“Modified Sandwich” Technique in the Surgery of Acute Type A Aortic Dissection
- 1. Medical postgraduate students, Hebei Medical University Third Hospital, China
ABSTRACT
Objective: To observe the therapeutic effect of the “modified sandwich” root shaping technique using an artificial vascular sheet in acute type A aortic coarctation surgery.
Methods: We retrospectively analyzed the clinical data of 28 patients with acute type A aortic coarctation who were treated with an artificial vascular sheet using the “modified sandwich” method. The operation and postoperative conditions were statistically analyzed.
Results: All 28 patients underwent successful surgery with an extracorporeal circulation time of 265.0 (210.0 - 322.5) min, an aortic block time of 151.0 (112.0 - 209.0) min, and a drainage flow rate of 237.5 (126.0 - 297.0) mL at 12 hours postoperatively. There were 2 (7.1%) perioperative deaths caused by renal failure, ischemia in 1 case, and coronary artery causes in 1 case. Postoperative complications included reopening of the chest for hemostasis in 1 case (3.6%) for reasons unrelated to the vascular anastomosis, hemodialysis in 3 cases (10.7%), paraplegia in 1 case (3.6%), and cerebral infarction resulting in impaired mobility of the left upper extremity in 1 case (3.6%). Tracheotomy was performed in 1 case (3.6%), and the duration of mechanical ventilation was 89 (48.0 - 165) h. Among the 26 recovered patients reviewed with aortic enhancement CT before discharge, the artificial vascular anastomosis had smooth blood flow, though 1 case still had residual entrapment in the sinus of the aorta.
Conclusion: In acute type A aortic coarctation surgery, the “modified sandwich” technique using an artificial vascular sheet for aortic root shaping is simple, effective, and easy to master. This method can reduce anastomotic blood seepage and prevent anastomotic tear and bleeding, making it worth recommending for clinical application.
KEYWORDS
- Acute type A aortic coarctation
- Artificial vascular slice
- Modified sandwich method
CITATION
Kong J, Liu T, Li Z, Xi S, Liu L (2024) “Modified Sandwich” Technique in the Surgery of Acute Type A Aortic Dissection. Ann Vasc Med Res 11(2): 1182.
INTRODUCTION
Acute type A aortic coarctation is a highly aggressive and life- threatening condition. According to Li et al. [1], if surgery is not performed promptly, patients face a mortality rate as high as 50% within 48 hours. Nonetheless, the procedure itself is complex and high-risk, and the complete resection of the root lesion in the aortic wall, aimed at eliminating residual entrapment, is difficult to achieve in most cases. Therefore, reinforcing the lesion-affected and fragile proximal aortic wall to establish a strong anastomotic zone is crucial. This step is essential to prevent pinhole tearing of the anastomosis, rupture bleeding, or malignant coronary events caused by sustained pressure increases within the residual entrapment, ensuring procedural safety.
Since the 1970s, a series of techniques for aortic root reinforcement and prevention of bleeding have been developed, including simple continuous suture apposition to fix separated inner and outer membranes, the sandwich technique and its various modifications, internalization of the outer membrane, flip anastomosis of artificial blood vessels, and the use of medical adhesives [2-5]. Prof. Liu Kexiang, a scholar from our country, used an artificial vascular sheet with a width of 1.5-2.0 cm for sandwich reinforcement and root molding, which effectively closed the proximal remnant of the sandwich and significantly reduced the risk of intraoperative bleeding and false lumen compression of the coronary artery [6]. However, the steps of continuous horizontal mattress transmural foldback suture at the lower edge of the sandwich and longitudinal suture between the upper and lower edges of the artificial vascular sheet are cumbersome and time-consuming. Thus, we simplified the suture fixation method of the artificial vascular sheet sandwich and still achieved good clinical efficacy. We now present our treatment experience and discuss the effectiveness of this method for clinical reference.
