Spontaneous Dissection of the Coronary Artery: A Cause of Myocardial Infarction not to be forgotten in the Young Subject
- 1. Department of Cardiology, Sylvanus Olympio Teaching Hospital of Lome, Togo
- 2. Department of Cardiology, Campus Teaching Hospital of Lome, Togo
- 3. Autel d’Elie Private Hospital, Lome, Togo
- 4. Department of Cardiology, Kara Teaching Hospital, Togo
ABSTRACT
Myocardial infarction in young people is relatively infrequent and presents etiological and therapeutic problem. We report the case of a 27-year-old patient with no cardiovascular risk factor, no substance abuse, and no family history of cardiovascular event who presented with recurrent atypical chest pain with electrocardiogram repolarization abnormalities as ST elevation in inferior-latero-basal location. Coronary angiography five months later revealed chronic subocclusive stenosis of the ostial left anterior descending artery and normal aspect of others coronary arteries. Coronary artery bypass surgery was indicated and done in Tunisia by anastomosis between the left internal mammary artery and the middle left anterior descending artery. For etiological purposes, we suspected thrombophilia, but the examinations performed were normal, suggesting spontaneous coronary dissection. The postoperative evolution was straightforward.
KEYWORDS
- Coronary heart disease
- Spontaneous dissection
- Young subject
- Lome
CITATION
Afassinou YM, Edorh L, Pessinaba S, Atta B, Sodou A, et al. (2023) Spontaneous Dissection of the Coronary Artery: A Cause of Myocardial Infarction not to be forgotten in the Young Subject. Ann Vasc Med Res 10(1): 1155.
INTRODUCTION
Young person’s myocardial infarction is relatively uncommon [1]. However, it is a public health problem due to the young age of the patients, the cost of its management and its socioeconomic and psychological consequences [2]. Its etiological mechanism is described [3], but there are cases of myocardial infarction of the young subject with undetermined cause [4,5]. Spontaneous dissection of coronary arteries should not be forgotten in this young subject context. We report a case of myocardial infarction in a young subject who posed both an etiological and therapeutic diagnosis problem.
CASE PRESENTATION
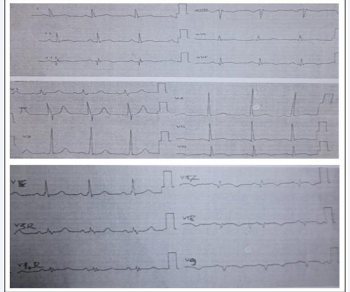
This is a 27-year-old male patient with no cardiovascular risk factor, no substance abuse, and no family history of cardiovascular event (myocardial infarction, sudden death), who had atypical chest pain from a basic thoracic seat, localized, 5/10 intensity burn type analog digital scale, lasting about 20 minutes. A recurrence of pain four days later prompted a medical consultation with an electrocardiogram; the electrocardiogram revealed repolarization abnormalities as ST elevation in the inferior-latero-basal location with posterior negative T-waves and inferior Q-waves (Figure 1).
Figure 1 Resting electrocardiogram at first medical contact showing ST elevation in the inferior-latero-basal location with posterior negative T-waves and inferior Q-wave.
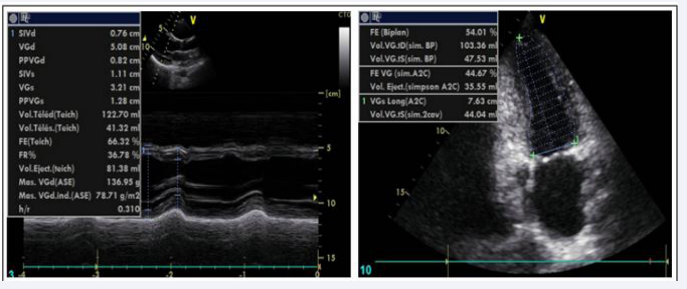
It should be noted that the physical examination was normal. Troponin I performed, was elevated to 454 times normal and C-reactive protein was negative. Cardiac ultrasound was normal with no segmental kinetics abnormalities and good left ventricular systolic function (LVEF=54%) (Figure 2).
