Central Venous Catheter Tips Showing Pigtail Features on Chest X-Ray to Both Sides of the Sternum-Highlighting the Causes
- 1. Department of Anesthesiology and Intensive Care Medicine, Friedrich-Schiller-University Jena, Germany
Abstract
Despite the level of skill of the operator and the use of ultrasound guidance, central venous catheter (CVC) placement can result in CVC malpositioning, i.e., an unintended placement of the catheter tip in an inadequate vessel. CVC malpositioning is not a complication of central line insertion; however, undiagnosed CVC malpositioning can be associated with significant morbidity and mortality.
Citation
Schummer W (2017) Central Venous Catheter Tips Showing Pigtail Features on Chest X-Ray to Both Sides of the Sternum-Highlighting the Causes. Ann Vasc Med Res 4(5): 1066.
INTRODUCTION
Central venous catheters (CVCs) are designed to access the central venous circulation and are normally inserted via the Seldinger guide wire technique. CVCs are an essential component of modern-day critical care and emergency medicine.1 In this context, CVCs are used to administer life-supporting fluids, potentially irritant drugs, blood products, and parenteral nutrition. In other settings, CVCs are used to provide access for hemodialysis, transvenous heart pacing, and monitoring of hemodynamics by measuring central filling pressure and cardiac output [1,2]. But the insertion of central venous catheters is not free of complications, even when performed by skilled professionals [3].
The most common adverse events associated with CVC insertion, extensively addressed in the literature, include mid- and long-term infection (5% to 26%), thrombosis (2% to 26%), and mechanical complications during the central venous access procedure (5% to 19%), with a nearly 7% malpositioning rate among skilled operators [1,3]. However, mechanical complications related to the access procedure are expected to be significantly reduced by the practices of ultrasound guidance and ultrasound assistance [4,5].
A less commonly described yet important complication of CVC placement is malpositioning of the CVC tip in a vessel other than the superior vena cava (SVC), usually in one of the various large tributaries of the SVC. This event has been described in the literature as occurring in approximately 7% of cases of thoracic CVC placement and can lead to serious complications if not addressed appropriately [2,3]. Placing the CVC tip in a vessel other than the SVC increases the risk of catheter wedging, erosion or perforation of vessel walls, local venous thrombosis, catheter dysfunction, and even cranial retrograde injection, in which the infusate is directed to the head instead of to the central circulation [2].
In this article, we focus on the rare pigtail features on chest X-ray after central venous catheterization, on their causes, and on measures to eliminate the risk of malpositioning or, if malpositioning already has happened, to recognize and manage the incident appropriately.
Case 1
In a 73-yr-old patient suffering with right-sided malignant infarction of the medial cerebral artery region of the brain, a CVC was placed in the left subclavian vein according to the Seldinger technique. Aside from meeting a slight resistance during advancement of the guide wire, no problems of catheter placement were reported. Venous blood could be aspirated easily and the transuded venous pressure measurements showed a typical venous waveform pattern. However, despite sinus rhythm while using electrocardiography (ECG) to guide the CVC positioning, a typical pattern of ECG changes could not be detected.
Assuming malposition of the original CVC, a second catheter was placed through the left brachiocephalic vein. Here, the ECG guidance worked as expected and the catheter was advanced until a maximum P-wave (Pmax) pattern could be detected.
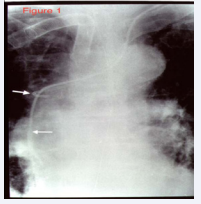
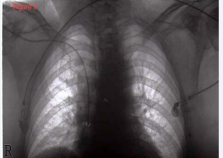
A frontal chest radiograph demonstrated the first catheter curling up in the azygos arch (Figure 1).
Figure 1: Frontal chest radiograph depicting the first CVC curling in azygosvein, the second CVC placed correctly in the SVC. Abbreviations: CVC: Central Venous Catheter; SVC: Superior Vena Cava
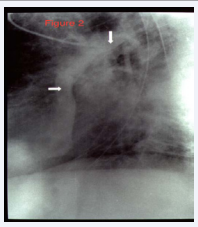
The second CVC was shown to be positioned correctly in and running along the long axis of the SVC. A second (lateral view) radiograph was taken, applying water-soluble contrast medium through the misplaced catheter (Figure 2).