INFORMATION AND METHODS
General information
From October 2020 to November 2022, 28 patients with acute type A aortic coarctation underwent surgical treatment in the Department of Cardiovascular Surgery at the Third Hospital of Hebei Medical University. Root shaping was performed using the “modified sandwich” method with artificial vascular sheets during the operation. Among the 28 patients, 18 were male and 10 were female. The average BMI was (27.29 ± 4.25) kg/m². Twenty- two patients had hypertension, 1 had diabetes mellitus, and 1 had coronary artery disease. The left ventricular ejection fraction (EF) was 61.0% ± 4.8%. Preoperative routine examinations revealed: serum creatinine (Cr) 92.70 (57.58 - 109.72) μmol/L, urea 2.375 (5.05 - 7.425) mmol/L, total bilirubin 17.94 (13.0230.96) μmol/L, alanine aminotransferase (ALT) 11.5 (15.026.5) U/L, and aspartate aminotransferase (AST) 34.5 (22.0 - 45.25) U/L. All patients underwent preoperative aortic CTA and echocardiography to establish the diagnosis, assess the extent of entrapment involvement, evaluate vascular involvement of each important branch, measure the diameters of each aortic segment, and select the site for arterial cannulation. The Ethics Committee of the Third Hospital of Hebei Medical University approved the study and granted an exemption from written informed consent.
Surgical methods
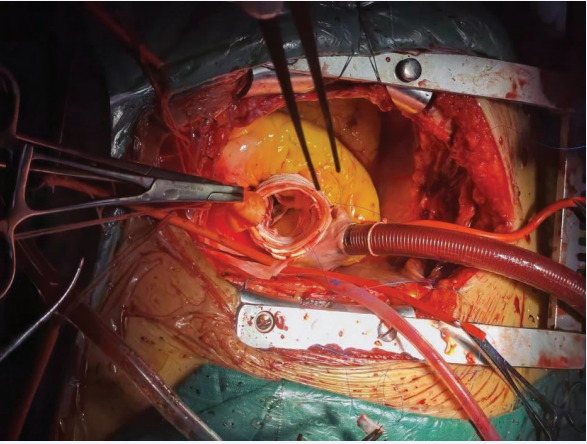
A median chest incision was performed to longitudinally split the sternum and access the chest. Three cephalic and brachial arteries were then dissected and freed. Extracorporeal arterial perfusion was conducted using a single pump and two cannulas: one through the femoral artery for extracorporeal circulation and the other for selective cerebral perfusion. After establishing extracorporeal circulation, cooling was initiated. The ascending aorta was occluded and longitudinally dissected. HTK myocardial protection fluid was infused through the right and left coronary artery openings. The thrombus in the entrapment was removed, the ascending aorta was transected 1.5-2 cm above the sinus- tubular junction, and the aortic root was dissected to the right and left coronary arteries above the main trunks. Initially, the sinus was examined for entrapment, avulsion of the junction, and involvement of the coronary openings. The root was then injected with water to verify the integrity of the inner and outer membranes and to assess any lesion soft aortic valve. If the lesion was suitable for root reinforcement molding, the artificial blood vessel was selected based on the diameter of the root ascending aorta and sinotubular junction. Three 1.5-cm-wide vascular rings were cut from the artificial vessel. One ring was placed with the intima against the proximal dissected end of the ascending aorta, while the other two strips were cut longitudinally and attached to the outer side of the dissected vessel. The remaining artificial vessels were trimmed into appropriately shaped and sized spacers and placed between the inner and outer membranes of the avulsed coronary sinus and sinotubular junction. Each vascular piece was adjusted to fit properly against the aortic wall. The lower edge of the sandwich was then secured with a three- needle 4-0 Prolene suture in three equal interrupted mattress seams above the sinotubular junction (noting that the first stitch was placed over the opening of the left coronary artery). One of the sutures was then used to create a continuous horizontal mattress suture along the level of the sinotubular junction, followed by another continuous horizontal mattress suture along the upper edge of the sandwich. The medial prosthetic vascular sheet was examined and trimmed as necessary if it affected the coronary artery openings. In cases where the leaflet junction was affected by the sandwich and avulsion led to aortic closure insufficiency, a 4-0 double-needle mattress suture with a spacer was used to suspend the aortic valve junction. A water injection test was performed to observe aortic valve closure. If any part of the coronary opening was involved in the sandwich, it was fixed with interrupted mattress sutures using a 5-0 Prolene thread. The upper edge of the sandwich was then neatly trimmed with scissors, ensuring that the layers of the artificial vascular sheet and the wall of the autologous aorta were properly aligned. Care was taken not to damage the upper edge of the suture line (Figure 1). The distal end of the sandwich was treated with either classic full arch replacement with stenting and elephant trunk surgery, simple ascending artery replacement, or half-arch replacement, depending on the extent of sandwich involvement. Selective cerebral perfusion was performed during a deep hypothermic shutdown cycle. Following distal treatment, the proximal end of the four-branched artificial vessel was anastomosed to the proximal ascending aorta using 3-0 Prolene sutures. After venting, the blocking clamp was removed, extracorporeal circulation was gradually discontinued, and cardioversion was performed.
