A Study on the Actual Value of Different Measurement Positions of Medical Infrared Thermometers
- 1. Department of infection prevention and control, People’s Hospital of Kizilesu Kirgiz Autonomous Prefecture, China
- 2. Department of operation management, The First Affiliated Hospital with Nanjing Medical University Nanjing, China
- 3. Department of Pharmacy, The First Affiliated Hospital with Nanjing Medical University Nanjing, China
Abstract
Objective: To study the practical value of medical infrared forehead thermometer (forehead thermometer gun) in body temperature screening and provide reference for accurate screening of fever patients in various institutions.
Methods: For the pre-examination triage patients, the forehead temperature gun was used to select the forehead (forehead method), wrist (wrist method) and neck (neck method) for temperature measurement, and the mercury thermometer was used to measure the axillary temperature (standard method).
Results: A total of 178 fever patients were included and their body temperature was measured at three different surface areas using a frontal thermometer. The results showed that the neck method > forehead method > wrist method and had a statistically significant difference (P < 0.001); Compared with the fever patients measured in the standard method, the neck method had the highest actual screening rate with reaching 91.57%. According to the sunset time, a day is divided into three time periods. There is a statistically significant difference in body temperature between the neck method and the standard method during the pre sunrise time period (22:00-7:00) and post sunrise time period (7:00-15:00) after sunset. However, there is no significant difference in body temperature measured between the two methods during the pre sunset time period (15:00-22:00) after sunrise, and the neck method has the highest actual screening rate of 97.22% during this time period.
Conclusion: The forehead temperature gun measures the body temperature of different parts of fever patients, with the highest accuracy and actual screening rate in the neck. The position of neck should be chosed firstly. During a specific time period of the day, the neck temperature measured by a forehead thermometer can replace the temperature measured by a mercury thermometer.
Keywords
- Medical Infrared Thermometer; Forehead Thermometer; Fever Patients; Body Temperature Screening
Citation
Zhang Q, Zhang B, Dou J, Liu B, Chen C (2025) A Study on the Actual Value of Different Measurement Positions of Medical Infrared Ther- mometers. Clin Res Infect Dis 9(1): 1070.
INTRODUCTION
Fever is one of the main symptoms of many infectious diseases, and measuring body temperature is a commonly used screening method for early warning of infectious diseases, playing a significant role in various outbreaks such as the Severe Acute Respiratory Syndrome (SARS) in 2003, the H1N1 Influenza in 2009, the Ebola Virus Disease (EVD) in 2014, and the Coronavirus Disease 2019 (COVID-19) [1]. For children, rectal temperature measurement is often considered the gold standard; for adults, pulmonary artery catheterization is the reference standard for measuring core body temperature, but it is invasive and requires specialized skills and equipment. Both methods are not suitable for large-scale screening. Traditional alternatives such as oral, axillary, and aural thermometers, though less invasive, require contact with the skin or even body fluids, posing a risk of cross-infection [2-4]. Currently, non- contact facial temperature measurement technology using infrared thermography has become one of the common screening methods, extensively used in hospitals, airports, and other restricted public areas.
However, this method has some issues, especially factors such as environmental temperature, humidity, noise, direct sunlight, sweating, various social and psychological factors, and technical differences in infrared cameras, all of which can affect the reliability and accuracy of the measurement [5]. If a patient with fever is detected, a mercury thermometer is still needed for re-measurement of body temperature, which requires patient cooperation. However, the premise of re-measuring body temperature is the ability to initially screen out patients with fever. At the same time, for some small-scale places, such as schools, pharmacies, supermarkets, and rural health clinics, there are limitations in terms of conditions, space, funding, and maintenance costs, making it impossible to equip with infrared thermography. Therefore, low-cost, non-contact, and easy-to-use medical infrared forehead thermometer (commonly referred to as a forehead thermometer) has been widely used for mass temperature screening. However, in practical work, there is often inconsistency in the choice of measurement sites for forehead thermometers, such as the forehead, wrist, neck, and other different parts.
There are few domestic reports on whether there is a difference in body temperature measured at different sites with a forehead thermometer, especially for patients with fever. This study compares and analyzes accuracy, applicability, and influencing factors of body temperature measured at different body surface sites with a forehead thermometer, explores its actual value in temperature screening, and provides a reference for selection of measurement sites for forehead thermometers in daily work.
