Childhood Adversities in Men with Schizophrenia: Dose -Response vs. Trauma Specific Hypothesis
- 1. José T. Borda Hospital, Argentina
- 2. Braulio A. Moyano Hospital, Argentina
Abstract
Introduction: Multiple studies have found that suffering from adverse experiences during childhood is associated with the development of mental diseases, substance abuse, poor physical health and negative repercussions in social functioning. Patients diagnosed with schizophrenia have higher rates of traumatic experiences during childhood than the general population. The current study aims to determine the clinical repercussion of adverse childhood experiences in a male schizophrenic sample and to compare different clinical characteristics among patients who suffered a specific trauma versus those who were victims of multiple types of adverse experiences during childhood. 1.2. Methods
An observational descriptive cross-sectional study was conducted at Jose T. Borda Hospital, in Buenos Aires, Argentina. Participants included 51 male patients between 18 - 63 years with a diagnosis of schizophrenia. Semi-structured interviews were taken, including SCID I and II to assess psychiatric diagnosis, a socio-demographic questionnaire and the Adverse Childhood Experiences (ACE) Questionnaire to evaluate the presence of adverse childhood experiences.
Results: We found that 94% of participants had experienced at least one adverse childhood experience. Sixty three percent of the sample suffered from four or more disruptive child events. We observed that sexual abuse and physical neglect increase the risk of substance abuse and auditory hallucinations, respectively. We also found a statistically significant relationship between patients who suffered from multiple adverse events and the presence of auditory hallucinations and the abuse of substances.
Citation
Vallejos M, Cesoni OM, Farinola R, Prokopez CR (2017) Childhood Adversities in Men with Schizophrenia: Dose-Response vs. Trauma Specific Hypothesis. Arch Paediatr Dev Pathol 1(1): 1002.
Keywords
• Adverse childhood experiences
• Men
• Schizhophrenia
• Adverse childhood experiences questionnaire
INTRODUCTION
Childhood adversity in patients with schizophrenia
Suffering adverse experiences during childhood increase the risk of developing physical diseases, aggressive behavior and psychiatric disorders in adulthood [1,2]. Given its high prevalence, it is likely that child abuse is a major factor in developing mental pathologies [1,2].
Several authors argue that individuals with a history of traumatic events in childhood rarely experience a single traumatic event, being more likely to suffer several traumatic episodes [3]. Numerous investigations show that 69% of children suffering from child abuse experience an average of three different types of adverse events in childhood [4].
Several studies show a higher prevalence of childhood traumatic events among psychotic patients in comparison with the general population. The rates varies between 45- 90% among schizophrenic patients [5-13]. Two hypotheses try to explain how child abuse influences on the psychic structuring and on the onset of clinical and mental diseases.
The first one postulates that the greater the number of types of trauma suffered, the greater the clinical and social repercussion [2,14,15]. People who were exposed numerous times to different severe events have a higher risk of developing psychosis, suggesting a dose-response relationship among trauma/ psychosis instead of a trauma specific hypothesis [5,8,11,16-18]. Supporting this hypothesis, Feletti et al. created the Adverse Childhood Experiences questionnaire (ACE) [2]. The ACE score has been framed by its creators as “a measure of the cumulative exposure to traumatic stress during childhood” and they emphasize the importance of cumulative burden and downplay the importance of exposure to specific types of maltreatment [14,19]. Moreover, many studies have linked the presence of multiple adverse childhood events in schizophrenic patients with an increase in substance abuse, psychotic symptoms, hospitalizations and a poor outcome [5,9,11,13,20-22].
On the other hand, the second hypothesis proposes that susceptibility is strongly dependent on the type and timing of maltreatment with a maximum vulnerability emerging to a specific type of abuse during a narrow sensitive exposure period. These authors argue that the exposure to a specific type of maltreatment at a certain age is a more relevant predictor than its multiplicity. Several studies also suggest a particularly deleterious role for a very early or lengthy exposure [23-25]. Some studies found that the exposure to a specific type of maltreatment during a narrow developmental stage is better as a predictor than over-all measures of exposure, such as severity, duration, or multiplicity [25]. A significant number of studies, using unbiased whole brain analyses, have shown that exposure to specific types of maltreatment selectively target sensory systems most involved in perceiving the experience [26-29].
A few studies have shown evidence that one type of maltreatment may be a stronger risk factor in comparison with others for a specific outcome, both in general population and in patients with mental disorder. However, there is no agreement in which type of trauma is associated with a specific outcome [5,10,11,24,30-32].
