Endovascular Repair of “Seat Belt” Aortic Injury Following Motor Vehicle Accident
- 1. Southern Arizona Vascular Institute, 777 W Calle Concordia Tucson, USA
- 2. Section of Vascular Surgery, The University of Arizona, USA
INTRODUCTION
The mechanical forces inflicted during collision are thought to compress the abdominal aorta between the low horizontal seat belt and vertebral column thereby manifesting thrombosis, dissection, and, with enough magnitude, traumatic transection [6-9]. Among these lesions, abdominal aortic transection carries a significant mortality rate of 80-85% [9]. Most patients die at the scene of the accident, and those who are transferred emergently to the hospital will exhibit a relatively high mortality rate of 20% [9].
Prompt recognition and management are crucial for patient survival. The treatment options for BAAI are either non-operative management or surgical repair, the latter of which has historically involved laparotomy as first-line intervention among patients with hypotensive shock, active bleeding, or penetrating mechanism of injury [10-12]. While use of endovascular aortic repair (EVAR) techniques for traumatic abdominal vascular injuries is becoming more frequent, its role in abdominal aortic transection remains underreported [11-15]. We present a case of endovascular revision for a transected abdominal aorta in a young male following an MVA. The patient has provided the authors with permission to use his clinical details and images for this report.
CASE REPRESENTATION
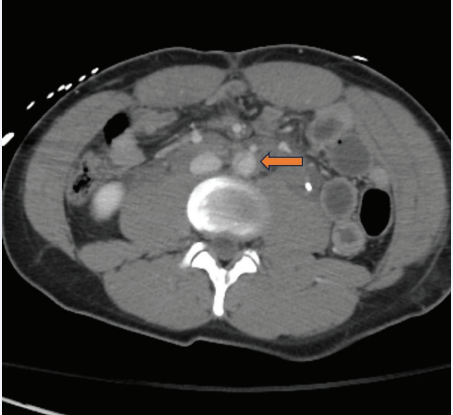
The patient is a 24-year-old male restrained driver involved in a head-on collision. He was taken to a local hospital where his primary complaints included abdominal and back pain. Computed tomography (CT) revealed a burst fracture of L3 and findings suggestive of contained transection of the abdominal aorta. Weather conditions delayed transport to a level 1 trauma center which was ultimately accomplished 4 hours later. Upon arrival, he was neurologically intact and continued to describe abdominal and back pain. He was normotensive, though slightly tachycardic. He had normal lower extremity pulse exams. He had bruising across his chest and abdomen consistent with seat belt and upper body restraints. Imaging from the referring hospital was reviewed by the trauma and vascular teams and confirmed the appearance of contained abdominal aortic transection just below the take-off of the inferior mesenteric artery (IMA) and above the bifurcation. There appeared to be a circumferential disruption of the aortic intima on CT imaging [Figure 1]. No other obvious intra-abdominal injuries were apparent.
Figure 1: Computed tomographic image of abdomen obtained upon emergency department arrival which shows circumferential transection of the intima of the abdominal aorta (arrow).
The trauma team did not feel he needed abdominal exploration based on the available imaging and his exam, so he was taken to the hybrid endovascular operating room and, under general anesthesia, underwent percutaneous endovascular repair of the aortic transection.
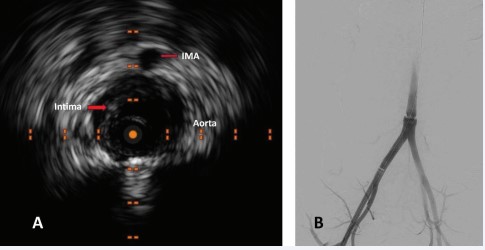
Intraoperative intravascular ultrasound [Figure 2A] and angiography [Figure 2B] evaluations confirmed a complete, circumferential intimal disruption that was highly focal. Successful exclusion of the injury was achieved by deploying a 26 mm x 33 mm Gore® Excluder® cuff (W.L. Gore and Associates, Inc., Flagstaff, Arizona) from just above the aortic bifurcation to just below the takeoff of the IMA. His immediate postoperative course was notable for continued abdominal pain. On the first postoperative day, he was taken for exploratory laparoscopy by the trauma team for ongoing abdominal pain and was found to have a bucket handle mesenteric injury requiring 2 segmental small bowel resections with primary anastomoses. One of the injured small bowel segments was perforated. He also had a serosal tear of his sigmoid colon that was treated with Lembert sutures. Additionally, he was noted to have complete transection of his rectus muscles.
Figure 2: Intraoperative intravascular ultrasound, A, which confirms complete circumferential disruption of the intima of the aorta just below the take-off of the inferior mesenteric artery (IMA), also seen on catheter-based angiography, B.