DATA AND METHODS
Data Source
This study involved patients who underwent temperature screening at the emergency department and outpatient pre-triaging clinic of a tertiary general hospital from April 1st to April 15th, 2022. Patients with a body temperature exceeding 37.4°C, identified as febrile patients (with the standard for fever determination based on measurements taken by an axillary thermometer) were selected as the subjects of the research. The study was approved by the hospital’s ethics committee, and informed consent was obtained from the patients themselves.
Measuring Instrument
Medical infrared frontal thermometer produced by Hunan Honggao Electronic Technology (Model: HG01); The mercury thermometer is a triangular rod glass thermometer produced by Chongqing Riyue Medical Equipment. Before the experiment, the two kinds of thermometers were calibrated and tested by the metrological department to meet the standard.
Research Method
Under the same conditions, the body temperature of the same subject was measured by four methods at the same time. Armpit temperature was taken as the standard method, and frontal temperature gun was divided into three methods: forehead method, wrist method and neck method. Operators are trained to ensure the accuracy of measurement data.
Concrete method
- Standard method: Before taking a measurement, the mercury thermometer that has been previously disinfected is shaken down to below 35°C. Patients are instructed to dry any sweat from their armpits. Then, the mercury end of the thermometer is placed right in the middle of the armpit, making sure it is in close contact with the skin. The patient is then asked to bend their arm over the chest and hold it tightly to keep the thermometer in place. After keeping the thermometer in this position for 5 minutes, the reading is taken, minimized [6]. Keep a record. Patients with axillary temperature exceeding 37.4? were included in the study.
- Forehead method: The patient should expose the forehead area without any hair obstruction, and dry any sweat. The triage personnel should then hold the infrared forehead thermometer at a distance of 3~5 cm directly in front of the forehead for 1s. Upon hearing a “beep” sound, signaling the completion of the scan, and the temperature reading should be taken. Record the measured value.
- Wrist method: The patient should expose the wrist area without any clothing obstruction. The triage personnel should then position the infrared forehead thermometer 3~5 cm in front of the wrist for 1s. Upon hearing a “beep” sound, signaling the completion of the scan, and the temperature reading should be taken. Record the measured value.
- Neck method: The patient should expose the neck area without any obstruction from hair, clothing, scarves, or other items. The triage personnel should aim the infrared thermometer at the area just above the carotid pulse on the patient’s neck, ensuring it is held perpendicular to the skin. The thermometer should be held at a distance of 3~5 cm for 1s. Upon hearing a “beep” sound, signaling the completion of the scan, and the temperature reading should be taken. Record the measured value.
Research Content
The difference between the temperature measured by the forehead method, the wrist method and the neck method was compared, and the difference between the temperature measured by the three methods and the standard method was compared, and the screening rate of the actual feverpatientswasmeasuredbythethreemethods (screening rate=the number of fever patients actually measured by the forehead temperature gun/the number of fever patients measured by the armpit thermometer). Based on the impact of ambient temperature on individual body surface temperature, the day is divided into three time segments using local sunrise and sunset times and changes in environmental temperature as references (with an average sunrise time of 7:00 AM and solar noon at 3:00 PM): the period from after sunset to before sunrise (22:00- 7:00), the period from sunrise to after solar noon (7:00- 15:00), and the period from after solar noon to before sunset (15:00-22:00). A comparison is made between the differences in body temperature measured by a forehead thermometer and the standard method, as well as the actual fever screening rate among patients.
Statistical Analysis
The database was established using Excel, and the values were analyzed with the statistical software SPSS version 26.0. Quantitative data are expressed as the mean ± standard deviation (x ± s). Data that are not normally distributed are described using the median (interquartile range). For comparing multiple samples, the non- parametric Kruskal-Wallis test is used, and for comparing data between two samples, the Mann-Whitney U test is applied. A difference is considered statistically significant when P < 0.05.
RESULT
Basic Patient Data
Over a continuous period of 15 days, a total of 13,395 patients were admitted for pre-examination and triage, among which 178 patients with a fever, defined as a body temperature exceeding 37.4? were identified. Among them, there were 25 patients over 60 years old (accounting for 14.04%), 31 patients between 18 and 60 years old (accounting for 17.42%), and 122 patients under 18 years old (accounting for 68.54%), with an average age of (19.86 ± 25.60) years old.
