Applicability of the Streptozotocin-Induced Diabetes Model in Rats for the Detection of Lithium Salts Cytoprotective Effects
- 1. Research Zakusov Institute of Pharmacology, Russia
Abstract
Based on importance of kinase-3β glycogen synthase (GSK-3β) and ambiguity of data concerning the action of GSK-3β inhibitors on the development of diabetes, it seems reasonable to continue the study of this issue. Considering the fact, that the decrease of β-cells amount determines the dynamics of the diabetes development and that streptozotocin (STZ) model reproduces the loss of β-cells, the goal of this work was to evaluate the possible cytoprotective effect of two lithium salts (chloride and carbonate) and to study their action on the functional manifestations of diabetes (hyperglycemia, polydipsia, weight loss) on the STZ model of diabetes in experiments on rats. STZ (single dose of 40mg/kg i.p.) was shown to increase the glucose blood level up to 27mmol/l, cause body weight decrease, polydipsia, MDA blood level increment and the loss of pancreatic β-cells detected by immunohistochemical analysis. Lithium chloride and lithium carbonate administrated for 28 days after STZ injection in doses of 10mg/kg and 8,9mg/kg correspondingly diminished the blood glucose level up to 12mmol/l to the end of experiment. Both lithium salts attenuated the body weight decrease, polydipsia and polyphagia, MDA level augmentation caused by STZ. The immunohistochemical examination shown that STZ diminished the amount of insulin-containing β-cells approximately 4 times, while lithium salts therapy results in two-fold increase of their amount comparing to untreated STZ group. The degree of pancreatic β-cells protection correlates with the level of anti-hyperglycemic activity.
Keywords
• Diabetes
• GSK-3β
• Streptozotocin
• Lithium salts
• Cytoprotection
CITATION
Ostrovskaya R, Ivanov S, Zolotov N, Durnev A (2017) Applicability of the Streptozotocin-Induced Diabetes Model in Rats for the Detection of Lithium Salts Cytoprotective Effects. JSM Diabetol Manag 2(1): 1003
ABBREVIATIONS
GSK-3β: Kinase-3β Glycogen Synthase; ATP: Adenosine Thiophosphate; STZ: Streptozotocin; GLP: Good Laboratory Practice; MDA: Malondialdehyde; NGF: Nerve Growth Factor; BDNF: Brain-Derived Neurotrophic Factor; PBS: PhosphateBuffered Saline; DAB: Diaminobenzidine; pro ngf: pro- Nerve Growth Factor; pro bdnf: pro-Brain-Derived Neurotrophic Factor
INTRODUCTION
The worldwide prevalence of diabetes among people aged 18 years and older has doubled from 4.7% (1980) to 8.5% of the population (2014). In 2010 diabetes affected about 285 million adult people globally, whereas by 2030 the number is forecasted to increase up to 439 million [1]. Diabetes-attributable health expenditures will rise from 612 to 1099 billion dollars USA [2]. Diabetes prevention and its effective treatment should be placed among the most urgent public health problems of modern society. One of the ways for searching drugs with antidiabetic activity may be based on the study of substances inhibiting the activity of kinase-3β glycogen synthase (GSK-3β). GSK-3β is an intracellular serine-threonine kinase synthesized in all tissues of the body and located in the cytoplasm, nucleus and mitochondria. From the point of view of translational medicine the fact of its presence in neurons and pancreatic β-cells deserves a special attention because GSK-3β hyperactivity plays an important role in the pathogenesis of neurodegenerative diseases and diabetes. One of the main functions of this enzyme is the regulation of glycogen synthesis: active GSK-3β inhibits glycogen synthase by phosphorylation and reduces the glycogen level. GSK-3β is a negative regulator of cell proliferation, including that in pancreatic β-cells. The inhibition of this enzyme’s activity was shown repeatedly to restore the rate of glycogen’s synthesis and increase the sensitivity to insulin [3,4]. One of the most extensively studied inhibitors of GSK-3β is lithium that inhibits this enzyme due to competition with magnesium and the non competitive inhibition of ATP-dependent reactions with an inhibition coefficient Ki of 2mmol/l [5].