Figure 2: Lateral view chest radiograph applying water-soluble contrast medium through the misplaced CVC. Parts of the azygos arch and the SVC were emphasized by runoff of contrast media. Abbreviations: CVC: Central Venous Catheter; SVC: Superior Vena Cava
Here, parts of the azygos arch as well as the SVC were emphasized by the runoff of contrast medium.
Case 2
In an intensive care patient, a CVC was inserted through the left internal jugular vein. The cannulation was described as having proceeded without problems. However, upon being interviewed, the operator revealed that he had met a slight elastic resistance at 10–12 cm while advancing the guide wire. The CVC insertion then proceeded without further problems, but, coincident with the ECG guidance, the P-wave amplitude did not change during advancement of the catheter. Clinically, venous blood could be aspirated easily and the transduced venous pressure measurements showed a typical venous waveform pattern.
Assuming malposition of the original CVC, a second catheter was placed through the left internal jugular vein. Here, the ECG guidance worked as expected and the catheter was advanced until a Pmax pattern could be detected.
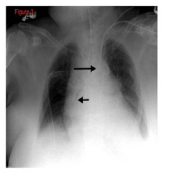
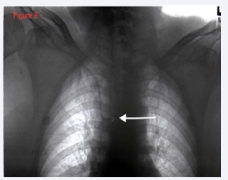
On frontal chest X-ray, the first catheter was found to have curled in projection of the aortic knob (Figure 3).
Figure 3: Frontal chest radiograph with first CVC curled in projection of the aortic knob. The second CVC was sited appropriately outside the right atrium and along the long axis of SVC. Abbreviations: CVC: Central Venous Catheter; SVC: Superior Vena Cava
Aortic misplacement could be ruled out by already proven venous pressures. The second CVC, placed at Pmax using ECG guidance, was placed appropriately, outside the right atrium and along the long axis of the SVC. The malpositioned CVC was removed uneventfully.
Case 3
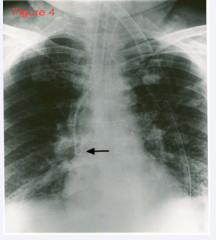
In another ICU patient on vasopressor support, a CVC had to be inserted. Here, no resistance was met during advancement of the guide wire and the catheter. ECG guidance worked properly while using an Alpha card® syringe (which uses the sodium chloride–filled distal lumen of the CVC as an electrical conductor). However, as could easily be seen on chest radiography, the CVC tip was curled in the SVC (Figure 4).
Figure 4: Frontal chest radiograph of a curled catheter tip of an appropriately sited CVC in the SVC. Abbreviations: CVC: Central Venous Catheter; SVC: Superior Vena Cava
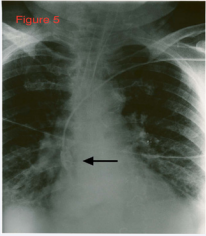
A second X-ray was taken while injecting a water-soluble contrast medium through the distal lumen (Figure 5).
Figure 5: Contrast media runoff in SVC. Abbreviations: SVC: Superior Vena Cava
The answer to this riddle was the type of catheter used-a COOK® curved tip, triple-lumen CVC designed to reduce the risk of SVC perforation, especially in left-sided approaches.
DISCUSSION
Central venous catheterization is an essential component of current clinical practice. But the insertion of CVCs is not without risk. Numerous complications described both during placement of the catheter and later during long-term maintenance, are hazardous to patients and expensive to treat. Malposition of the catheter tip is one of such complication, which usually involves placement of the catheter in various large tributaries of the SVC.
Anatomy
Variations in venous anatomy as well as challenging body habitus (e.g., obesity or large breasts) are believed to contribute to primary CVC malpositioning and tip migration and thus to secondary malpositioning as well.
Two types of variants in venous anatomy are recognized: congenital and acquired.In patients with congenital variations, they are usually discovered incidentally on imaging after CVC placement [2]. Although these variations are usually asymptomatic, they can make the radiologic location of the CVC tip difficult to discern. A common congenital variation with clinical significance is a persistent left-sided SVC, which is seen in 0.3% of healthy patients and 4% of patients with congenital heart disease [6,7].