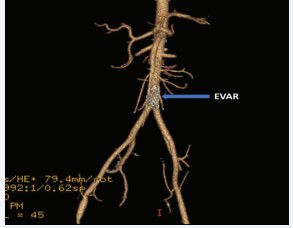
His hospital course after the laparotomy was largely uneventful. His L3 burst fracture was treated conservatively by neurosurgery with a lumbar-sacral orthosis brace. He had advancement of diet and activity then discharged home on the 8th postoperative day. Prior to discharge, a follow-up CT angiogram was performed to assess the aortic repair which demonstrated complete exclusion of the area of injury with the endovascular stent graft with widely patent IMA and iliofemoral run-off vessels [Figure 3].
Figure 3: Follow-up computed tomographic angiography, maximum intensity 3-D projection obtained prior to hospital discharge demonstrating complete exclusion of the area of injury with the endovascular stent graft (EVAR), as well as widely patent iliofemoral run-off vessels.
DISCUSSION
The management of concomitant bowel and mesenteric injuries in the context of BAAI can be challenging, particularly in the setting of trauma. Patients may present with shock, exquisite hypotension, massive blood loss, or multiple associated injuries including blunt intraabdominal injury and thoracolumbar fractures, the concurrent presentation of which was initially described in 1962 as “seat belt syndrome” [1,16]. The term “seat belt aorta” was later coined by Dajee in 1979 to describe blunt aortic injury sustained by a seat belt secondary to MVA [6]. Indeed, a cautious integration of clinical observation and diagnostic tools is essential for prompt recognition of aortic transection, with the primary focus of treatment being rapid hemorrhage control [11].
Prior publications have suggested that the location and grading of vascular injuries will determine the most optimal treatment algorithm [1-3,10,12,17]. BAAIs are classified into one of three categories: Zone I, involving the diaphragmatic hiatus to the superior mesenteric artery (SMA); Zone II, which includes the SMA and renal arteries; and Zone III, extending from the renal arteries inferiorly down to the aortic bifurcation. Among these, Zone III is believed to be the most common location of traumatic abdominal aortic injuries [1]. In the present case report, the area of aortic transection was deemed to be Zone III. A Western Trauma Association multicenter study from 2014 found that among 113 patients with BAAIs, 89.5% of intimal tears and flaps were managed non-operatively with blood pressure optimization, while 100% of aortic ruptures were managed with laparotomy [2]. Within the same year, the Society for Vascular Society published guidelines for the management thoracic aortic injuries [17].
EVAR has emerged as a promising modality for management for abdominal aortic injuries. In a recent comparative study of 325 BAAIs requiring surgery, Dayama et al., observed a mortality rate of 21% among 91 endovascular cases compared to 67% among 234 cases of open surgical reconstruction [18]. Moreover, patients who underwent laparotomy demonstrated a 6- fold higher risk of mortality compared to the endovascular group [18]. Branco et al., also reported superior in-hospital mortality (12.9% vs 22.4%), and lower rates of sepsis (5.4% vs 7.5%) among endovascular patients [15]. Given the high incidence of concomitant bowel and mesenteric injury, the endovascular approach for BAAI offers significant benefit in lowering risk of implant infection by avoiding direct contamination from intestinal spillage [19].
At present, the infrequent use of endovascular repair for abdominal aortic injuries makes it difficult to perform direct outcome comparisons [18-20]. Special consideration must also be given to the patient selection process [19]. Young individuals with long life expectancy will require routine surveillance to monitor the durability of stent graft material, as well as possible aortic- graft size mismatch from patient growth. The presence of aortoiliac thrombosis may also increase the risk of distal embolization and complicate future stent deployments. Nevertheless, the endovascular management of BAAI can yield excellent results among well-chosen patients who can participate in strict follow-up surveillance protocol.
CONCLUSION
The case described herein illustrates the applicability of EVAR for a limited zone III BAAAI. The EVAR approach offers a safe and effective treatment modality for BAAI that has demonstrated lower risk of in-hospital mortality and sepsis when compared to open surgical reconstruction. The low incidence of BAAI limits our ability to achieve rigorous comparisons between open and endovascular techniques beyond that reported in small series and case reports. However, the published experience should provide guidance for surgeons who may encounter BAAI in their clinical practice and support the availability of EVAR in their centers when cases present with anatomy amenable to this less invasive treatment option.
COI DISCLOSURE
All JTACS Disclosure forms have been supplied and are provided as supplemental digital content.
REFERENCES
- Shalhub S, Starnes BW, Tran NT, Hatsukami TS, Lundgren RS, Davis CW, et al. Blunt abdominal aortic injury. J Vasc Surg. 2012; 55: 1277-1285.
