Early Initiation of Renal Replacement Therapy in Burns Patients with Acute Kidney Injury
- 1. Department of Plastic, Singapore General Hospital, Singapore
- 2. Department of Renal Medicine, Singapore General Hospital, Singapore
Abstract
Acute Kidney Injury (AKI) can be a serious complication in severely burned patients, it portends a poor prognosis and we hypothesize that initiating Renal Replacement Therapy (RRT) early leads to improved survival outcomes. In our retrospective observational cohort of 27 patients who developed AKI requiring RRT, the average patient age was 45.4 years, 89% were men, 15% were diabetic and the average TBSA burned was 54.8%. 67% of patients were exposed to nephrotoxic antibiotics prior to the development of AKI. 89% of patients had urine output of >0.5 ml/kg/ hour at RRT initiation and average fluid resuscitation volume was 2.7 ml/kg/TBSA. The mean time from admission to dialysis was 6.4 days. Mean urea and creatinine levels at RRT initiation were 17.5 mmol/L and 275.8 umol/L, respectively. 52% patients had RRT initiated at KDIGO AKI Stage 1, 22% patients at KDIGO AKI Stage 2 and 26% patients at KDIGO AKI Stage 3. 74% of patients received Continuous Renal Replacement Therapy (CRRT), 18% received Sustained Low-Efficiency Dialysis (SLED) and the remaining 8% received intermittent hemodialysis. CRRT was instituted at a dose of 30 ml/kg/hour, with an aim to achieve a target dose of at least 25 mL/ kg/hour. The mortality rate in our cohort of patients was 37% and 2 patients were discharged on long term dialysis.
Keywords
Burns, Acute kidney injury, Renal replacement therapy
Citation
Cheah AKW , Chong SJ , Kaushik M , Tan HK , Tan BK (2016) Early Initiation of Renal Replacement Therapy in Burns Patients with Acute Kidney Injury. JSM Burns Trauma 1(1): 1001
ABBREVIATIONS
AKI: Acute Kidney Injury; RRT: Renal Replacement Therapy
INTRODUCTION
Acute Kidney Injury (AKI), a serious complication of burns, develops in approximately a quarter of patients with burns [1] and portends a poor prognosis. Despite appropriate resuscitation and supportive management, 1-2% patients require renal replacement therapy (RRT) and have high mortality rates of 73-100% [1]. Burns patients are hyper-catabolic, have “leaky capillaries” and have high obligatory fluid requirements. Traditional indications for RRT such as refractory fluid overload, severe metabolic acidosis, hyperkalemia and overt uremia are not the most appropriate in burns patients
We hypothesize that initiating RRT early leads to improved outcome and survival. We believe that the benefits of early initiation of RRT allow superior fluid management, thus reducing tissue edema, controlling exudate and decreasing the risk of complications such as Acute Respiratory Distress Syndrome (ARDS) and abdominal compartment syndrome.
The early restoration of electrolyte imbalances and the clearance of metabolites, uremic toxins and inflammatory cytokines also play an important role in the recovery of patients with severe burns
MATERIALS AND METHODS
In our study we conducted a retrospective systematic analysis of all burns patients who developed AKI requiring RRT, from January 2011 to February 2016. A total of 27 patients were identified. Data collected included patients’ age, sex, total body surface area (TBSA) burns sustained, history of diabetes, history of hypertension, history of nephrotoxic antibiotics, total volume of fluid resuscitation per TBSA and urine output pre-dialysis. We have also included measurements of serum creatinine levels at both baseline and post-RRT for patients who survived.