The aim of this study is 1) to determine the prevalence of each subtype of trauma in a men sample diagnosed with schizophrenia 2) to determine the prevalence of those individuals who suffered 4 or more types of adverse events 3) to correlate both groups with clinical variables.
METHOD
Study design
The present study is a descriptive-observational, crosssectional study conducted at Dr. Tiburcio Borda Hospital. This is a male’s neuropsychiatric hospital and serves a large urban catchment area in Buenos Aires, Argentina, and predominantly uninsured patients.
All procedures performed in studies involving human participants are in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The present study was approved by the ethics committee of José T. Borda Hospital.
Procedure
Interviews were conducted by three psychiatrists (MV, OC and RF). All psychiatrists were trained to take the semi-structured interview administered as part of the study protocol. Initial evaluation was performed to determine if patients met inclusion criteria: (a) age between 18 and 65 years and (b) diagnosed with schizophrenia. Patients were excluded if they (a) were unable to respond autonomously (i.e., due to sedative effects of medication or language limitations), (b) suffered delusions at the time of the study. All patients who agreed to participate provided a written informed consent.
Measures
Each patient underwent a semi-structured interview with a psychiatrist from the research team. It included questions related to clinical and demographic variables. Structured Clinical Interview for DSM (SCID I and II) was used to assess the psychiatric disorder in Axis I and II [34].
Patient history of childhood trauma: Information about childhood experiences were collected through questions selected from the Adverse Childhood Experiences study (ACE) [2], (translated into Spanish by Carolina Whitelegg and backtranslated by Gabriela Kardos). The questionnaire consists of 10 questions about the presence of different types of trauma before 18 years. The maximum score is ten and a higher score indicates a greater number of adverse childhood experiences suffered during childhood. The questionnaire explores the history of physical, emotional and/ or sexual abuse, the history of physical and/ or emotional neglect and the presence of psychiatric disorders and family legal problems. It includes the following variables:
Childhood abuse: One question related to the experience of each of the following forms of abuse: physical (being hit or beaten), emotional (being threatened, frightened, belittled, neglected), and sexual (being touched against your will, threatened to do things against your will, being abused sexually). Responding ‘often’ or ‘sometimes’ on any of the types of abuse was taking as indicating experience with this sort of abuse.
Childhood neglect: Divided into emotional and physical neglect, measured by five questions each. The questions measuring emotional neglect were: (1) ‘Nobody in my family helped me feel important or special’, (2) ‘I did not feel loved’, (3) ‘People in my family did not look out for each other’, (4) ‘People in my family did not feel close to each other’, (5) ‘My family was not a source of strength and support’. Responding ‘often’ or ‘sometimes’ on any of the questions was considered an indicator of emotional neglect. The questions measuring physical neglect were: (1) ‘I did not have enough to eat’, (2) ‘I knew there was not someone there to take care of me and protect me’, (3) ‘My parents were too drunk or too high to take care of me’, (4) ‘I had to wear dirty clothes’, (5) ‘There was not someone to take me to the doctor if I needed it’. Responding ‘often’ or ‘sometimes’ on any of the questions was considered an indicator of physical neglect.
Household dysfunction: Measured by the following variables:
- Witnessing intimate partner violence: (1) ‘Did you ever hear or see that your father or your mother’s partner abusing your mother physically, emotionally or sexually?’, (2) ‘Did you ever hear or see that your mother or your father`s partner abusing your father physically, emotionally or sexually?’. Responding ‘often’ o ‘sometimes’ to one or both of these questions was considered evidence of having witnessed intimate partner violence.
- Household substance abuse: Measured by two questions: ‘Have you ever lived with (1) an alcoholic or problem drinker? (2) ‘Someone using drugs?’. Affirmative responses to one or both of these questions were taken as evidence of being exposed to household substance abuse.
- Parental separation, divorce or death: Measured by responding ‘yes’ to the question: ‘Were your parents separated or divorced or did any of your parents die before you reached the age of 18?’
- Mental illness among household members: Measured by responding ‘yes’ to one or both of the following questions: (1) ‘Was anyone in your household ever depressed or mentally ill?’ (2) ‘Did anyone in your household ever attempt to commit suicide?’
- Incarceration of household member: Measured by responding ‘yes’ to the following question: ‘Did anyone in your household ever go to prison?’
Definition of a history of auditory hallucination: A history of hallucination was defined as a ‘yes’ response to the question: ‘Have you ever had or do you have hallucinations (heard things that were not really there)?’