Figure 2 Parasternal Echocardiographic Slices with Good Left Ventricle Systolic Function
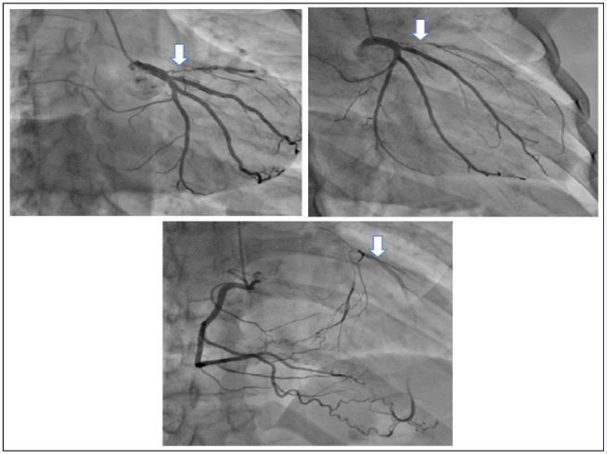
The diagnosis of recent myocardial infarction in inferior- latero-basal was retained. The patient was then put on medical treatment. A requested coronary angiography was performed five months later due to the financial difficulties and geographic accessibility of the exam. It demonstrated chronic subocclusive stenosis of the ostial left anterior descending artery and a normal appearance of the rest of the coronary arteries (Figure 3).
Figure 3 Coronary angiographic images showing chronic subocclusive stenosis of the ostial left anterior descending artery collateralized by the right coronary artery rentrop 3.
Coronary artery bypass surgery was indicated and performed in Tunisia by anastomosis between the left internal mammary artery and the middle left anterior descending artery. Etiologically, we suspected thrombophilia because of his young age, the absence of cardiovascular risk factor and the totally isolated aspect of the coronary lesion, and performed the assay of the protein C, protein S, antithrombin III, homocysteinemia, antiphospholipid antibodies, looking for factor II G20210A mutation and factor V Leiden. All these tests were normal. Human immunodeficiency virus serology, hepatitis B and C virus testing were also normal. Prior to these normal examinations and the isolation of the coronary artery lesion and its appearance, spontaneous coronary dissection was retained. The post-operative evolution was simple. Short and medium term developments have been favourable.
DISCUSSION
Male predominance is found in the infarction of the young black subject and our concerns a young male [6]. In the Western series, the majority of young patients with myocardial infarction have at least one of three risk factors: male sex, active smoking, and/or early coronary inheritance [7], but also drug use [8]. No other etiologic factors were discovered in this case. The coronary appearance clearly suspected spontaneous coronary dissection. The pathogenesis of coronary disease in the young person describes many mechanisms: atherosclerosis linked to traditional cardiovascular risk factors similar to those of the elderly, recreational drug use, coronary embolism, Atheromatous coronary artery disease without critical coronary stenosis or coronary vasospasm, but also congenital abnormalities of coronary arteries and states of hypercoagulability [3,4,9,10]. In our context, intravascular coronary imaging would have made it possible to better visualize the lesion, confirming the cause of this myocardial infarction in this young subject.
Our case, apart from the problem of etiologic diagnosis, also posed a problem of therapeutic management; angioplasty or bypass. The coronary lesions in our case were not acute and according to the recommendations of the European Society of Cardiology on myocardial revascularization, angioplasty and bypass surgery were indicated to the same degree [11]. We preferred bypass surgery considering the patient’s young age, appearance and location of the lesion, which poses a significant risk to the left main artery and circumflex artery in angioplasty. An unusual case was described by van der Schoot et al., [5]. In the Netherlands in a 27-year-old subject with a similar profile to ours who had chest pain radiating to both arms associated with nausea and vomiting with admission, repolarization to the resting electrocardiogram and a normal troponin at the first time. The evolution was marked by the sudden occurrence of successfully resuscitated ventricular fibrillation and an ST segment elevation.
Coronary angiography revealed that the left anterior descending artery was occluded and repaired by angioplasty. In the acute phase, angioplasty is the most indicated treatment especially in case of over-added complication. This angioplasty could have been chosen for us. But etiology remains an element of choice. If it is simple to perform in the case of an acute coronary lesion, this does not seem to be the case in spontaneous dissection.
The short-term prognosis in our case was good as in the literature [6,12,13]. But rigorous surveillance of this patient is essential because of the long-term, pejorative prognosis of coronary disease in young patients [14,15].