Our indications for dialysis include any one of the following:
• Rise in creatinine > 1.5x baseline,
• Urine output < 0.5ml/kg/hr for at least 2 consecutive hours with refractory response to fluid challenges,
• Rhabdomyolysis
RESULTS
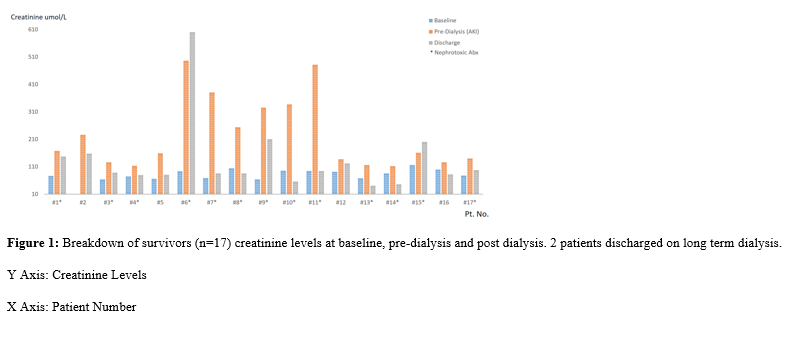
A total of 27 burns patients developed AKI requiring RRT over the study period. The mean patient age was 45.4 years (18-73), 89% were men, 15% were diabetic, 11% were hypertensive and the mean TBSA burned was 54.8%. 67% of patients were exposed to nephrotoxic antibiotics such as Vancomycin and Polymyxin B prior to the development of AKI. Average fluid resuscitation on admission was 2.7ml/kg/TBSA. The mean time from admission to dialysis was 6.4 days and at the point of RRT initiation, 89% of patients had urine output of >0.5ml/kg/hour. Mean urea and creatinine at RRT initiation were 17.5 mmol/L and 275.8 umol/L, respectively. Drawing reference to Kidney Disease: Improving Global Outcomes (KDIGO) guidelines [2], 52% patients had RRT initiated at KDIGO AKI Stage 1, 22% patients at KDIGO AKI Stage 2 and 26% patients at KDIGO AKI Stage 3. 74% (n=20) of patients received Continuous Renal Replacement Therapy (CRRT), 18% (n=5) received Sustained Low-Efficiency Dialysis (SLED) and the remaining 8% (n=2) received intermittent hemodialysis. CRRT was instituted at a dose of 30 ml/kg/hour, with an aim to achieve a target dose of at least 25 mL/kg/hour, as recommended by the KDIGO guidelines. The mean duration of RRT was 18.4 days. The mortality rate in our study was 37% and 2 patients were discharged on long term dialysis (Figure 1)
Figure 1: Breakdown of survivors (n=17) creatinine levels at baseline, pre-dialysis and post dialysis. 2 patients discharged on long term dialysis.
Y Axis: Creatinine Levels
X Axis: Patient Number
DISCUSSION
Our cohort of patients with AKI requiring RRT had lower mortality rates than previously reported studies [3-6]. The mean urea and creatinine at RRT initiation in our cohort was lower than mean urea and creatinine reported by Tremblay et al., [5] 35.1 ± 8.4 mmol/L and 292 ± 72 umol/L, respectively and by Sun et al [6]. Blood Urea Nitrogen 87-147 mmol/L and creatinine 336-552 umol/L. In another study, by Chung et al. [3], the authors reported a mean urea of 16.4 ± 8.5 mmol/L and mean creatinine of 256 ± 177 umol/L, at RRT initiation. They also reported a 28- day mortality of 38% in their RRT cohort. The findings from the above studies may support the hypothesis that early initiation of RRT in burns AKI is associated with favorable outcomes.
In a recent study, the ELAIN trial [7] by Zarbock et al., concluded that in critically ill patients with AKI, early initiation of RRT compared to delayed initiation resulted in reduced mortality over the first 90 days. On the contrary, the Artificial Kidney Initiation in Kidney Injury (AKIKI) study [8] found no significant difference with regard to mortality between early and late initiation of RRT. These studies involved non-burns critically ill patients. It is important to realize that traditional guidelines and indications for RRT in critically ill patients may not be entirely appropriate in burns patients. We believe that there has been a paradigm shift in the management of both AKI and the resulting systemic inflammatory response in extensive burns.