Comparison of Body Temperature Measurements at Different Sites Using a Forehead Thermometer
During the study period, a total of 178 patients with fever measured under the armpit were included. The body temperatures measured at the forehead, wrist, and neck using a forehead thermometer showed that the average temperature was in the order of neck method > forehead method > wrist method. The comparison of the temperature differences among the three methods indicated a significant statistical significance, for specific details, please refer to (Table 1).
Table 1: Comparison Results of Body Temperature Measurements at Different Sites Using a Forehead Thermometer.
|
Group |
Mean Value (?) |
Temperature Interquartile Range (?) |
P |
|
Forehead Method |
37.7 |
37.7 (37.3,38.1) |
< 0.001 |
|
Wrist Method |
37.4 |
37.3 (36.9,37.7) |
|
|
Neck Method |
38.4 |
38.3 (37.8,39.0) |
|
Comparison of Body Temperature Measurements Between Forehead Thermometer and Standard Method
Upon comparison, it was found that the body temperatures measured by the forehead and wrist methods were both significantly lower than those measured by the standard method. However, although there was a statistical difference in the body temperature results measured by the neck method compared to the standard method, the values were close to each other, please refer to (Table 2).
Table 2: Comparison Results of Body Temperature Measurements between the Forehead Thermometer Group and the Standard Method.
|
Group |
Forehead Method (?) |
Wrist Method (?) |
Neck Method (?) |
|
Standard Method 38.5 (37.9,39.13) |
37.7 (37.3,38.1) |
37.3 (36.9,37.7) |
38.3 (37.8,39.0) |
|
Z-Score |
-11.24 |
-11.47 |
-2.21 |
|
P |
P < 0.001 |
P < 0.001 |
P = 0.027 |
Actual Screening Rate of Fever Patients by Forehead Thermometer
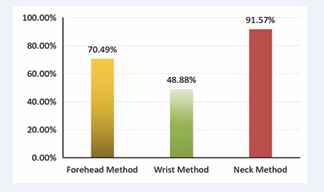
Among the 178 fever patients measured by the standard method, 126 were actually detected by the forehead method, 87 by the wrist method, and 163 by the neck method. The highest actual screening rate was achieved by the neck method, reaching 91.57%, For detailed information, please refer to (Figure 1).
Figure 1: Results of the actual screening rates of fever patients using the three methods of forehead thermometer.
Comparison of Body Temperature Measurements Between Neck Method and Standard Method at Different Time Periods
Comparing the body temperature measurements between the neck method and the standard method across threetime periods, theresults show that thereisa significant statistical difference in body temperature between the two groups during the period after sunrise (7:00-15:00) and the period before sunrise the following day (22:00- 7:00). However, during the period before sunset after sunrise (15:00-22:00), no significant statistical difference was observed in the body temperatures measured by the two groups. For specific details, please refer to (Table 3).
Table 3: Comparison results of body temperature measurements at different time periods.
|
Item |
7:00-15:00 |
15:00-22:00 |
22:00-7:00 |
|
Neck Method |
38.5 (38.2,39.0) (n = 57) |
38.5 (38.0,39.2) (n = 70) |
37.8 (37.4,38.2) (n = 36) |
|
Standard Method |
38.0 (37.8,38.8) (n = 60) |
38.6 (38.2,39.3) (n = 72) |
38.7 (38.2,39.2) (n = 46) |
|
Z-Score |
3.41 |
0.685 |
5.649 |
|
Inspect |
P < 0.001 |
P = 0.493 |
P < 0.001 |
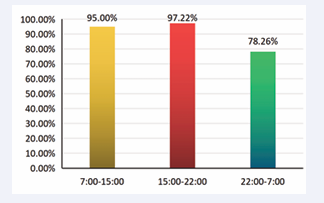
In the three time periods, the standard method detected 60, 72and 46 fever patients respectively, while the neck method identified 57, 70 and 36 actual fever patients respectively. The actual screening rate was highest during the period from after sunrise to before sunset (15:00- 22:00), reaching 97.22%. For specific details, please refer to (Figure 2).