Figure 1 Completion of root treatment.
Statistical analysis
Statistical analysis was conducted using SPSS 22.0 software. Measurements with a normal distribution were expressed as mean ± standard deviation (mean ± SD). For data not following a normal distribution, values were presented as median and interquartile range (IQR). Categorical data were reported as frequency or percentage (%).
RESULTS
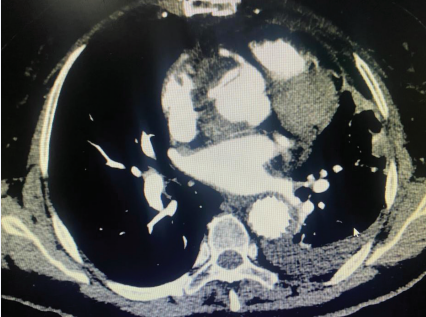
In our cohort, 28 cases of acute type A aortic coarctation underwent intraoperative “modified sandwich” root shaping with artificial vascular slices. Among these cases, 24 patients received total arch replacement with stenting and elephant trunk surgery, 4 patients had ascending aorta replacement with a small curvature of the arch under deep hypothermic shutdown, and 1 patient required coronary bypass grafting due to severe involvement of the right coronary artery opening. All 28 patients successfully completed their surgical treatment. The operative time was 9.5 (8.0 - 12.2) hours, including selective cerebral perfusion time of 23.0 (8.0 - 35.0) minutes, intraoperativeextracorporeal circulation time of 265.0 (210.0 - 322.5) minutes, and aortic occlusion time of 151.0 (112.0 - 209.0) minutes. Postoperative awakening time for 21 patients was 36.0 (33.0 - 81.5) hours, endotracheal intubation time was 88.6 (55.5 - 172.1) hours, and postoperative ICU stay was 124.7 (89.9 - 185.1) hours. There were 2 perioperative deaths (7.1%): one due to renal failure and abdominal ischemia, and the other due to coronary artery causes. At 24 hours postoperatively, serum creatinine (Cr) was 104.19 (81.70 - 149.30) μmol/L, urea was 9.76 (6.44 13.45) mmol/L, total bilirubin was 52.28 ± 24.75 μmol/L, alanine aminotransferase (ALT) was 24.5 (19.0 - 43.0) U/L, and aspartate aminotransferase (AST) was 56.0 (38.0 - 114.0) U/L in 26 patients. Postoperative complications included reopening of the chest for hemostasis in 1 case (3.6%) due to reasons unrelated to the vascular anastomosis, hemodialysis in 3 cases (10.7%), paraplegia in 1 case (3.6%), cerebral infarction with impaired mobility of the left upper extremity in 1 case (3.6%), and tracheotomy in 1 case (3.6%). Of the 26 recovered patients, aortic enhancement CT prior to discharge showed that blood flow through the prosthetic anastomosis was smooth, although 1 case still had residual entrapment in the aortic sinus (Figure 2).
Figure 2 Residual entrapment in the sinus of the aorta.