Other relevant congenital variations in venous anatomy include a dominant supreme (highest) intercostals venous drainage to the hemiazygos vein, inferior vena cava (IVC) variations, partial anomalous pulmonary venous drainage, and azygos vein abnormalities in origin, course, tributaries, anastomoses, and termination [2,8].
Acquired variations in venous anatomy are more common than congenital variations and can be external or internal in origin. More than 85% of external vessel distortions are caused by compression secondary to malignancy (often lung cancer, breast cancer, lymphoma, or germ cell tumors) [2]. Benign causes of external distortion include substernal goiter, thymoma, cystic hygroma, and histoplasmosis. Also, lung collapse or pleural effusions can shift venous structures such as the SVC away from the midline. Internal vessel distortion can be caused by thrombosis or stenosis. The risk of thrombosis can be increased by recent surgery, inflammation, malignancy, immobilization, hemodialysis, chemotherapy, and pregnancy, and vessel stenosis has been associated with overuse of any vessel, subclavian cannulation, and central venous access from the left side of the neck [2,8].
In normal anatomy, the azygos vein (v. azygos; vena azygos major) begins opposite the first or second lumbar vertebra, by a branch, the ascending lumbar vein, or sometimes by a branch from the right renal vein, or from the IVC. It enters the thorax through the aortic hiatus in the diaphragm, and passes along the right side of the vertebral column to the fourth thoracic vertebra, where it arches forward over the root of the right lung, and ends in the superior vena cava, just before that vessel passes through the pericardium [9].
The left vein (v. intercostalis suprema sinistra) runs across the arch of the aorta and the origins of the left subclavian and left common carotid arteries and opens into the left in nominate vein. It usually receives the left bronchial vein (and sometimes the left superior phrenic vein) and communicates below with the accessory hemiazygos vein [9].
The azygos and hemiazygos system are thoracic continuations of the ascending lumbar veins within the posterior aspect of the thorax. Usually, the azygos arch drains into the posterior aspect of the SVC approximately 1 cm below the junction of the right and left brachiocephalic (in nominate) veins. The hemiazygos system drains into the left brachiocephalic vein via the left superior intercostal vein [9,10].
Anatomically, when compared with the right brachiocephalic vein, the left brachiocephalic vein is more horizontal and its junction with the SVC usually occurs almost a right angle [9]. Accordingly, guide wires inserted from the left side may be advanced inadvertently into an inferior tributary of the brachiocephalic vein, leading to CVC malpositioning [11,12].
Also, guide wires from the left while being advanced will always contact the lateral wall of the SVC before (hopefully) turning round into the SVC. This seems to be the mechanism for misplacement of catheters into the azygos arch. Hence, the risk of azygos arch cannulation is substantially increased if catheters are inserted through left-sided veins [13].
In our Case 1, the azygos arch drained close to the junction of the brachiocephalic veins. We blame this anatomical variation for causing the repeated difficulties in advancing the guide wire into the SVC, since the guide wire and the catheter kept getting caught in the azygos arch.
Malposition in the azygos arch occurs in 1.2% of central venous cannulations [13].
In one series, 19% of catheters misplaced into the azygos arch resulted in perforation [13].
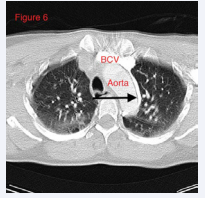
In our Case 2, the pigtail feature of the CVC tip in projection on the aortic knob is pathogenetic of CVC misplacement in the left superior intercostal vein. This is due to the course of the left superior intercostal vein in the neighborhood of the aortic arch (Figure 6) [9,14].
Figure 6: Computed tomography of the course of left superior intercostal vein (arrow) in another patient. Abbreviations: BCV: Brachiocephalic Vein
However, one should bear in mind that malposition of the catheter tip may occur not only at the time of insertion, but also later, as a result of spontaneous migration due to anatomic positioning or pressure changes within the thoracic cavity, an effect augmented by repeated forceful coughing. Also, intravenous therapy is often administered faster than recommended, as workload for nursing staff is steadily increasing.
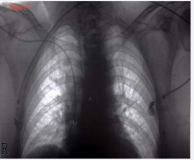
A high flow rate at the catheter tip may produce a jet effect, causing displacement of the tip backwards and upwards (Figures 7-9) [15].