Data analytic approach
Categorical measures are reported as frequencies or percentages and compared with contingency tables (χ2). Continuous measures are reported as means ± standard deviations (SD) and compared by ANOVA methods or Wilcoxon ranksum test (Mann–Whitney U statistic) for non-normally distributed continuous data. Statistical significance required two-tailed p < 0.05. All statistical analyses were conducted using SPSS 22 software.
RESULTS
Clinical characteristics
The study included 51 male patients admitted to the hospital or outpatients. According to the DSM IV, all patients were diagnosed with schizophrenia, subtype paranoid (72.6%), disorganized (15.7%), residual (9.8%) and catatonic (1.9%). All patients were between 18 and 65 years (M = 41.27; SD = 12.61). Patients reported an average of 10.33 years (SD = 3.55) of completed education and the majority of the sample were single (82.4%) and unemployed (88.2%) (Table 1).
|
Table 1: Socio-demographic characteristics of patient sample (N = 51). |
|||
|
|
M (±SD) or % |
Range |
|
|
Mean age |
41,27 (±12,61) |
20-65 |
|
|
Relationship status, n (%) |
|
|
|
|
Single |
82,4% |
|
|
|
Married/living with a partner |
13,7% |
|
|
|
Divorced |
2,0% |
|
|
|
Widowed |
2,0% |
|
|
|
Years of education |
10,33 (±3,55) |
|
|
|
Occupation, n (%) |
|
|
|
|
Employed |
11,8% |
|
|
|
Unemployed |
88,2% |
|
|
Adverse childhood events
The average score of the scale was 4.33 ± 2.17 (mean +/- SD) and the median score was 5 (range 0-9). Of the total sample, 32 individuals (63%) reported 4 or more disruptive events.
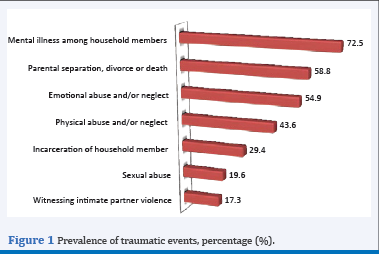
The most frequent subtype found was a mental illness among household members, reported by 37 patients (72.5%), followed in decreasing order by parental separation, divorce or death (30 patients, 58.8%), emotional neglect (28 patients, 54.9%), and physical neglect (22 patients, 43.6%) (Figure 1).
Figure 1 Prevalence of traumatic events, percentage (%).
We also found a significant relationship between patients who suffered multiple adverse events during childhood (ACE > 4) and the presence of auditory hallucinations (p = 0.016) (Table 2).
|
Table 2: Descriptive statistics of the variables studied among the group of patients with 3 or less ACE and the group with 4 or more ACE. |
|||
|
|
0-3 ACE (n = 19 ) |
4 or more ACE (n = 32 ) |
p value |
|
Mean hospitalizations, n (SD)
|
4,24 (3,36) |
3,65 (2,39) |
0,483 |
|
Prevalence of substance use, n (%)
|
7 (36,8) |
18 (56,3) |
0,180 |
|
Prevalence of auditory hallucinations, n (%) . |
13 (68,4) |
30 (93,8) |
0,016 |
In our analysis we found a significant relationship between suffering sexual abuse during childhood and the presence of substance abuse in adulthood (p=0.03) and between the history of physical neglect and the presence of auditory hallucinations (p=0.02) (Table 3).
|
Table 2: Descriptive statistics of the variables studied among the group of patients with 3 or less ACE and the group with 4 or more ACE. |
|||
|
|
0-3 ACE (n = 19 ) |
4 or more ACE (n = 32 ) |
p value |
|
Mean hospitalizations, n (SD)
|
4,24 (3,36) |
3,65 (2,39) |
0,483 |
|
Prevalence of substance use, n (%)
|
7 (36,8) |
18 (56,3) |
0,180 |
|
Prevalence of auditory hallucinations, n (%) . |
13 (68,4) |
30 (93,8) |
0,016 |
DISCUSSION
The majority of the individuals included in the study suffered from some traumatic event during childhood (94%). We found that 63% of the sample scored four or more types of trauma. Our findings are higher than those found in general population [2,34], in subjects with mental disorders in prison [35,36], in patients with a severe mental illness [5], and among schizophrenic spectrum patients [5,6,8-11,20,37].
In contrast to others studies, we found that certain types of adverse childhood events increase the risk of some clinical variables: sexual abuse increases the risk of substance abuse and psychical neglect rises the risk of hallucinations [10,23,30,32,37].