DISCUSSION
Acute type A aortic coarctation is an aggressive condition with a poor prognosis, challenging treatment, and a high propensity for serious complications, including poor organ perfusion and acute kidney injury [7-9]. With the rapid advancements in technology and material science, the surgical success rate for acute type A aortic coarctation has improved significantly. According to the International Registry of Acute Aortic Clamping, the surgical success rate has reached 90%, while the mortality rate has decreased from 25% in 1995 to 18% in 2013 [10]. However, a multicenter study revealed that Chinese patients with acute type
A aortic coarctation experience a longer interval between onset and hospital arrival but have relatively lower early mortality rates. This study suggests the presence of a significant survivor bias among Chinese patients with acute type A aortic coarctation [11]. This implies that patients who reach the hospital alive for treatment may possess certain physiological or pathological advantages, while those who do not reach the hospital in a timely manner during the early stages may be excluded from the statistics, potentially leading to an underestimation of the overall mortality rate. In China, only 52.6% of patients with acute type A aortic coarctation received surgical treatment, indicating a need for enhanced efforts to promote and popularize surgical interventions [12].
One of the keys to achieving surgical success is the prevention of uncontrollable intraoperative hemorrhage, particularly in the proximal anastomosis at the aortic root, where the risk of hemorrhage is significantly increased by the presence of residual entrapment and a high-pressure environment. Management of the aortic root entails the following: effective closure of the false lumen, protection of the valve and coronary arteries, and establishing a stable and robust proximal anastomotic area. If an intimal tear or imprecise suture results in incomplete closure of the false lumen, continued blood flow can trigger root dilatation, which can lead to tearing of the sinusoidal dissection and uncontrollable bleeding. This situation can compress the coronary artery openings, leading to difficult cardiac arrest, and can even jeopardize the patient’s life. Therefore, meticulous attention to every detail of the aortic root during surgery is essential to prevent postoperative complications and to ensure the success of the procedure [13].
The aortic wall is extremely fragile due to entrapment lesions, often requiring reinforcement to ensure a safe closure. In 1966, Gerbode et al. [14], introduced the “sandwich” method of aortic root reinforcement, utilizing Teflon felt strips on both the inner and outer sides of the diseased aortic wall to securely affix the detached membranes, thus forming a “sandwich”-like structure. This technique employs Teflon felt strips to securely join the separated inner and outer aortic membranes, forming a robust structure. It has undergone improvements since its introduction and remains widely used. For instance, Cachera et al. [15], suggested using wider felt strips; in China, Prof. Xu Zhiyun applied this method to completely cover the entire non-coronary sinus and eliminate its pseudo-lumen, effectively preventing tears in the intercalated tissues and blood seepage. However, the expansion of the felt strips may complicate needle entry and suturing, posing risks of aortic stenosis, hemolysis, and thromboembolism [16-18]. These concerns must be carefully considered and addressed in clinical practice. Consequently, Gaeta et al. [19], began using polyester artificial vascular strips, which offer better flexibility and maneuverability, thus alleviating needle entry difficulties and facilitating smoother suturing. Moreover, polyester material exhibits greater stability in response to blood swelling, potentially reducing the risk of aortic complications. Prof. Kexiang Liu [6], employed artificial vascular sheets measuring 1.5-2.0 cm in width to reinforce the
aortic root stump during surgery, demonstrating significant improvements in procedural outcomes. A 4-0 thread continuous horizontal mattress, transmural foldback suture was utilized at the lower edge of the “sandwich” structure at the sinotubular junction and at the upper edge in the plane of the aortic dissection. Additionally, 3-5 longitudinal mattress sutures were employed within the sandwich structure to separate the false lumen. This method was employed in our previous clinical practice, proving to be easy to perform, master, and effective, thus providing reliable technical support for the operation. Aortic valve closure insufficiency, often resulting from acute type A aortic coarctation, is primarily due to intimal avulsion at the leaflet junction, with the right atrioventricular junction avulsion being particularly common. In patients exhibiting normal aortic valve leaflet activity, absence of organic lesions, and a normal aortic valve structure without significant left ventricular enlargement on preoperative ultrasound, aortic valve junction suspension can typically be conducted intraoperatively using a 4-0 double-ended needle with spacers in a mattress suture technique to achieve satisfactory aortic valvuloplasty outcomes. Following the suspension, a water injection test is conducted to assess aortic valve closure and confirm recovery of valve function. Furthermore, employing continuous sutures on the upper and lower margins can induce a ring contraction effect on the sinotubular junction widening due to entrapment, positively impacting the restoration of sinus morphology and enhancing aortic valve function. The study results indicated that the procedure was effective. In this cohort,
23 patients presented with varying degrees of aortic valve closure insufficiency preoperatively; postoperatively, aortic regurgitation was completely resolved in 13 patients, while the remainder exhibited only mild aortic regurgitation. This suggests that aortic valve junction suspension possesses a high success rate and significant clinical value in managing aortic valve closure insufficiency attributable to entrapment.