Figure 7: CVC in appropriate position in SVC. Abbreviations: CVC: Central Venous Catheter; SVC: Superior Vena Cava
Figure 8: CVC malposition in azygos vein.
Figure 9: CVC in appropriate position in SVC. No intervention had been performed in the meantime.
Malposition, whether aberrant into another vein or simply due to poor positioning, can have serious consequences [16]. Perforation, thrombosis, vascular stenosis, and even complete vascular occlusion in children have been reported with CVC malpositioning in the azygos arch [11].
It is difficult to ensure correct placement of a CVC in the SVC in the absence of either ECG guidance or ultrasound or pressure monitoring. Any difficulty in advancing a guide wire or catheter is the vital clue that should alert the operator that misplacement may be occurring. Also, catheter dysfunction and/or (in the conscious patient) persistent, intermittent, or exacerbating chest or back pain after central infusion always require immediate chest radiography (frontal and lateral), eventually with contrast material. A misplaced CVC in the azygos arch or left superior intercostal vein must be removed immediately.
Mechanisms of malpositioning
While the mechanisms of CVC malpositioning are not well understood, it appears to be multifactorial. Some studies have shown that, upon needle insertion, the orientation of the bevel facilitates the progression of the guide wire in a certain direction [17]. For example, when one attempts an internal jugular vein catheterization, orienting the needle bevel medially facilitates guide wire passage into the SVC [18]. On the same rationale, there have been small randomized controlled studies demonstrating an effect of bevel orientation in subclavian catheterizations, with a higher rate of correct placements when the bevel was oriented caudally [18].
During guide wire insertion, it will be prudent to feel for any obstruction or change in resistance that may denote change in direction or coiling. However, it takes awareness and experience to develop this feel [19].
A maneuver to prevent misplacement of a subclavian CVC into the ipsilateral internal jugular vein due to guide wire deflection has been described, namely, manual occlusion of the ipsilateral internal jugular vein in the supraclavicular area during guide wire insertion [20].
The tips of catheters that are inserted on the left side, however, are also more likely to impinge on the right caval wall; this holds particularly true when the inserted length of the CVC is insufficient. Moreover, unfavorable angulations of the catheter against the SVC wall, irritations produced by high flow, infused hyperosmolar infusion, and mechanical forces from catheter migration promote vascular perforation. Even when the proper position of the CVC tip has been confirmed radio graphically, erosion may occur. It is well documented that flexion and extension of the neck can cause a catheter to migrate several centimeters, and this migration can unfavorably reposition the catheter tip [11,16].
Measures for prevention
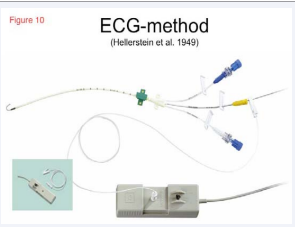
ECG guidance during CVC placement is an excellent technique that excludes unrecognized malpositioning. This technique was first described by Heller stein and colleagues in 1949. With an intra luminal wire or with saline as an electro conductive medium, the tip of the catheter is used as an electrode to obtain the intravascular/intra-atrial ECG (Figure 10) [21].
Figure 10: ECG-guidance during CVC insertion. Attach connection cable (white) with a crocodile clip to the guide wire. The other end of the connection cable joins a switch box that has to be joined up in the circuit. This allows switching the right-arm ECG electrode to the catheter tip to get an intravascular ECG display. Arrow indicates tip of the guide wire, which serves as an intravascular electrode.
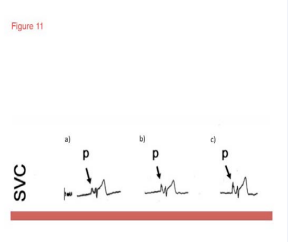
As the catheter tip is at the junction of the SVC and the right atrium (RA), the P-wave amplitude increases to Pmax (Figure 11) [22,23].
Figure 11: ECG guidance during insertion: a) Normal P-wave amplitude in SVC above pericardial reflection. b) At pericardial reflection first significant increase in P-wave amplitude. c) Maximal P-wave amplitude at SVC/RA junction. Abbreviations: SVC: Superior Vena Cava; RA: Right Atrium.
Further advancement of the catheter tip either shows a decrease in P-wave amplitude or turns the P-wave biphasically [22,23]. Almost 40 years ago, neurosurgeons used this technique for the first time to place ventriculo-atrial shunts. At that time, other applications of the ECG-guidance technique were used for positioning pacer probes and for intra cardial diagnosis of complex cardiac dysrhythmias.