FINDING
This case highlights the difficulty in the etiological diagnosis of myocardial infarction in young subjects. Despite this, it was possible to retain the diagnosis of spontaneous coronary dissection on strong arguments in our context where explorations are very limited.
CONCLUSION, LIMITATIONS AND RECOMMENDATIONS
Myocardial infarction is a coronary disease that poses a real etiological problem as in our patient. The difficulty is partly facilitated by the delay in performing coronary angiography and others explorations. Intravascular coronary imaging would have enabledustobettervisualizethe lesion, confirming thecauseofthis disease in this young subject. However, spontaneous dissection of the left anterior descending artery appears as the most obvious etiology. To this, is added a therapeutic difficulty with the choice of bypass which seems to us to be the best decision, with good immediate prognosis. As a recommendation, given the limited means in the exploration of coronary lesions in our countries, it is essential to properly analyze coronary angiographies lesions and to help if possible experts in interventional cardiology. It is also necessary to think of spontaneous coronary dissection in young subjects without cardiovascular risk factors.
ACKNOWLEDGEMENTS
Thank you for facilitating these coronary explorations at the Autel d’Elie Private Hospital.
REFERENCES
- Trzos E, Uzna?ska B, Rechci?ski T, Krzemi?ska-Paku?a M, Buga?a M, Kurpesa M. Myocardial infarction in young people. Cardiol J. 2009; 16: 307–11.
- Zeitouni M, Collet J. Infarctus du sujet jeune : quel bilan étiologique spécifique ? Quel suivi ? Réal Cardiol. 2022.
- Gulati R, Behfar A, Narula J, Kanwar A, Lerman A, Cooper L, et al. Acute Myocardial Infarction in Young Individuals. Mayo Clin Proc. 2020; 95: 136–56.
- Egred M, Viswanathan G, Davis GK. Myocardial infarction in young adults. Postgrad Med J. 2005; 81: 741–5.
- van der Schoot GGF, Anthonio RL, Jessurun GAJ. Acute myocardial infarction in adolescents: reappraisal of underlying mechanisms. Neth Heart J. 2020; 28: 301–8.
- Nobila Valentin Y, Mouhamadou Bamba N, Alassane M, Rajaa B, Larissa Justine K, Malick B, et al. L’infarctus du myocarde du jeune adulte -Analyse rétrospective des cas colligés au CHU de Dakar. Pan Afr Med J. 2010; 6: 21.
- Tea V, Danchin N, Puymirat E. Myocardial infarction in young patient:Epidemiological specificities and risk factors. La Presse Médicale.2019; 48: 1383–6.
- Rizk T, Blankstein R. Not All Heart Attacks are Created Equal: Thinking Differently about Acute Myocardial Infarction in the Young. Methodist DeBakey Cardiovasc J. 2021; 17: 60–7.
- Osula S, Bell GM, Hornung RS. Acute myocardial infarction in youngadults: causes and management. Postgrad Med J. 2002; 78: 27–30.
- Benzarouel D, Benyass A, Rabhi M, Chaari J, Boukili A, Hamani A. Infarctus du myocarde silencieux chez une jeune femme de 18 ans présentant un syndrome des anticorps antiphospholipides. Ann Cardiol Angéiologie 2007; 56: 313–5.
- Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019; 14: 1435–534.
- renier O, Cambou JP, Ferrières J, Thomas D, Amelineau E, Cantet C, et al.Caractéristiques initiales et prise en charge thérapeutique des sujets jeunes (âge inférieur à 45 ans) hospitalisés pour syndrome coronaire aigu : résultats des études françaises PRÉVENIR 1 et PRÉVENIR 2. Ann Cardiol Angéiologie. 2002; 51: 15–9.
- Fournier JA, Sánchez A, Quero J, Fernández-Cortacero J, González- Barrero A. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. 1996; 19: 631-636.
- Fournier JA, Cabezón S, Cayuela A, Sm B, Cortacero J, Díaz De La Llera LS. Long-term prognosis of patients having acute myocardial infarction when =40 years of age. Am J Cardiol. 2004; 94.
- Awad-Elkarim AA, Bagger JP, Albers CJ, Skinner JS, Adams PC, Hall RJC. A prospective study of long term prognosis in young myocardial infarction survivors: the prognostic value of angiography and exercise testing. Heart. 2003; 89: 843–7.