Figure 2: Results of the actual screening rates for fever patients using the neck method at three different time periods.
DISCUSSION
Fever is a temporary pathophysiological state that involves changes in the hypothalamic temperature regulation system and is followed by an increase in body temperature above the normal range. The measurement of body temperature depends on the choice of anatomical region, as there is a significant difference between core body temperature and surface temperature [7]. Another significant source of variability is the change in body temperature that occurs throughout the day, which depends on a person’s activity status and the ambient temperature conditions at the time.
During the past few years of the pandemic, fever screening has been conducted at the entrances of busy traffic areas and high-frequency access locations, such as public transportation hubs, shopping malls, hospitals, and other similar places. Infrared thermography (also known as thermal imaging) and medical infrared forehead thermometers (commonly referred to as forehead thermometers) are the primary types of equipment used for screening, and they have also demonstrated great potential in detecting abnormal body temperatures [8,9]. Their working principle is based on the fact that the human body emits infrared radiation. Like other types of electromagnetic radiation, infrared radiation can be focused onto a detector, which then converts the heat into an electrical signal. This signal is displayed as a graphical contour (thermal scanner) or a digital reading, representing the temperature of the area [10,11]. In the daily process of body temperature screening, most medical institutions typically set up a secondary measurement point. Preliminary patients identified with fever are directed to this point for a re-measurement of body temperature using a mercury thermometer. The mercury thermometer operates on the principle of thermal expansion and contraction of mercury. When measuring axillary temperature, it forms a sealed space under the armpit, isolating factors that could influence the reading from the surrounding environment. This method provides a measurement that is closer to the core body temperature of a person compared to general surface body temperatures, resulting in a more accurate and truthful outcome [12]. However, a crucial aspect is the ability to more accurately identify feverish patients during preliminary screening of body temperature. sensitivity and specificity of screening equipment are important.
In this study, when using a forehead thermometer to measure body temperature at different body surface sites, the neck method yielded a significantly higher average temperature measurement compared to the forehead and wrist methods. Although there were differences in the temperature measurements obtained by the three methods when compared to the standard method, the neck method provided values that were closer to those of the standard method, and it also had a higher actual screening rate of 91.57%. It can be seen that measuring forehead or wrist temperatures often results in missing a portion of patients who actually have a fever. This study shows that wrist monitoring may even miss over 50% of patients with fever, and the forehead method also misses nearly 30%. Therefore, when using a forehead thermometer to measure body temperature, the forehead should not be the first choice, especially not for simply measuring the temperature at the wrist site. This is inconsistent with the research conclusions of Cai si [13] which may be due to the fact that the latter’s study targeted all patients who had their temperature measured, while this study specifically targeted patients with fever, resulting in a difference in the selection of the study population. The focus of this study was on the month of April (spring season), at the outpatient and emergency pre-examination triage entrances. Considering that body surface temperature may be greatly affected by environmental temperature differences, the day was divided into three time periods based on sunrise and sunset times. A comparison of the temperature differences between the neck method and the standard method revealed that during the (7:00-15:00) time period and the (22:00-7:00) time period, there was a statistically significant difference in body temperature measurements between the neck method and the standard method. However, during the (15:00-22:00) time period, there was no statistically significant difference in body temperature measurements between the neck method and the standard method (P > 0.05).
This indicates that environmental temperatures that are too high or too low during the day can affect the accuracy of forehead thermometers. Therefore, during the (15:00-22:00) time period, the precision of measuring neck temperature with a forehead thermometer is similar to that of measuring axillary temperature with a mercury thermometer. However, during the two time periods of 22:00-7:00 and 7:00-15:00, measuring neck temperature with a forehead thermometer may miss some patients with fever, especially during the (22:00-7:00) time period (where nearly 22% of feverish patients were not detected). In the (15:00-22:00) time period, where the neck method has ideal precision, among the 70 fever patients in the age composition of those detected, there were 36 patients aged 1-6 years old (accounting for 51.43%), 10 patients aged 7-18 years old (accounting for 14.29%), and 24 patients older than 18 years old (accounting for 34.29%). This is similar to the overall age composition ratio of fever patients, showing that minors have a relatively high proportion. This indicates that choosing the neck as the measurement site for forehead thermometers in minors has significant advantages, which is partially similar to the conclusions of the overall forehead thermometer study by Fanghua Qin, et al. [14]. Analyzing the possible reasons, the necks of minors, especially children, are in a semi- exposed area and are less affected by the environment. Therefore, using a forehead thermometer to measure neck temperature can yield results that are closer to the actual value. Previous research [15] has found that age is a variable that affects skin measurements, but the role of gender is not very significant. Hence, gender was not included in the analysis of influencing factors in this study. This suggests that the neck method using a forehead thermometer may be particularly suitable for measuring the temperature of minors, as it can provide more accurate reflection of core body temperature, which less influenced by external environmental conditions.