The existing data on lithium salts effects on the course of diabetes are quite contradictory. There is definite information about the antidiabetic activity of lithium salts [3,6]. This seems contrary to the data for lithium’s ability to inhibit the insulin biosynthesis from its precursor in experiments on isolated islets of Langerhans and thus to exert the diabetogenic effect [7]. Jacobs et al., [8] reported that along with a pro-apoptotic effect GSK-3β in certain conditions can demonstrate an anti-apoptotic effect; it follows that the effect of this enzyme inhibitors’ on the function of pancreatic β- cells is not always predictable. For this reason, it is important to study the effect of lithium salts in vivo using the streptozotocin-induced (STZ) model of diabetes, known to reproduce the main pathogenic mechanisms of this disease [9]. Considering the fact that the decrease of β-cells number and the progressive loss of their function determines the dynamics of diabetes development [10], and that STZ model reproduces the loss of β-cells, the goal of this study was to evaluate the possible cytoprotective action of two lithium salts (chloride and carbonate) and assess their effect on the functional manifestations of diabetes (hyperglycemia, polydipsia, weight loss) on the STZ model of diabetes in experiments on rats.
MATERIALS AND METHODS
AnimalS
All animals’ procedures had pre-approved by the Commission on Biomedical Ethics of the Research Zakusov Institute of Pharmacology, and were in accordance with Good Laboratory Practice (GLP) and the guidelines of the European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes (Strasbourg, 1986). The study was performed on male Wistar rats weighting upon arrival 300-320g obtained from “Stolbovaya” (the nursery of laboratory animals of “Scientific Centre of Medicobiological Technologies of Federal Medicobiological Agency”). The animals were housed under controlled temperature (22-26°C) and artificial light regimen (12h light/dark cycles), with free access to rodent chow and water except of food deprivation 12h prior to STZ administration. The rats were group-housed (10 animals per cage) in ventilated cages.
Substances
STZ (Sigma, USA) dissolved in cold citrate buffer (pH = 4.5) was used as a diabetogenic substance. Lithium chlorides were purchased from the Sigma (USA), lithium carbonate - from Pharmstandard (Russia).
Design of experiments
The diabetes was modeled by a single intraperitoneal (i.p.) injection of STZ (40mg/kg) [11]. This dose was chosen taken into account our previous data that it provokes a two-fold decrease in insulin blood level and the preservation of about 30% of viable β-cells in the pancreas [12]. 72h after STZ injection, blood glucose level was measured. Only animals with the developed diabetes (blood glucose levels of 15-18mmol/L) were included in the experiment (n = 40). Lithium chloride was administrated in the dose of 10mg/kg, shown to be by Kanzariya N.R. et al., (2011) effective in STZ model of diabetes [13]. Lithium carbonate was administrated in the dose of 8.9mg/kg equimolar to lithium chloride 10mg/kg. Both these doses are much lower than those usually used in experiments dealing with antimanic and neuroprotective lithium’ effects [14] and therefore avoided of toxic effects.
The animals were randomly divided into 4 groups.
1) The passive control group – administrated i.p. with cold citrate buffer on the 1-st day of the experiment and distilled water (10ml/kg) daily for consecutive 28 days;
2) The active control group – administrated i.p. with a single STZ and i.p injections of distilled water daily for a consecutive 28 days;
3) The experimental group 3 – administrated i.p. with STZ and consecutive daily injections of lithium chloride (10mg/kg) for 28 days;
4) The experimental group 4 – administrated i.p. with a single STZ injection and consecutive daily injections of lithium carbonate at a dose 8.9mg/kg (equimolar to lithium chloride 10mg/kg) for 28 days.
The weighting of experimental animals was performed before STZ injection and on days 1, 7, 14, 21, 28 of the vehicle or drugs administration. Food and water consumption was recorded throughout the whole period of the experiment. Two hours following the vehicle or the drug administration, blood samples were obtained from the lateral tail vein on days 1, 7, 14, 21, 28. Blood glucose measurements were performed using the One Touch Ultra® (USA) glucometer. On day 29, the animals were sacrificed by decapitation. 1ml of arterial blood was taken for biochemical analysis. Pancreases were dissected out for further histochemical estimation.
Biochemical analysis.
