Progressive Aortic Valve Stenosis: Is it all about the Calcium Deposition?
- 1. School of Medicine, Mayo Clinic, USA
- 2. Division of Cardiovascular Disease and Department of Internal Medicine, Mayo Clinic, USA
Abstract
Two patients with bicuspid aortic valve developed progressive dyspnea and severe stenosis during active surveillance. Patient 1 is a 67 year-old male with mild coronary artery disease. Prior to valve replacement, Computed Tomography (CT) demonstrated a heavily calcified valve (4,238 AU) with severely reduced leaflet excursion. Patient 2 is a 40 year-old female with no significant past medical history. CT showed moderately thickened aortic valve leaflets and minimal calcification (54 AU). In conclusion, hemodynamic assessment is a better indicator of severe aortic stenosis than CT calcium quantification, which may be limited in a subset of patients with bicuspid aortic valve.
Citation
Huntley GD, Thaden JJ, Clavel MA, Enriquez-Sarano M, Nkomo VT (2017) Progressive Aortic Valve Stenosis: Is it all about the Calcium Deposition? Clin J Heart Dis 1(1): 1004.
Keywords
• Aortic stenosis
• Bicuspid aortic valve
• Computed tomography
ABBREVIATIONS
BAV: Bicuspid Aortic Valve; AS: Aortic Stenosis; CT: Computed Tomography; AVC: Aortic Valve Calcium
INTRODUCTION
Degenerative calcification of tricuspid aortic valves and bicuspid aortic valves (BAV) is the most common cause of significant aortic stenosis (AS) and increases in prevalence with aging [1]. It is now recognized that aortic valve calcification is an active process similar to atherosclerosis, involving lipoprotein accumulation, cellular infiltration, and extracellular matrix formation that leads to progressive valve calcification and consequential cusp immobility and outflow obstruction [2]. Since valve calcification plays a key role in the development of AS, computed tomography (CT) with aortic valve calcium (AVC) scoring can be utilized to grade the severity of stenosis. CT AVC scoring provides a flow-independent assessment of severity, so it is particularly helpful in patients with discordant gradients, classically with aortic valve area ≤ 1.0?cm2 indicating severe stenosis but a peak velocity <4?m/s and mean gradient <40?mm?Hg consistent with less than severe disease [3]. In this case report, we present two unique patients with BAV stenosis in which CT with AVC scores was utilized in their management.
CASE PRESENTATION
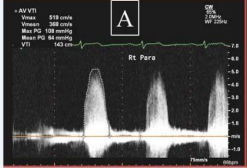
Patient 1 is a 67 year-old Caucasian male with a 21-year diagnosis of BAV stenosis. His history is significant for mild coronary artery disease but otherwise negative. During active surveillance he developed progressive NYHA symptoms. On cardiac exam, he had a late-peaking systolic murmur with a single, diminished S2. Severe stenosis was confirmed by 2D-Doppler echocardiography (Figure 1A, Table 1).
Figure 1: Continuous Wave Doppler assessment for mean systolic gradient. The mean systolic gradient, 64 mm Hg, was obtained in the right parasternal window for Patient 1 (A) while the mean systolic gradient for Patient 2, 47 mm Hg, was obtained from the apical imaging window. Both were consistent with severe outflow obstruction.
Table 1
Table 1: Comparison of Transthoracic Echocardiographic and MDCT with Calcium Results.
|
|
Patient 1 |
Patient 2 |
|
Demographics |
67 year-old male |
40 year-old female |
|
Aortic Valve Area |
0.93 cm2 |
0.98 cm2 |
|
Transaortic Maximum Velocity |
5.19 m/s |
4.60 m/s |
|
Mean Pressure Gradient |
64 mmHg |
47 mmHg |
|
Ejection Fraction |
66% |
72% |
|
Stroke Volume Index |
66 |
43 |
|
CT Calcium Score |
4,238 AU |
54 AU |
|
Excised Valve Weight |
2.03 g |
1.62 g |
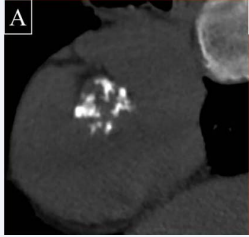
Prior to aortic valve replacement, Multiple Detector CT with AVC quantification was performed to exclude concomitant coronary artery disease (Figure 2A).