- Shalhub S, Starnes BW, Brenner ML, Biffl WL, Azizzadeh A, Inaba K, et al. Blunt abdominal aortic injury: a Western Trauma Association multicenter study. J Trauma Acute Care Surg. 2014; 77: 879-885.
- de Mestral C, Dueck AD, Gomez D, Haas B, Nathens AB. Associated injuries, management, and outcomes of blunt abdominal aortic injury. J Vasc Surg. 2012; 56: 656-660.
- Gunn M, Campbell M, Hoffer EK. Traumatic abdominal aortic injury treated by endovascular stent placement. Emerg Radiol. 2007; 13: 329-331.
- Sheehan BM, Grigorian A, de Virgilio C, Fujitani RM, Kabutey NK, Lekawa M, et al. Predictors of blunt abdominal aortic injury in trauma patients and mortality analysis. J Vasc Surg. 2020; 71: 1858-1866.
- Dajee H, Richardson IW, Iype MO. Seat belt aorta: acute dissection and thrombosis of the abdominal aorta. Surgery. 1979; 85: 263-267.
- Freni L, Barbetta I, Mazzaccaro D, Settembrini AM, Dallatana R ,Tassinari L, et al. Seat belt injuries of the abdominal aorta in adults--case report and literature review. Vasc Endovascular Surg. 2013; 47: 138-147.
- Ahmed M, Mahmoud A, Samotowka M, Mitchell K, Saeed R. Seat Belt Aortic Dissection: A Case Report. Cureus. 2019; 11: e4662.
- Murat TE, Arslan FD, Kilci A?, Hakkoymaz H, Gedik MS. A Rare Diagnosis After a Traffic Accident Aortic Transection. J Emerg Med Case Rep. 2020; 13: 59-61.
- Charlton-Ouw KM, DuBose JJ, Leake SS, Sanchez-Perez M, Sandhu HK, Holcomb JB, et al. Observation May Be Safe in Selected Cases of Blunt Traumatic Abdominal Aortic Injury. Ann Vasc Surg. 2016; 30: 34-39.
- Kobayashi L, Coimbra R, Goes AMO Jr, Reva V, Santorelli J, Moore EE, et al.. American Association for the Surgery of Trauma-World Society of Emergency Surgery guidelines on diagnosis and management of abdominal vascular injuries. J Trauma Acute Care Surg. 2020; 89: 1197-1211.
- Chang R, Fox EE, Greene TJ, Eastridge BJ, Gilani R, Chunget KK, et al.. Multicenter retrospective study of noncompressible torso hemorrhage: Anatomic locations of bleeding and comparison of endovascular versus open approach. J Trauma Acute Care Surg. 2017; 83: 11-18.
- DuBose JJ, Savage SA, Fabian TC, Menaker J, Scalea T, Holcomb JB, et al.. The American Association for the Surgery of Trauma PROspective Observational Vascular Injury Treatment (PROOVIT) registry: multicenter data on modern vascular injury diagnosis, management, and outcomes. J Trauma Acute Care Surg. 2015; 78: 215-223.
- Murata M, Aoki M, Hagiwara S, Sekihara M, Kohri T, Shibuya K, et al. Successful Endovascular Therapy in an Elderly Patient with Severe Hemorrhage Caused by Traumatic Injury. Open Med (Wars). 2018; 13: 203-207.
- Branco BC, Musonza T, Long MA, Chung J, Todd SR, Wall MJ Jr, et al. Survival trends after inferior vena cava and aortic injuries in the United States. J Vasc Surg. 2018; 68: 1880-1888.
- Kurt D, Ammar C, Ablah E, Lightwine K, Okut H, Lu L, et al. Evaluation of Outcomes and Treatment Options Among Trauma Patients with Abdominal Vascular Injuries. Kans J Med. 2023; 16: 11-16.
- Osgood MJ, Heck JM, Rellinger EJ, Doran SL, Garrard CL 3rd, Guzman RJ, et al. Natural history of grade I-II blunt traumatic aortic injury. J Vasc Surg. 2014; 59: 334- 341.
- Dayama A, Rivera A, Olorunfemi O, Mahmoud A, Fontecha CA, McNelis J. Open and Endovascular Abdominal Aortic Injury Repair Outcomes in Polytrauma Patients. Ann Vasc Surg. 2017; 42: 156-161.
- Gouveia E Melo R, Amorim P, Soares TR, Fernandes E Fernandes R, Ministro A, et al. Clinical aspects and present challenges of the seat belt aorta. J Vasc Surg. 2020; 72: 995-1004.
- Safaya A, Carroll FX, Laskowski IA. Blunt Mesenteric Vascular Injuries: Endovascular Management and Midterm Outcomes. EJVES Vasc Forum. 2021; 53: 9-13.