Compared to the traditional mercury thermometer measurement method that requires contact with the human body, forehead thermometers have operational advantages as they can reduce patient discomfort and provide faster readings [11]. Based on the results of this study, when using a forehead thermometer to measure different body surface sites, the neck temperature is more similar to the axillary temperature, and the actual screening rate of neck temperature is higher than that of the forehead and wrist measurements. Therefore, the neck should be the primary choice for measurement sites with a forehead thermometer. In this region, during the specific time period (15:00-22:00), the forehead thermometer can be used to measure neck temperature as an alternative to the mercury thermometer for large-scale screening, which is especially practical for minors. Due to differences in manufacturing processes and detection accuracy among various brands, this study may have certain limitations. However, the results provide important reference for the selection of measurement sites when using forehead thermometers.
REFERENCES
- Zhou Y, Ghassemi P, Chen M, McBride D, Casamento JP, Pfefer TJ, et al. Clinical evaluation of fever-screening thermography: impact of consensus guidelines and facial measurement location. J Biomed Opt. 2020; 25(9): 097002.
- Non-Contact Thermometers for Detecting Fever: A Review of Clinical Effectiveness. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. 2014.
- Aw J. The non-contact handheld cutaneous infra-red thermometer for fever screening during the COVID-19 global emergency. J Hosp Infect. 2020; 104(4): 451.
- Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020; 20(9): e238-e244.
- Micheletti E, El-Nimri NW, Weinreb RN, Liu JHK. Relative Stability of Regional Facial and Ocular Temperature Measurements in Healthy Individuals. Transl Vis Sci Technol. 2022; 11(12): 15.
- Xiaohan Li, Shaomei Shang. Basic Nursing [M] 6th Edn. Beijing: People’s Medical Publishing House. 2017: 242-247.
- Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ, Roberts DJ, Stelfox HT. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015; 163(10): 768-777.
- Schuchat A; CDC COVID-19 Response Team. Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24-April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(18): 551-556.
- Wang Q, Zhou Y, Ghassemi P, McBride D, Casamento JP, Pfefer TJ. Infrared Thermography for Measuring Elevated Body Temperature: Clinical Accuracy, Calibration, and Evaluation. Sensors (Basel). 2021; 22(1): 215.
- Ng EY, Kaw GJ, Chang WM. Analysis of IR thermal imager for mass blind fever screening. Microvasc Res. 2004; 68(2): 104-109.
- Aggarwal N, Garg M, Dwarakanathan V, Gautam N, Kumar SS, Jadon RS, et al. Diagnostic accuracy of non-contact infrared thermometers and thermal scanners: a systematic review and meta-analysis. J Travel Med. 2020; 27(8): taaa193.
- Xian Zhou, Meizhen Zhao, Qunmei Yan. Exploration of the Feasibility of Measuring the Temperature at the Ying xang Point with an Infrared Thermometer. Journal of Nursing Science, 2012; 27(9): 11-12.
- Si Cai, Xinlu Men, Shan Wang. Research on Rapid and Precise Body Temperature Measurement Methods in Dense Populations During the Epidemic of Coronavirus Pneumonia. West China Medical Journal. 2020; 35(4): 385-390.
- Fanghua Tan, Meimei Ma, Meiying You. The Application of Non- contact Infrared Thermometers in Body Temperature Screening at Pediatric Outpatient Departments. Contemporary Nurse (Mid-month Edition). 2018; 6: 118-119.
- Hausfater P, Zhao Y, Defrenne S, Bonnet P, Riou B. Cutaneous infrared thermometry for detecting febrile patients. Emerg Infect Dis. 2008; 14(8): 1255-1258.