We have observed that fluid resuscitation alone is not sufficient in the management of early AKI in extensive burns; this is evident in our study. In our cohort, 89% patients had urine outputs of >0.5 ml/kg/hr at the time of initiation of RRT. This highlights the fact that etiology of AKI in burns injury is multi-factorial and not strictly limited to hypovolemia. Indeed, other mechanisms in the pathophysiology of AKI in burns injury including cardiac dysfunction, release of inflammatory mediators and denatured proteins, sepsis and nephrotoxic drugs have been implicated [9]
More recently, intra-abdominal hypertension and abdominal compartment syndrome, secondary to excessive fluid resuscitation, has been postulated to have a role in the development of AKI [10]. The traditional Parkland’s Formula (4ml x weight (kg) x TBSA) often causes over resuscitation, which may predispose patients to ARDS and abdominal compartment syndrome. In recent times we have shifted our management away from the traditional Parkland’s Formula in favor of a more conservative approach. We begin initial resuscitation at half of Parkland’s Formula (2ml x weight (kg) x TBSA) and titrate according to urine output. If urine output drops below 0.5ml/ kg/hr we also add in boluses of Albumin into the fluid regime. Severely burned patients, and especially those with concomitant AKI, are known to be hyper-catabolic. This results in excessive generation of toxic metabolic products, which the diseased kidneys are unable to clear. This consequently, leads to their accumulation in blood and exposes patients to their ill effects. RRT is beneficial to burns patients by the removal of uremic toxins, which are well known to have negative effects on wound healing [11]. The negative effects of uremia on fibroblast proliferation and collagen production in wounds have been identified as early as 1960 [12-14]. RRT also aids in the clearance of inflammatory cytokines such as TNF, IL-1 beta, IL-6 and IL-8 [15]. Many of these cytokines are potent vasoconstrictors [16] which can cause peripheral shut down and organ ischemia.
It is well established that severely burned patients have “leaky capillaries” [17] and require aggressive fluid resuscitation. These characteristics render these patients susceptible to fluid overload and organ edema, which manifests as organ dysfunction. The ability to fine tune fluid balance by regulating fluid removal directly from the RRT circuit permits superior fluid management. For example, extracting excess fluid directly from the RRT circuit reduces the dependence on diuretics. Diuretic related complications such as hypotension and hypokalemia secondary to Furosemide usage can hence be avoided. It is important to control edema because excess fluid in tissues provides an obstacle to angiogenesis deprives blood supply and increases the potential for ischemia. We have observed that with vigilant fluid management, interstitial edema is reduced and wound healing improves. RRT also allows rapid correction of metabolic acidosis, hyper-kalemia and rhabdomyolysis.
We recognize that RRT is not without its drawbacks. Adequate intravenous access can be complex in a patient with severe burns and the large caliber central lines required in RRT are also prone to infections causing line sepsis. In addition to the above, close attention has to be paid to antibiotic doses as RRT clears antibiotics from the blood stream. We have in some cases, required 4 times the usual dosage of antibiotics because of RRT. We recommend close monitoring of antibiotic levels and appropriate dosage adjustments by the Microbiologists. It is also vital to have a warmed circuit to prevent hypothermia. In our center, we use regional citrate anticoagulation for RRT, in which the anticoagulation is restricted to the extracorporeal circuit, where citrate acts by ionized calcium [18].
Limitations to our study include our small study population and the absence of a control group to draw a direct comparison to. Our single center study is also retrospective, which brings about their associated disadvantages. CRRT was prescribed at a dose as recommended by the KDIGO guidelines, but the actual delivered dose of CRRT was not recorded.
The early detection of AKI and subsequent early initiation of RRT has been important in the favorable outcomes in the management of extensive burns within our center. We have found RRT to be safe, effective and hemodynamically well tolerated. As such, within our center, the institution of RRT at relatively low thresholds has become a recognized modality of treatment; this is facilitated by a dedicated Renal Physician along with a team of well trained nurses.
CONCLUSION
The early detection of AKI and subsequent early initiation of RRT has shown promising early outcomes within our center. Acknowledging the small study population and recognizing our limitations, when compared to other similar studies [3-6], we had a faster time to dialysis and a lower mortality rate. Through experience, we have found RRT to be safe and effective. As a result, the institution of RRT at lower AKI defining thresholds has become an important tool in the management of AKI in burns patients within our center. The recent set up of a centralized burns database will facilitate further prospective studies in the coming years; ideally this would be one that is multi-centered. Further prospects of development within the field of Renal Replacement Therapy such as the addition of antibiotic impregnated filters into the circuit may also prove beneficial to critically ill patients with severe burns. We aim to eventually identify a criterion to help guide the early initiation of RRT in burns patients.