The blood was collected in BD Vacutainer tubes with EDTA, centrifuged and stored at temp -20°C to perform malondialdehyde (MDA) measurement. 50µL of blood plasma was added to 20µL 0.495 M of Mohr’s salt and incubated 30min at 37?C. After adding 1030µL of 0.9% 2-thiobarbituric acid in 50% acetic acid the mixture was incubated at 80°C for 60 min. The samples were left at the room temperature. The absorbance was measured at 532nm using DU-50 spectrophotometer (Beckman-Coulter). MDA content was determined using the extinction coefficient of MDA (ε = 155μM-1cm-1).
Histopathological study
In order to perform the immunohistochemical analysis of the pancreatic islets, the pancreatic samples taken from animals of all groups were fixed in 10% neutral buffered formalin (pH 7.4) (Sigma, USA), dehydrated in alcohol and xylene and embedded in paraffin blocks. 5µm thick microtome sections were made using Jung microtome RM2035 (Germany). Immunohistochemical studies were performed using primary (anti-insulin GP 1:500, Abcam, UK) and secondary (anti-insulin GP 1:500, Abcam, UK) peroxidase-labelled monoclonal antibodies in accordance with the producer’s protocol. PBS (Sigma, USA) was applied for washing and dilution of antibodies. The detection was performed with the DAB (Vector Labs, USA). The accuracy of results was achieved by using negative and positive antigen controls as well as negative antibody controls. Morphometric examination was performed using Aristoplan microscope (Leitz, Germany) at 800× and 1600× magnification, equipped with DCM-800 digital camera (Micromed, Russia), personal computer and ScopePhoto image software. The general amount of pancreatic islets, the surface area of pancreatic islets in absolute number, and as a ratio of pancreatic islets surface area to the total surface area of the micro slide was measured.
Statistical analysis
Statistical analyses of data were carried out with the use of Excel 2007 (MS Office) and Biostat (2009). The results were presented as means ± S.E.M. One-way ANOVA was used to compare the data of MDA level and the total square area of β-cells in islets; repeated measures analysis of variance ANOVA was used for the glucose blood level and body weight. The data was considered significant if p<0.05. To establish the relationship between the glucose level and pancreatic islets surface area, the Spearman correlation coefficient was calculated.
The relative antihyperglycemic activity index (IAg ) was proposed to characterize the dynamics of drugs’ effects:
RESULTS
Effect of lithium salts on blood glucose level and weight dynamics
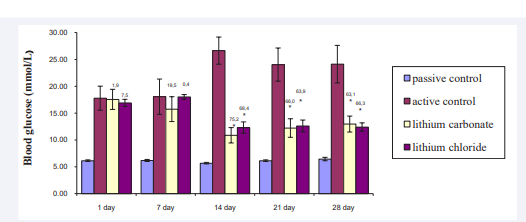
The results of blood glucose basal levels measurement and weight dynamics are presented on Figure 1
Figure 1 The influence of the studied drugs on the blood glucose basal levels in Wistar rats Values are given as mean ± SEM for groups * - the significance between experimental and active control groups, ?<0.05 # - the significance between experimental 1 and 2 groups, ?<0.05 F (12, 120) = 4.2180, p = 0.00002 Figures above bars are values of the index of relative antihyperglycemic activity
and 2 respectively. Blood glucose level in rats with untreated diabetes on day 7 after STZ administration significantly exceeded that in healthy animals; on the consecutive days 14, 21, 28 in untreated rats with STZ diabetes blood glucose levels persisted to be more than 17mmol/L, thus 3-5 times exceeded the values of healthy rats.
The experiment has shown a reliable and stable hypoglycemic effect of both studied lithium salts. The blood glucose level in lithium carbonate-treated diabetic animals on the 7th day was 12.6% lower than in the active control group, whereas on the 14th day the difference in glucose levels with untreated diabetic group amounted to 53.8% in lithium chloride-treated group and to 59.2% in lithium carbonate-treated animals. Subsequently, the hypoglycemic activity of lithium salts stabilized, the glucose level in the experimental groups was – on average – 50% lower than in the untreated STZ group.
These data are confirmed by the measurements of the relative anti-hyperglycemic activity index which points at an earlier onset (day 7) of lithium carbonate therapeutic effect in comparison with lithium chloride. After two weeks of treatment, the antihyperglycemic activity of both lithium salts reached its maximum and remained stable until the end of the experiment.
