Severe Dengue Epidemic in Children without Fatalities
- 1. Pedro Kouri Institute of Tropical Medicine, Cuba
- 2. El Cerro Teaching Pediatric Teaching Hospital, Cuba
Abstract
Dengue is the most important mosquito-borne viral disease. Prompt case detection and appropriate clinical management can reduce the mortality associated to severe dengue. From 19 June to 12 November 2022, 306 children were hospitalized (67% being 5 to 14 years old) with confirmed dengue. Most patients were admitted with Dengue Warning Signs (WS): 192 (62.7 %) and 114 (37.6%), p = 0,000) with Severe Dengue (SD). The patients were managed according to PAHO Guidelines. No fatalities occurred.
Keywords
• Dengue
• Severe Dengue
• Dengue with warning signs
• Dengue shock
CITATION
Martinez E, Consuegra A, Capiro IM, Ramos R, Rodríguez AM, et al. (2023) Severe Dengue Epidemic in Children without Fatalities. Clin Res Infect Dis 7(1): 1061.
INTRODUCTION
Dengue is the most important mosquito-borne viral disease [1]. No vaccine or specific antiviral therapy currently exists to address the growing threat of dengue. Estimates of the global incidence of dengue infections per year have ranged between 50 million and 200 million; however, recent estimates suggest this number is closer to almost 400 million [1]. Here we report the successful application of WHO/PAHO Dengue Classification and recommended management [2,3] during a burst in Havana City, Cuba, during the second semester of 2022. Dengue is a systemic and dynamic infectious disease. The infection may be asymptomatic or present itself with a broad clinical spectrum that includes both severe and non-severe clinical manifestations. The illness begins abruptly and is followed by three phases:
Febrile Phase When
patients typically develop sudden onset of high-grade fever, which may be biphasic, usually lasts 2 to7 days and is often associated to facial flushing, skin erythema, generalized body ache, myalgia, arthralgia, headache, and retro-orbital pain. Patients who deteriorate with defervescence may progress to the critical phase of plasma leakage. Warning Signs should be used to detect the onset of this phase sometimes also with some minor bleedings.
Critical Phase
When the temperature drops some patients may experience an increase in capillary permeability with sudden and uncontrolled leakage of fluids, as well as increased hematocrit levels. This marks the beginning of the critical phase; Shock is the most frequent form of severe dengue. Prolonged shock may be associated to intravascular coagulation, multiple organ failure and other complications.
Recovery Phase
Once patients survive the critical phase, they move on to the recovery phase, during which there is a gradual reabsorption of the leaked fluid from the extravascular to the intravascular compartment. This reabsorption period may last from 48 to 72 hours. In these cases, general well-being improves. Dengue infection can be diagnosed by viral isolation, viral genome detection (through RT-PCR or real-time RT-PCR), and detection of a dengue antigen, as well as the study of serological response in patients with epidemiological and clinical criteria [2,3]. The objective of this study has been to characterize the clinical and laboratory profiles of children and adolescents having dengue with some severity, warning signs included.
METHODS
From 19 June to 12 November 2022, both sex patients aged 1-18 years old were admitted at El Cerro Pediatric Teaching Hospital, Havana City. 306 children were hospitalized, 67% being 5 to 14 years old. Most of patients were admitted with Dengue Warning Signs (WS): 192 (62.7 %) and 114 (37.6%),) with Severe Dengue (SD). Hospitalized patients by age and sex, according to severity at admission is shown in (Table 1). Many patients had received medical attention at Primary Care units during two to five days before coming to the hospital. All of them included in the study were confirmed by positive specific IgM and an important number of cases also having specific PCR that informed Dengue serotype 3 as the most frequent and Dengue serotype 2 in a few cases. Patients with negative results were excluded. All patients were managed according the Pan American Health Organization (PAHO) Tool for the diagnosis and care of patients with suspected arboviral diseases [3]. All adolescents and children aged 10 or more or the mothers of the others had given informed consent and the study was done according to the international ethical rules and ethics committee approvals have been obtained.