One patient in our group succumbed postoperatively due to coronary causes. In this case, a significant dilatation of the sinus epithelium, but not of the intima, was observed intraoperatively, resulting in a mismatch between the inner and outer dimensions. The entrapment involved the right coronary artery opening, identified as a Neri A-type lesion; however, this opening was not reinforced intraoperatively. Despite smooth cardiac rebeating and shutdown during the procedure, a significant hematoma was discovered in the aortic sinus and part of the right sinus during chest closure. The patient’s circulation remained stable during the postoperative night; however, the following morning, he developed anuria accompanied by unsustainable blood pressure and elevated central venous pressure. Bedside ultrasound revealed right ventricular distension and dyskinesia, and additional bedside electrocardiography along with myocardial injury marker testing confirmed an inferior wall myocardial infarction. We hypothesized that the cause was likely due to a sinus hematoma compressing the right coronary artery opening. Reflecting on this case, the patient’s sinus dilated to a diameter exceeding 45 mm, whereas the intima-media was not significantly dilated, resulting in a severe mismatch that precluded effective use of the “sandwich” method for root angioplasty. Upon opening the aorta, the sinus membrane, lacking support from the outer membrane, is susceptible to the high-pressure blood flow from the aortic root, potentially leading to endothelial tearing at the needle site and blood ingress into the sandwich’s pseudo- cavity, with serious consequences. For these patients, in the absence of primary valve pathology and without undergoing root replacement or David’s surgery, it is advisable to reinforce the inner lining of the uncinate sinus with a patch, or to customize shims to the shape of the uncinate sinus, lining both its inner and outer sides. The “sandwich” reinforcement of the uncrowned sinus effectively covers and eliminates its pseudocavity, thus diminishing the risk of postoperative complications and enhancing the procedure’s safety and efficacy [20,21].
This study is a retrospective case series, limited by its small number of cases and the lack of mid- and long-term follow-up data. The artificial vascular sheet “modified sandwich” method for root shaping, used in the study, was performed above the level of the sinotubular junction. However, when the aortic sinus is affected by the sandwich method, the separation between the inner and outer membranes persists. Therefore, the incidence of postoperative residual sinus entrapment and the progression of sinus lesions over the long term necessitate further observation and study.
CONCLUSION
In conclusion, the application of the “modified sandwich” method in acute Stanford A aortic dissection root planing has been satisfactory. This method is straightforward to implement, simple to master, and highly valuable for widespread adoption, potentially enabling more hospitals to perform this surgery and thereby extending valuable treatment time for patients.
REFERENCES
- Saw LJ, Lim-Cooke MS, Woodward B, Othman A, Harky A. The surgical management of acute type A aortic dissection: Current options and future trends. J Card Surg. 2020; 35: 2286-2296.
- Li Liangpeng, Huang Fuhua, Su Cunhua. Application of partial aortic root reconstruction in acute Stanford type A aortic dissection. Chinese Clin J Thorac Cardiovasc Surg. 2017; 24: 506-511.