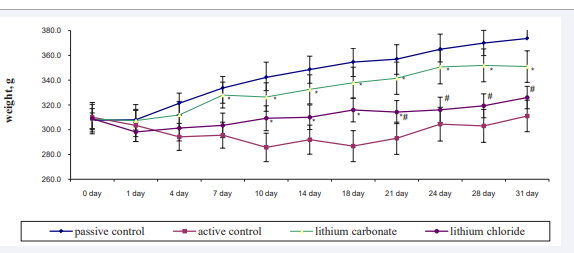
The clear anti-diabetic activity of both lithium salts was characterized by a more prominent increase in body weight of the rats from the experimental groups in comparison to those from the active control group (Figure 2).
Figure 2 The influence of the studied drugs on weight dynamics in Wistar rats Values are given as mean ± SEM for groups * - the significance between experimental and active control groups, ?<0.05 # - the significance between experimental 1 and 2 groups, ?<0.05 F (30, 270) = 5.9167, p = 0.00000
So, the difference of mean weights between the beginning and the end of the experiment was 52.0g (16.2% increase) in healthy animals, while in the active control group this difference was 17.0g (5.8%) only; in lithium carbonate-treated group it was 39.0g (12.5%), and in lithium chloride-treated group – 27.7g (8.9%).
Effect of lithium salts on polyphagia and polydipsia
The antidiabetic activity of the studied compounds was confirmed also by the decrease in the values of polydipsia and polyphagia, which are the most important indicators of diabetes. In the active control group the animals suffered from excessive polydipsia, while in both experimental groups the decrease in water consumption was noted. This effect reached its maximum by the end of experiment: animals of untreated diabetic group daily consumed a volume of fluid more than 200% higher than healthy animals (75.9ml contrary 34.5ml water daily); diabetic animals treated with lithium chloride – 62% less (55.6ml), lithium carbonate – 51% less (55.1ml). We observed also the tendency to the increase in food consumption in the active control group;starting from the third week of the experiment, lithium salts attenuate this increase (healthy rats consumed 23.8g, while daily feed intake in active control group was 27.1g, rats treated lithium chloride – 24.9g, carbonate – 25.0g food).
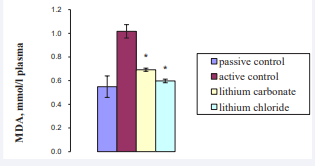
Effect of lithium salts treatment on MDA level
STZ was shown to cause more than a two-fold increase in content plasma MDA level, known to be one of the indicators of free radical processes; both lithium salts eliminate this increase (Figure 3).
Figure 3 Plasma MDA level on 28-th day of experiment Values are given as mean ± SEM for groups * - the significance between experimental and active control groups, ?<0.05 # - the significance between experimental 1 and 2 groups, ?<0.05 F (3, 27) = 28.289, p = 0.00000
Cytoprotective action of lithium salts
In order to get direct evidence of lithium salts’ cytoprotective activity the immunohistochemical analysis of pancreatic tissue using monoclonal antibodies against insulin was performed. This method is characterized by high specificity and enables precise detection of β-cells in islets of Langerhans [15].
The results of morphometric analysis of the pancreas are shown in (Table 1).