|
Age Groups (years) |
Dengue with Warning Signs n (%) |
Severe Dengue n (%) |
Total |
||||||
|
Sex |
Subtotal |
Sex |
Subtotal |
Sex |
Total |
||||
|
Females |
Males |
Females |
Males |
Females |
Males |
||||
|
1 a 4 |
12 (60.0) |
8 (34.8) |
20 (46.5) |
8 (40.0) |
15 (65.2) |
23 (53.5) |
20 (46.5) |
23 (53.5) |
43 (14.1) |
|
5 a 9 |
33 (67.3) |
41 (64.1) |
74 (65.5) |
16 (32.7) |
23 (35.9) |
39 (34.5) |
49 (43.4) |
64 (56.6) |
113 (36.9) |
|
10 a 14 |
33 (67.3) |
27 (62.8) |
60 (65.2) |
16 (32.7) |
16 (37.2) |
32 (34.8) |
49 (53.3) |
43 (46.7) |
92 (30.1) |
|
15 a 18 |
25 (65.8) |
13 (65.0) |
38 (65.5) |
13 (34.2) |
7 (35.0) |
20 (34.5) |
38 (65.5) |
20 (34.5) |
58 (19.0) |
|
Total |
103 (66.0) |
89 (59.3) |
192 (62.7) |
53 (34.0) |
61 (40.7) |
114 (37.3) |
156 (51.0) |
150 (49.0) |
306 (100) |
RESULTS
In patients 1-4 years old not a meaningful difference was found when Dengue with WS and SD were compared (p = 0.6662), neither nor when comparison was made according to sex: females p = 0.3428; males p = 0.0768). From 5 years on, Dengue with WS predominate upon cases with SD (p < 0.05) in all cases and in females of all groups, not in males.
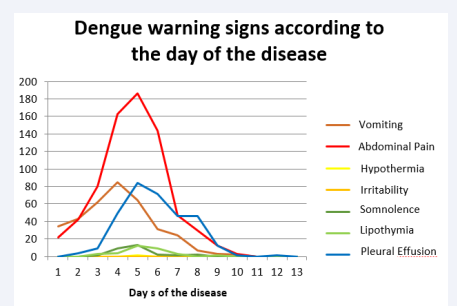
Table 1 Hospitalized patients by age and sex, according to severity at admission. Cerro Pediatric Teaching Hospital, Havana City, June-November/2022. Fever, headache and retroocular pain were frequent symptoms during the first days of the disease (0-4 days), some patients also having petechiae or ecchymosis, about 30%. The most frequent WS of the disease were abdominal pain and vomiting that appeared usually from third to 6th day, and preceded pleural effusion and/or ascites. Irritability, somnolence and lipothymia were also identified (Figure 1).
Figure 1: Source: Clinical documents.
Abdominal pain was the most frequent WS in adolescents (patients 15-18 years old), while vomiting and irritability have predominated in the younger patients, sometimes associated to diarrhea. Not another relevant comorbidity but the antecedent of bronchial asthma in 20% of cases.
All SD cases have had signs of hypovolemic shock. By sex and age group, the frequency of SD was similar (p > 0.05). Most SD cases were admitted to the Pediatric Intensive Care Unit. Shock appeared on 6th day (3th to 7th day), more often at defervescence. Bleedings were not so frequent (5% of patients). No hemoptysis and no lung nor gut hemorrhages occurred, but genital bleeding was present in 42/156 of girls. Respiratory distress was diagnosed in 30, 4% of younger children (less than 5 years old) with SD. Two children belonging to this age group had severe hepatopathy, showing elevated liver enzymes (> 1000 u). Serology was the most frequent diagnostic tool: IgM on 6th day to all cases and IgG to a group of them, ten to fourteen days later. The identification of the infecting virus was done by molecular diagnosis (PCR/TR) with dengue virus 3 predominating and some cases of dengue 2 at the end of the period. Leucopenia was more frequent during 4th and 5th days of the disease. Trombocitopenia was identified from the 2nd day on; the number of platelets recovered in the 10th day. Hemoconcentration of different degrees was evident and high aspartate aminotransferase values (4443 vs. 1061 U/L other enzymes; P = 0.002), Pleural effusion (5th to 9th day), thickened wall of the gallbladder (4th to 8th day), ascites (4th to 10th day), and less frequent fluid in pericardium (5th day and later) were detected by ultrasound and/or radiology.
The patients were managed according to PAHO Guidelines [2,3]. All of them received fluid replacement with glucosaline solutions. Colloid solutions were given when it was strictly necessary, being albumin and fresh plasma the most utilized. Platelets transfusion was not indicated except when hemorrhages were concomitant. Packed red cells were given when hemoglobin was low enough. No fatalities occurred.
DISCUSSION
Our data demonstrate the usefulness of the Classification of Dengue of 2009 in Dengue (with or without Warning Signs) and Severe Dengue. All our 306 patients could be classified in one of those categories. The former classification considered as severe dengue the so-called Dengue Hemorrhagic Fever, which in practice could not include all severe patients and it was too dependent on laboratory [4]. That term is not recommended now. In America, Cuba was the first country with an epidemic of such severe form of dengue. At the beginning, hemorrhages were responsible of the majority of patients who died but later the physicians in charge were aware that prolonged shock with associated hypoxemia and other complications were the cause of bleedings. It was also identified a regularity: some signs preceded shock, which were named warning signs [5].
