 0.3 cm and reaching 92% for diameters larger than 0.6 cm. The authors calculated a 1.79 increase in the probability of success per millimeter increase in vessel diameter.
In our study, no UGVC success rate differences were found in relation to vessel depth. Conversely, authors like Nakayama et al. [31], reported higher success rates for more superficial vessels (located between 0.2 and 0.4 cm depth). In this sense, Panebianco et al. [30], concluded that the success rate fell down at depths larger than 1.6 cm depth.
A mean of 1.8 trials were required for successful cannulation in this study, similarly to that reported by Thomas et al. [27] also in a training model. Furthermore, studies describe a decrease in the number of required trials associated to the use of an ultrasound-guided approach to vessel cannulation [27,32].
The number of trials was significantly higher when vessel cannulation was not achieved (1.14 vs. 3.06, p<0.001). In general, the required number of trials is inversely related to the success rate [25,30], similarly to what happens in “in vivo” patients, where trial repetition may result in hematoma, vessel perforation or arterial vessel spasm. In this study, we found a 67% rate of success-on-first-trial and 26% rate of complications due to vessel perforation or incorrect guidewire positioning.
The time needed to cannulation was 87.7 seconds in our model. Erickson et al. [28], and Phelan et al. [33], reported shorter times in their series, either because they used larger vessel diameters (0.8 cm) or because the time required to introduce the guidewire or catheter into the vessels was not included in their measurements. In such cases, the success rate may be overestimated. In our model, vessels were adequately punctured but subsequent cannulation was not possible in up to 4% of times.
In a study by Vogel et al. [34], operators with few experience in USVC, who were trained with a human torso mannequin, needed significantly less repositioning when they punctured vessels on the LA/IP. In our series, similar results were obtained; the proportion of RNG was higher on the TA/OP than on the LA/ IP (62% vs. 38%) because needle visualization was easier on the latter one. Some studies however, have described different results. On the one hand, Chittoodan et al. [35] and Schummer et al. [36] reported higher success-on-first-trial rates and less needle repositioning on the TA/IP than on the LA/OP. According to these authors, these outcomes were due to the fact that operators had previous UGVC experience and had been using the TA/IP more frequently, because puncture on the LA/OP required better eyehand coordination and harder-to-achieve alignment of vessel axis and transducer. On the other hand, in two other studies [30,37], no differences were found between the longitudinal and the transverse approach in terms of RNG and the authors concluded that it was not possible to do recommendations in this regard.
The choice of an axis for ultrasound and vessel approach is a controversial issue. In this study, no difference was found in UGVC success rate between LA/IP and TA/OP. However, Tassone et al. [38], in a comparison of both axes, reported higher success rate for the LA-IP (83.3%) than for the TA/OP (70.8%).
Needle visibility (NV) is a further important issue in UGVC. Few studies on this topic have been conducted. Basically, it has been addressed in terms of the ultrasound axis where NV is better. The rate of NV is controversial and highly subjective; artifacts may introduce confusion and different observers may report different NV results for the same patient or model [14,39].
In our study, NV was null in 16% of cases. Some studies describe that real-time visual control of the needle tip increases technique’s safety and may consequently reduce complications. Therefore, obtaining NV is a basic goal in UGVC, when it comes to improve patient safety, as Hovgesen et al. [40] and Moak et al. [41] claim.
In a series published by Stone et al. [42], the LA/IP approach to UGVC was associated to better needle tip visibility during vessel puncture. The authors reported that NV reached 62% on the LA/IP, while it was 23% on the TA-OP. In our series, NV was also higher on the LA/IP (59%) than on the TA/OP (39%), a foreseeable outcome since the first axis provides better visualization of the needle path. However, the LA/IP approach requires better ultrasound imaging skills through accurate alignment of the needle, vessel and transducer axes.
Therefore, a good knowledge is important to promote the safety of this technique, especially regarding needle manipulations, so as to prevent derived complications [41,42].
Thus, accurate identification of the needle tip is a main objective to achieve, so as to be able to continue monitoring the needle path towards the vascular structure. However, involved technical difficulties and safety implications make this issue one of the most frustrating aspects of applying UGVC “in vivo” after a training period with simulation models, where achieving good needle visibility is easier.
REFERENCES
16. Nolting L, Hunt P, Cook T, Douglas B. An Inexpensive and Easy Ultrasound Phantom: A Novel Use for SPAM. J Ultrasound Med. 2016; 35: 819-22.








































































































