Tables
|
Table 1: The morphometric data of pancreatic islets in male Wistar rats. |
|||
|
Group |
Number of islets |
The total square area of β-cells in islets
|
|
|
absolutely, μm2 |
% of the total sample’s square area |
||
|
Passive control
|
17.8±1.89 |
15934.00±4057.55 |
17.8±1.89 |
|
Active control
|
7.19±0.77 |
4106.00±506.1 |
1.15±0.16 |
|
Lithium carbonate
|
9.66±0.98* |
5931.00±919.86* |
2.42±0.33* |
|
Lithium chloride
|
10.52±0.91* |
8255.00±1070.7*# |
1.41±0.12# |
|
Values are given as mean ± SEM for groups * - the significance between experimental and active control groups, ?<0.05 # - the significance between experimental 1 and 2 groups, ?<0.05 F (3, 53)=5.1907, p = 0.00322 |
|||
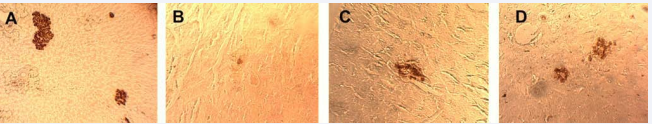
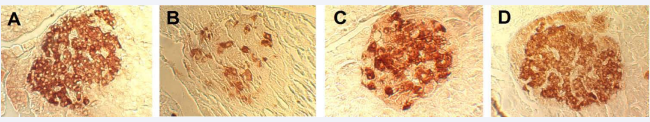
The morphometric study revealed the decrease in quantity of islets, absolute and relative numbers of β-cells in untreated diabetic animals: the amount of pancreatic islets was decreased significantly and the remaining β-cells demonstrated the signs of cellular damage and dystrophic changes (vacuolization, sclerosis) (Figure 4B, 5B). The mean square area of β-cells in untreated STZ-group was about 4100μm2 , four times less than the value of healthy animals. In the group of active control the percentage rate of the total square area of β-cells in cross-section was 1.15%, while in healthy animals it was 17.80% (Figure 4A, 5A).
Figure 4 Pancreatic islets of animals in different groups, Magnification-800? A – The passive control group B – The active control group C – The experimental group treated by lithium chloride D – The experimental group treated by lithium carbonate
Figure 5 Pancreatic islets of animals in different groups. Magnification-1600? A – The passive control group B – The active control group C – The experimental group treated by lithium chloride D – The experimental group treated by lithium carbonate
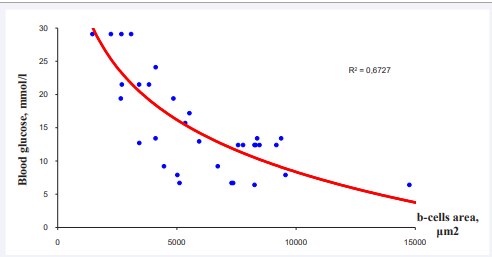
The 28-day treatment of diabetic rats with lithium salts caused the statistically significant increase in the number of the islets and improvement of β-cells morphological features (Figure 4C,D,5C,D). In the lithium salts-treated group the mean quantity of the islets substantially exceeding this value in untreated diabetic animals; the total square area of the β-cells was higher than in the active control. It is worth to underline the sufficient correlation between β-cells area and blood glucose level (correlation coefficient 0.67) (Figure 6).
Figure 6 The correlation between blood glucose level and total square area of pancreatic islets in cross-section of the pancreas
DISCUSSION
The main results of this work are as follows. Using the immunohistochemical method of β-cells detecting, we demonstrated the ability of two lithium salts to restore their number and morphological characteristics that were severely impaired under exposure to STZ. Our data show that STZ at a dose of 40mg/kg causing the development of hyperglycemia and polydipsia, reduces the total area of insulin-producing β-cells compared to healthy animals by 74%, consistent with data obtained by Bonner-Weir S. [15], who showed that the development of clinical manifestations of diabetes in rodents started to manifest when 80% of the islets are deleted. This finding are conformed also with the study of Figeac F. et al. [16], who demonstrated intrapancreatic GSK-3β down regulation by lithium chloride in 90% pancreatectomized rats due to the stimulation of β-cells proliferation and neogenesis. Our data on lithium salts’ ability to reduce the degree of cell damage and a fairly good correlation with the degree of hyperglycemia attenuation indicate the reversibility of the STZ induced morphological and functional manifestations of diabetes.
The available literature data about possible mechanisms involved in regeneration of insulin-producing β-cells are ambiguous. So, according to Cheng Y. et al. [17], the pancreatic proliferative activity on the STZ-model and, possibly, in diabetes is carried out by the conversion of α- and δ-cells to insulinproducing β-cells. Bonner-Weir S. [15], claims that the source of new islets is the epithelium of the pancreatic ducts, which retains the ability to give rise to all differentiated types of cells throughout life. Sun L. et al. [18], suggest that the division of mesenchymal stem cells should be considered as the main mechanism for increasing the number of cells in the process of diabetes pharmacological treatment. With all the differences in the mechanisms’ underlying the reversibility of this pathological process, none of these authors have any doubts about the ability of modern antidiabetic drugs to increase the viability of pancreatic β-cells.