Several studies have linked the history of multiple adverse childhood events with substance abuse, greater psychotic symptoms and also with higher rates of hospitalization among patients with mental disorders [5,11,20]. As in many studies, we also found a significant relationship between the development of auditory hallucinations among patients with a large history of adverse childhood events [9,20,38]. In comparison with other analysis, we observed a greater use of psychoactive substances among people who suffered from 4 or more events, although this difference was not statistically significant in our study [11]. In contrast to other studies, we did not find a greater number of hospitalizations among subjects who suffered multiple adverse events [11,38].
Despite the evidence, the relationship between childhood adversity and schizophrenia is neither simple nor linear. Childhood adversity is neither necessary nor sufficient to cause schizophrenia, and a critical review of the association between childhood trauma and psychosis found only tentative evidence of a positive relationship.
The current study contains limitations that should be considered when interpreting the findings. First, results are based on observational, cross-sectional data with a small simple. Second, the data were obtained retrospectively and the accuracy can be affected by recall bias. However, several studies have demonstrated the reliability of retrospective reports of trauma in patients with psychosis. These studies demonstrated that the information obtained from questionnaires correlates adequately with other sources of information. There is evidence that retrospective evaluation of child abuse tends to be underestimated due to mnesic alterations, denial, or a decision not to disclose such experiences. Individuals reporting abuse retrospectively were those who typically endured the most severe abuse on prospective assessment [39,40], this allows us to conclude that the results obtained could be undervalued [14,41]. Finally, due to the preliminary and exploratory nature of our work, our study lack a control group, and we are therefore unable to assume on whether the patients in our sample experienced higher levels of substance abuse than appropriately matched controls from the same population.
Our growing theoretical understanding of the way in which biological and psychosocial alterations can lead to the development of psychosis in subjects suffering from childhood traumatic events allows us to have a more integrative approach for the evaluation and implementation of psychological, social and biological therapeutic strategies.
Our findings suggest that it would be useful for pediatricians to explore the presence of adverse events in children, in order to detect their presence and to initiate an appropriate treatment at an early age. By the other side, clinicians should routinely inquire about adverse events during childhood in adults patients in order to develop treatment plans when working with patients with schizophrenia or similar diagnoses. In agreement with Varese et al, we consider that psychosocial interventions that have been used for patients affected by trauma events might be consider among the treatment options for patients with schizhophrenia and childhood maltreatment [18].
Table 1: Socio-demographic characteristics of patient sample (N = 51).
| M (±SD) or % | Range | |
| Mean age | 41,27 (±12,61) | 20-65 |
| Relationship status, n (%) | ||
| Single | 82,4% | |
| Married/living with a partner | 13,7% | |
| Divorced | 2,0% | |
| Widowed | 2,0% | |
| Years of education | 10,33 (±3,55) | |
| Occupation, n (%) | ||
| Employed | 11,8% | |
| Unemployed | 88,2% |
Table 2: Descriptive statistics of the variables studied among the group of patients with 3 or less ACE and the group with 4 or more ACE.
| 0-3 ACE (n = 19 ) |
4 or more ACE (n = 32 ) |
p value | |
| Mean hospitalizations, n (SD) | 4,24 (3,36) | 3,65 (2,39) | 0,483 |
| Prevalence of substance use, n (%) | 7 (36,8) | 18 (56,3) | 0,180 |
| Prevalence of auditory hallucinations, n (%). | 13 (68,4) | 30 (93,8) | 0,016 |
Table 3: Type of childhood abuse and clinical variables.
| Prevalence of auditory hallucinations | Mean Hospitalizations | Prevalence of Substance use | ||||
| n (%) | p value | n (SD) | p value | n (%) | p value | |
| Emotional Abuse | 25 (48) | 0,28 | 3,7 (2,4) | 0,75 | 14 (27) | 0,87 |
| Physical abuse | 17 (33) | 0,91 | 3,7 (2,4) | 0,44 | 10 (19,6) | 0,91 |
| Sexual abuse | 8 (16) | 0,67 | 2,8 (1,5) | 0,19 | 8 (16) | 0,03 |
| Emotional neglect | 25 (48) | 0,28 | 4,2 (2,6) | 0,35 | 12 (24) | 0,33 |
| Physical neglect | 23 (43) | 0,02 | 3,7 (2,5) | 0,71 | 13 (25,5) | 0,57 |
| Parental separation, divorce or death | 25 (48) | 0,81 | 4,2 (2,8) | 0,19 | 18 (36) | 0,06 |
| Witnessing intimate partner violence | 8 (16) | 0,67 | 3,4 (2,2) | 0,62 | 5 (10) | 0,66 |
| Mental illness among household members | 32 (62) | 0,48 | 4,2 (3,3) | 0,09 | 18 (36) | 0,93 |