- Meng Maolong, Ma Qiong, Li Gang, Wang Xiang, Zhuang Xianmian, Lu Pingping. Application of adventitial inversion sinus plasty in the surgical treatment of acute Stanford type A aortic dissection. Chinese J Circulation. 2021; 36: 596-600.
- Guo Yingqiang, Zhang Eryong, Meng Wei, Shi Yingkang. Improvement of aortic end reinforcement method in acute type A aortic dissection surgery. Chinese Clin J Thoracic Cardiovasc Surg. 2009; 16: 389-391.
- Kaya E. Reinforcement of suture lines with aortic eversion in aortic replacement. Cardiovasc J Afr. 2018; 29: 12-45.
- Zhu C, Piao H, Wang Y, Wang T, Li D, Xu R, et al. A New Aortic Root Reinforcement Technique for Acute Type A Aortic Dissection Surgery. Int Heart J. 2019; 60: 1131-1136.
- Osada H, Minatoya K. Overview of acute type A dissection in Japan. Indian J Thorac Cardiovasc Surg. 2023; 39: 280-286.
- Zhou H, Wang G, Yang L, Shi S, Li J, Wang M, et al. Acute Kidney Injury After Total Arch Replacement Combined With Frozen Elephant Trunk Implantation: Incidence, Risk Factors, and Outcome. J Cardiothorac Vasc Anesth. 2018; 32: 2210-2217.
- Rylski B, Schilling O, Czerny M. Acute aortic dissection: evidence, uncertainties, and future therapies. Eur Heart J. 2023; 44: 813-821.
- Wang W, Duan W, Xue Y, Wang L, Liu J, Yu S, et al. Clinical features of acute aortic dissection from the Registry of Aortic Dissection in China. J Thorac Cardiovasc Surg. 2014; 148: 2995-3000.
- Zhao R, Qiu J, Dai L, Song J, Fan S, Cao F, et al. Current Surgical Management of Acute Type A Aortic Dissection in China: A Multicenter Registry Study. JACC Asia. 2022; 2: 869-878.
- Sun Lizhong, Li Jianrong. Progress and challenges in the diagnosis and treatment of Stanford type A aortic dissection in my country. Chinese J Surg. 2017; 55: 241-244.
- Yang B, Malik A, Waidley V, Kleeman KC, Wu X, Norton EL, et al. Short- term outcomes of a simple and effective approach to aortic root and arch repair in acute type A aortic dissection. J Thorac Cardiovasc Surg. 2018; 155: 1360-1370.e1.
- Gerbode F, SGS, Hill JD. Aneurysms of the Ascending Aorta: A Method of Reconstructing the Aortic Root. Ann Thoracic Surg. 1966; 2: 525- 531.
- Cachera JP, PRV, Loisance DY. Surgical management of acute dissections involving the ascending aorta. J Thorac Cardiovasc Surg. 1981; 82: 576-584.
- Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ. Dissection of the aorta and dissecting aortic aneurysms. Improving early and long- term surgical results. Circulation. 1990; 82: IV24-38.
- Sakaguchi M, Takano T. Hemolytic anemia caused by aortic flap and inversion of felt strip after ascending aorta replacement. J Cardiothorac Surg. 2016; 11: 117.
- Sogawa M, Moro H, Namura O, Ishiyama T, Hayashi J. Thrombus on the intraluminal felt strip. A possible cause of postoperative stroke. Jpn J Thorac Cardiovasc Surg. 2001; 49: 333-335.
- Gaeta R, Lentini S, Tancredi F, Monaco F, Savasta M. Surgery for acute aortic dissection: an easy and cheap method to reinforce the anastomosis. J Card Surg. 2009; 24: 173-174.
- Chen LW, Wu XJ, Li QZ, Dai XF. A modified valve-sparing aortic root replacement technique for acute type A aortic dissection: the patch neointima technique. Eur J Cardiothorac Surg. 2012; 42: 731-733.
- Tang Y, Liao Z, Han L, Tang H, Song Z, Xu Z. Long-term results of modified sandwich repair of aortic root in 151 patients with acute type A aortic dissection. Interact Cardiovasc Thorac Surg. 2017; 25: 109-113.