In analyzing possible biochemical mechanisms of lithium anti-apoptotic action, it should be noted that diabetes develops due to multi component metabolic disorders, among which the most important role belongs to the GSK-3β hyperactivity [3,6]. GSK-3β is a negative regulator of cell proliferation including that in β-cells of the pancreas, as it facilitates the degradation of two positive regulators of the cell cycle D1 and E-cyclin, and stabilizes the main negative regulator of the cell cycle p27. Among the most important mechanism for the development of diabetes and its complications is the excess of free radical processes due to the accumulation of peroxide, alkoxy, alkyl radicals, superoxide anion, singlet oxygen and cytotoxic peroxynitrites, which react with phospholipids of cell membranes and damage proteins, lipids, nucleic acids and DNA [19]. In a diabetic condition, the activity of natural factors of endogenous antioxidant protection – superoxide dismutase, catalase, glutathione peroxidase – decreases [20]. Excessive accumulation of free radicals leads to the activation of the inflammatory processes [21]. The oxidative stress caused by hyperglycemia also leads to a shift in the ratio of pro NGF and pro BDNF and their mature forms towards the predominance of precursors, which in contrast to the mature NGF and BDNF provoke the apoptosis of insulin-producing β-cells. This is the main reason of the neurotrophins’ decrease in the blood patients with type 2 diabetes [22,23].
The STZ model reproduces the main pathological mechanisms of the diabetes development, and therefore can be considered as its translational model. Under the conditions of this model there is an increase in GSK-3β expression [24]. Due to the accumulating in β-cells with the participation of glucose transporter GluT 2, STZ causes the increase of reactive oxygen species, including hydroxyl radicals, peroxy radicals and peroxynitrates, which lead to DNA damaging and depletion of NAD+ [9]. STZ is a donor of NO that inhibits the activity of the a?onitase, leading to the alkylation and DNA damage. Pancreatic β-cells are particularly sensitive to the action of free radicals and NO, since they have poorly represented antioxidant system [25]. The STZ model is characterized by a decrease in NGF [26], BDNF [27] and increase the content of pro NGF in the pancreas [28].
Lithium salts exert a selective inhibitory effect on the expression of GSK-3β [29]. They attenuate the manifestations of oxidative stress [30,31]. Lithium enhances the expression of BDNF not only by reducing oxidative stress, but also by activating the transcription of a specific exon IV; lithium was shown to inhibit the proapoptotic genes Bax and caspase-3 [32]. The combination of the listed properties of lithium – to reduce the GSK-3β hyperactivity, to attenuate the expression of free radical processes, to enhance the expression of neurotrophic factors, and to display an anti-inflammatory effect, may contribute to the shown by us ability of lithium salts to restore the number and morphological characteristics of β-cells, severely impaired by STZ.
CONCLUSION
In this work using the highly selective and sensitive methods of β-cells determination, we demonstrated the presence of cytoprotective effects of lithium carbonate and lithium chloride on STZ model of diabetes, reproducing its main pathogenetic mechanisms. Our data on the ability of lithium salts to reliably reduce the degree of cell damage and a good correlation with the degree of attenuation of hyperglycemia indicate the reversibility of the STZ induced morphological and functional manifestations of diabetes. This study designates GSK-3β as a viable drug target for therapeutic intervention on diseases of endocrine and exocrine pancreas associated with cell deficiency.
The data obtained can serve the purpose of translating the fundamental data on these multi-target medicines into medical practice.
ACKNOWLEDGEMENTS
The authors are grateful to Dr. A.B. Michunskaya and Dr. A.V. Sorokina for their help with the morphological study.
REFERENCES
8. Jacobs KM, Bhave SR, Ferraro DJ, Jaboin JJ, Hallahan DE, Thotala D. GSK-3β: A Bifunctional Role in Cell Death Pathways. Int J Cell Biol. 2012; 2012: 930710. doi:
15.Bonner-Weir S. beta-cell turnover: its assessment and implications. Diabetes. 2001; 50:20-24.
19.Marnett LJ. Oxy radicals, lipid peroxidation and DNA damage. Toxicology. 2002; 181-182: 219-222.