Many clinical studies have shown that ECG guidance during CVC placement is a well-proven tool for reducing malpositioning [21-26]. For other methods, such as chest radiography or formulas, evidence in this respect is lacking. Chest radiography is useful for recognizing malpositions after CVC placement and for detection of mechanical complications. Formulas can give only an assumption of insertion depth, which is of little help in clinical practice, due to the individuality of each patient.
ECG-guided CVCs can be positioned exactly, obviating the need for position control via chest radiography. However, for exclusion of mechanical complications (e.g., pneumothorax), a chest X-ray is mandatory. ECG guidance, however, can be difficult in patients with arrhythmias.
Placing a CVC without fluoroscopic or ECG guidance results in malpositioning in at least 15% of patients, and an incidence of complications of about 12%.
When available, transesophageal echocardiography (TEE) to assist during placement of the CVC is a highly accurate method of ensuring a location in the SVC or at the SVC/RA junction [22-24].
With reservations, this also holds true for transthoracic echocardiography (TTE).
Ultrasound examination is performed through epigastric and subcostal acoustic windows along the short heart axis. This enables the simultaneous visualization of the SVC, IVC, and RA. A 10-mL syringe, containing 9 mL of saline and 1 mL of air, is agitated until a homogeneous mixture of saline and air is achieved. Subsequently, this syringe is attached to the lumen of the catheter, ending at its tip. Next, 5 mL of the solution is injected rapidly through the catheter. Interpretation of the micro bubble test should be performed using the criteria described by Vezzani and colleagues (Table 1) [27].
|
Table 1: Criteria for Classification and Interpretation of Microbubble Test. |
|
|
Characteristic |
Interpretation |
|
No bubbles
|
Negative test: an aberrant tip position must be considered |
|
Few bubbles or appearance time > 2 sec |
Test to be repeated: if confirmed, possible misplacement |
|
Numerous bubbles and turbulent flow coming from RA within 2 sec |
Negative test: intra-atrial positioning |
|
Numerous bubbles and laminar flow coming from SVC |
Positive test: CVC tip correctly placed in SVC |
|
Abbreviations: CVC: Central Venous Catheter; RA: Right Atrium; SVC: Superior Vena Cava |
|
A stream of micro bubbles with laminar jet flow from the SVC within 1 to 2 seconds after the injection indicates correct catheter location.
After placement of all CVCs, a chest X-ray should be performed for exclusion of mechanical complications and CVC malpositions. A poster anterior or anteroposterior film is usually adequate; if not, a lateral view may be taken. If uncertainty still exists, a venogram through the catheter should be performed for precise localization [7,13] A properly placed subclavian or internal jugular catheter should run parallel to the shadow of the SVC.
Differential diagnosis of left-sided thoracic CVCs will help categorize the type of malposition-extra vascular in pleura, pericardium, or mediastinum; arterial; in a vein other than the superior vena cava; or a persistent left SVC (LSVC) [7,28,29].
• An extravascular malposition can be excluded clinically by free venous backflow through all catheter lumina and the absence of clinical symptoms.
• Malposition in the descending aorta should be ruled out by transduction of the venous pressure waveform.
• A water-soluble contrast medium-enhanced lateral chest X-rayis the quickest and most inexpensive reliable method fordifferentiatinga left-sided malposition from a correct position in a persistent LSVC.
• A catheter tip overlying the anterior mediastinum is located in the left internal mammary vein.
• A catheter tip overlying the middle mediastinum is placed in an LSVC or leftpericardiophrenic vein.
• A catheter inserted deep into the left pericardiophrenic vein runs a characteristic course on frontal chest x-ray along the cardiac border [7,28].
• Contrast media run-off will allow differentiation of a pericardiophrenic vein and persistent LSVC; contrast media run-off is poor in the pericardiophrenicvein. In an LSVC, the run-off is good.
• A catheter tip overlying the posterior mediastinum is placed in the left superior intercostal vein or the descending aorta [7,28,29].
• Contrast media will extravasate if the catheter tip is placed extravascularly.
• Because an LSVC runs in front of the descending aorta, on frontal chest radiography, a catheter in a LSVC can easily be confused with a malposition in the descending aorta.