In our study, abdominal pain and vomiting were the more frequents WS. These symptoms usually precede to pleural effusion or ascites. It suggests that the liquid from extravasation was accumulated before in other part of the body, for example in retroperitoneal areas. It could be the cause or contribute to the abdominal pain. Irritability, somnolence and lipothymia are manifestations of hypoxemia associated to brain hypoperfusion that can occur even before signs of shock are evident. Having had 114 patients with SD without fatalities supports the effectiveness of PAHO recommendations. Anyway, very important is also that 192 children and adolescents with WS could be successfully managed and severity could be probably prevented. Early diagnosis of Shock is determinant for the successful management of dengue severe patients [6]. Being blood hypotension a late sign of shock, other clinical signs should be identified before, such as the weak pulse or the narrowing of the blood pressure. Administration of fluids during that first stage of shock may prevent complications as bleedings. It could be the explanation for the relative infrequent hemorrhages in our patients. Only a small number of these cases had important associated thrombocytopenia. It explains that platelet transfusions were only a few.
Dengue is a viral infection transmitted to humans through the bite of infected mosquitoes. The primary vectors that transmit the disease are Aedes aegypti mosquitoes and, to a lesser extent, Ae. albopictus. Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. The virus responsible for causing the disease is called Dengue Virus (DENV). There are four DENV serotypes and it is possible to be infected four times. To have heterotypic antibodies is a risk factor for severe dengue. The global incidence of dengue has grown dramatically with about half of the world’s population now at risk [7]. Although an estimated 100-400 million infections occur each year, over 90% are generally mild and asymptomatic. Severe dengue is a leading cause of serious illness and death in some Asian and Latin American countries. There is no specific treatment for dengue/severe dengue [8]. An effective vaccine is urgently needed [9].
While most DENV infections are asymptomatic or produce only mild illness, occasionally this develops into a potentially lethal complication called severe dengue, mostly hypovolemic shock with or without respiratory distress [10]. In Viet Nam, signs of vascular leakage and shock were more frequent and more severe in children than adults, while bleeding manifestations and organ involvement were more common in adults. Additionally, adults experienced significantly more severe thrombocytopenia [11]. Fluid extravasation due to cytokines and some viral factors acting on endothelium can determine hypovolemic shock that is the cause in 90% of severe cases [12]. Warning Signs (WS) announce the imminence of Dengue shock [13]. No inflammation exist in dengue as it does in Covid-19, which has to be differentiated in areas where both diseases coexist. Prolonged shock can induce disseminated intravascular coagulation or multiple organ failure. Other forms of severity are hemorrhages, mainly digestive or respiratory and particular severe organ damage, like hepatitis, myocarditis and encephalitis [14].
The uncertainty of dengue’s progression from infection to its severe form represents a major health care challenge, especially in children. Clinical identification of impending clinical manifestations of Severe Dengue (SD), along with proper and immediate management, is crucial. After multivariate analysis, Juliansen et al has assessed the ability of warning signs to predict SD infection in pediatric patients [15]. Abdominal pain, mucosal bleeding, lethargy, hepatomegaly and increased hematocrit concurrent with a rapid decrease in platelets were associated with SD infection, with a high quality of discrimination. Some studies have found that adults experienced significantly more severe thrombocytopenia than children did [11]. Criteria for platelet transfusion are diverse but most researchers do not recommend it, only if hemorrhages are concomitant.
Severe dengue is a leading cause of serious illness and death in many countries [16]. Anyway, death from dengue is generally preventable if either hypovolemic shock is prevented or treated timely using intravenously administered crystalloid preparations at the time of detecting alarming signs that indicate the onset of clinical deterioration of the patient [17]. Dengue prevention and control depends on effective vector control measures. Sustained community involvement can improve vector control efforts substantially [18]. The main limitation of this study is that some patients with Dengue Warning Signs and Severe Dengue were admitted in other Pediatric Hospitals in the City, being our results not necessarily the only ones. However, our Hospital was the one that received the biggest number of patients from all parts of the City and other neighbor cities close to Havana and most patients with some degree of severity were sent to ours, as it was established. Other limitation to be declared is that all patients were not admitted to the Intensive Care Unit of the hospital but in other Wards having specialized personnel. Anyway, all of them were diagnosed and managed according to the PAHO Guidelines because all doctors and other medical professionals had participated in teaching sessions organized by the Direction of the Hospital before and at the beginning of the epidemic and the management of all children and adolescents with dengue was daily controlled.
AUTHORS CONTRIBUTIONS
EM, AC and MGG: design and coordination of the study. EM also wrote the initial draft. RR and IMC: acquisition and analysis of local data. AM performed statistical analysis and interpretation of merged data. All authors were involved in the drafting of the final manuscript, and all have read and approved it.
REFERENCES
6. Guzmán MG, Perez AB, Martinez E, Fuentes O. Dengue, in Encyclopedia of Public Health, Elsevier. 2016.
10. Khanam A, Gutiérrez-Barbosa H, Lyke KE, Chua JV. Immune-Mediated Pathogenesis in Dengue Virus Infection. Viruses. 2022; 14(11): 2575. doi: 10.3390/v14112575. PMID: 36423184; PMCID: PMC9699586.