Figure 2A: Multiple Detector Computed Tomography for Aortic Valve Calcium Quantification. Despite hemomodynamically severe stenosis in both patients, the valve of Patient 1 (A) appears heavily calcified while the valve of Patient 2
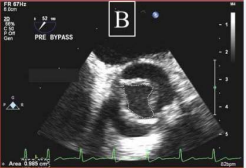
The preoperative transesophageal echocardiogram confirmed a heavily calcified valve with severely reduced leaflet excursion (Figure 3A).
Figure 3A: Transesophageal echocardiography showing bicuspid aortic valve in the short axis.The valve of Patient 1 (A) appears heavily calcified with severely restricted leaflet excursion. By comparison, the valve of Patient 2
Aortic valve replacement was performed using a bioprosthetic (bovine) valve, and the excised valve was weighed (2.03 g). At follow up 4 years postoperatively, he was doing well.
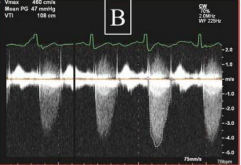
Patient 2 is a 40 year-old Caucasian female with known BAV stenosis. She had no significant past medical history and her BAV was discovered at the time of pregnancy 13 years earlier with asymptomatic moderate stenosis. During active surveillance she developed progressive NYHA symptoms. On cardiac exam, her heart sounds suggested a compliant valve with an opening click and preserved S2.Transthoracic echocardiography revealed severe stenosis (Figure 1B, Table 1),
Figure 1B
Figure 1B: Continuous Wave Doppler assessment for mean systolic gradient. The mean systolic gradient, 64 mm Hg, was obtained in the right parasternal window for Patient 1 (A) while the mean systolic gradient for Patient 2, 47 mm Hg, was obtained from the apical imaging window. Both were consistent with severe outflow obstruction.
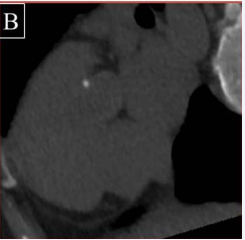
and aortic valve replacement was planned. Preoperative Multiple Detector CT (Figure 2B),
Figure 1B :appears to lack any significant calcium deposition
and transesophageal echocardiography (Figure 3B)
Figure 3B:appears to have minimal calcification and less restriction of leaflet motion. Interestingly, despite the appearance of less significant stenosis, direct planimetry of the valve suggests a severely narrowed orifice with a valve area of 0.99 cm2.
revealed no significant coronary artery disease, moderately thickened aortic valve leaflets, and minimal calcification of the aortic valve. A mechanical 23mm Carbomedics mechanical valve was placed, and the excised valve was weighed (1.62 g). Postoperative examination confirmed a congenitally bicuspid valve with moderate fibrosis and mild calcification. The patient did well postoperatively.
DISCUSSION
We present two cases of patients with BAV, severe stenosis by Doppler echocardiography, and increased valve weight but widely discordant valve calcification. Patient 1 represents the stereotypical case of BAV stenosis: severe calcification of cusps and consequential abnormal hemodynamics by 70 years of age requiring replacement. Patient 2 provides an interesting contradiction: echocardiography-confirmed severe stenosis but minimal calcification at 40 years of age requiring replacement. The majority of the weight of an operatively excised valve with AS was thought to be the result of calcium deposition [4]. However, the striking difference in the valve calcification of these two patients is discordant with the similar excised valve weights (1.62g vs. 2.03g). Normal aortic valve weight is approximately 0.50 +/- 0.13 g, and the increased valve weight in Patient 2 suggests active remodeling of the valve5 . Emerging data suggests that calcification is not the only mechanism for BAV stenosis, and Patient 2 raises many questions about the mechanism of stenosis in younger patients [5,6]. There may be a subset of patients with severe BAV stenosis, particularly young patients, in which the mechanism of stenosis is fundamentally different and fibrosis predominates without appreciable calcification. It remains to be elucidated whether this phenomenon is a function of age, valve morphology, or a composite. Therefore, hemodynamic assessment remains the superior modality for evaluation of aortic stenosis, since CT calcium quantification may have limitations in certain patients [6,7]. We advocate further studies evaluating the diagnostic utility of CT particularly in younger patients.