• Further methods to differentiate left-sided catheters and venous anomalies are TEE, magnetic resonance imaging, and computed tomography.
For the differential diagnosis of curled CVCs to either right or left of sternum, please refer to Table (2).
|
Table 2: Differential Diagnosis of Curled CVCs to Right or Left of Sternum. |
|||
|
Anatomy |
CXR ap view |
CXR lat view |
Contrast media application |
|
Azygos arch |
Right of sternum |
Dorsal mediastinum |
Runoff in SVC |
|
Superior intercostal vein |
Left of sternum, characteristic „bend“ in projection to aortic knob |
Dorsal mediastinum |
Runoff in hemiazygos vein |
|
Abbreviations: CXR: Chest Radiograph; ap: antero-posterior; lat: lateral; SVC: Superior Vena Cava |
|||
Malpositioning of CVCs is usually asymptomatic. Placement in the superior intercostal, azygos, and hemiazygos veins may, in awake patients, result in back pain while flushing the catheter. Though characteristic chest pain often provides a clue to the erroneous catheter position, catheter malposition is more often identified by a post-procedure chest radiograph.
If the course of a misplaced catheter can be correctly identified as not lying within a vulnerable structure, then it can be safely removed. If the misplaced catheter is lying within or traversing large and incompressible arteries or veins, it should not be removed before consideration of what is likely to happen once it is removed. Advice and further imaging should be sought, typically in conjunction with interventional radiology or vascular surgery. With regard to misplaced CVCs, in the short term, a useful aide mémoire is: “If in doubt, don’t take it out” [8,30].
CONCLUSIONS
Knowledge of normal and variant anatomy must be considered essential for all those involved in the insertion and assessment of central venous catheters. Moreover, during guide wire insertion, it will be prudent to feel for any obstruction or change in resistance that may denote change in direction or coiling. Any difficulty in advancing a guide wire or catheter is the vital clue that should alert the operator that misplacement may be occurring.
In patients with sinus rhythm, the only low-key and reliable bedside method for assessing CVC tip position is ECG guidance while advancing the catheter. Alternatively, TTE can be performed, applying an agitated saline solution through the catheter to estimate CVC tip position.
Post procedural chest radiography should be performed after each CVC insertion for assessment of malpositioning and contingent mechanical complications.
Always bear in mind that, while CVCs are beneficial devices in modern medicine, they also carry particular risks. To deal with them, awareness, knowledge, and experience are key.
REFERENCES
- McGee DC, Gould MK. Preventing complications of central venouscatheterization. N Engl J Med. 2003; 348: 1123-1133.
- Roldan CJ, Paniagua L. Central venous catheter intravascular malpositioning: causes, prevention, diagnosis, and correction. West J Emerg Med. 2015; 16: 658-664.
- Schummer W, Schummer C, Rose N, Niesen WD, Sakka SG. Mechanical complications and malpositions of central venous cannulations by experiencedoperators: a prospective study of 1794 catheterizations in critically ill patients. Intensive Care Med. 2007; 33: 1055-1059.
- Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, et al. International evidence-basedrecommendations on ultrasound-guided vascular access. Intensive Care Med. 2012; 38: 1105-1117.
- Schummer W, Köditz JA, Schelenz C, Reinhart K, Sakka SG. Pre-procedure ultrasound increases the success and safety of central venous atheterization. Br J Anaesth. 2014; 113: 122-129.
- Schummer W, Schummer C. Images in cardiovascular medicine. Cannulation of a persistent left superior vena cava: a clue given by ECG guidance. Circulation. 2006; 114: e503-504.
- Schummer W, Schummer C, Steenbeck J. Central venous catheter in the left hemithorax--malpositioned?. J Cardiothorac Vasc Anesth. 2004; 18: 529-531.
- Gibson F, Bodenham A. Misplaced central venous catheters: applied anatomy and practical management. Br J Anaesth. 2013; 110: 333-346.
- Shah P. Heart and great vessels. In: Standring S.Gray`s Anatomy:TheAnatomical Basis of Clinical Practice, 39th ed. Elsevier, 2005:1025-1027.
- Heitzman ER. The Mediastinum: Radiologic Correlations with Anatomy and Pathology, 2nd ed. Berlin, Germany: Springer, 1988.
- Currarino G. Migration of jugular or subclavian venous catheters into inferior tributaries of the brachiocephalic veins or into the azygos vein, with possible complications. Pediatr Radiol. 1996; 26: 439-449.
- Muhm M, Sunder-Plassmann G, Apsner R, Pernerstorfer T, Rajek A, Lassnigg A, et al. Malposition of central venous catheters. Incidence, management and preventive practices. Wien Klin Wochenschr. 1997; 109: 400-405.
- Bankier AA, Mallek R, Wiesmayr MN, Fleischmann D, Kranz A, Kontrus M, et al. Azygos arch cannulation by central venous catheters: radiographic detection of malposition and subsequent complications. J Thorac Imaging. 1997; 12: 64-69.
- Ghatak T, Azim A, Baronia AK, Muzaffar SN. Malposition of central venous catheter in a small tributary of left brachiocephalic vein. J Emerg Trauma Shock. 2011; 4: 523-525.
- Rasuli P, Hammond DI, Peterkin IR. Spontaneous intrajugular migration of long term central venous access catheters. Radiology. 1992; 182: 822-824.
- Tocino IM, Watanabe A. Impending catheter perforation of superior vena cava: radiographic recognition. AJR Am J Roentgenol. 1986; 146: 487-490.
- Park HP, Jeon Y, Hwang JW, Han SH, Bahk JH, Oh YS. Influence of orientations of guidewire tip on the placement of subclavian venous catheters. Acta Anaesthesiol Scand. 2005; 49: 1460-1463.
- Tripathi M, Dubey PK, Ambesh SP. Direction of the J-tip of the guidewire, in Seldinger technique, is a significant factor in misplacement of subclavian vein catheter: a randomized, controlled study. Anesth Analg. 2005; 100: 21-24.
- Dubey PK. Beware of the twisted guidewire. J Clin Anesth. 2008; 20: 70-71.
- Ambesh SP, Dubey PK, Matreja P, Tripathi M, Singh S. Manual occlusion of the internal jugular vein during subclavian vein catheterization: a maneuver to prevent misplacement of catheter into internal jugular vein. Anesthesiology. 2002; 97: 528-529.
- Schummer W, Schummer C, Müller A, Steenbeck J, Fuchs J, Bredle D, et al. ECG-guided central venous catheter positioning: does it detect the pericardial reflection rather than the right atrium?. Eur J Anaesthesiol. 2004; 21: 600-605.
- Schummer W, Schummer C, Schelenz C, Schmidt P, Fröber R, Hüttemann E. [Modified ECG-guidance for optimal central venous catheter tip positioning. A transesophageal echocardiography controlled study]. Anaesthesist. 2005; 54: 983-990.
- Chu KS, Hsu JH, Wang SS, Tang CS, Cheng KI, Wang CK, et al. Accurate central venous port-A catheter placement: intravenous electrocardiography and surface landmark techniques compared by using transesophageal echocardiography. Anesth Analg. 2004; 98: 910-914.
- Kremser J, Kleemann F, Reinhart K, Schummer W. Optimized method for correct left-sided central venous catheter placement under electrocardiographic guidance. Br J Anaesth. 2011; 107: 567-572.
- Gebhard RE, Szmuk P, Pivalizza EG, Melnikov V, Vogt C, Warters RD. The accuracy of electrocardiogram-controlled central line placement. Anesth Analg. 2007; 104: 65-70.
- Ender J, Erdoes G, Krohmer E, Olthoff D, Mukherjee C. Transesophageal echocardiography for verification of the position of the electrocardiographically-placed central venous catheter. J Cardiothorac Vasc Anesth. 2009; 23: 457-461.
- Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, Corradi F. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010; 38: 533-538.
- Gentili DR, Onofrey D, Gabrielson GV, Benjamin E, Iberti TJ. Malposition of central venous catheters outside the central circulation. J Cardiothorac Anesth. 1989; 3: 752-756.
- Godwin JD, Chen JT. Thoracic venous anatomy. AJR Am JRoentgenol. 1986; 147: 674-684.
- Guilbert MC, Elkouri S, Bracco D, Corriveau MM, Beaudoin N, Dubois MJ, et al. Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithm. J Vasc Surg. 2008; 48: 918-925.