A Physiological Soft Tissue Procedure for Hallux Valgus Deformity Correction
- 1. Department of Orthopaedic Surgery, Hong Kong Adventist Hospital, China
Abstract
Hallux valgus is a soft tissue condition of normal bones deviating from their normal alignment due to failure of their stabilizing ligaments. Affected bones are victims rather than culprits. Osteotomy of normal bones to compensate a soft tissue problem can compromise biomechanics of the all-important first ray for function and complicate the matter.
To patients, hallux valgus deformity is mainly a function problem of the foot that can eventually produce secondary problems like clawed toes, collapsed arches, and metatarsalgia and bunionette pain. To surgeons, hallux valgus should always be a function issue and their chosen surgical technique should have been proven capable of improving and restoring foot function.
A thought provoking case is presented to illustrate why a non-osteotomy and non-arthrodesis soft tissue procedure can correct not only a severe hallux valgus foot but also salvage a failed osteotomy procedure.
Keywords
• Hallux valgus
• Metatarsus primus varus
• Bunion
• Syndesmosis procedure
• Osteotomy procedure
• Soft tissue procedure
Citation
Wu DY (2016) A Physiological Soft Tissue Procedure for Hallux Valgus Deformity Correction. JSM Foot Ankle 1(3): 1012.
ABBREVIATIONS
HV: Hallux Valgus; MPV: Metatarsus Primus Varus; TMTJ: Tarso Meta Tarsal Joint; DMAA: Distal Metatarsal Articular Angle; HVA: Hallux Valgus Angle; IMA: Inter Metatarsal Angle; MTP: Meta Tarso Phalangeal
INTRODUCTION
Hallux valgus is a deformity complex made up of mainly normal bones or bones with normal variances moving out of their normal anatomical positions. Its underlying cause is mainly the progressive MPV deformity. Their close association has long been recognized [1].
Metatarsals are held together mainly by a distal soft tissue tie-bar system described by Stains by. The attenuated and stretched medial metatarsosesamoid ligament at its very medial end is usually responsible for the destabilization and gradual varus angular deviation of first metatarsal [2], and the failed medial collateral ligament of meta tarsophalangeal joint (MPJ) was associated with the HV deformity. No real deformity of first metatarsal itself could be blamed but its incompetent ligaments.
The surgical principle for HV correction has been primarily correction of the MPV deformity, which is re-alignment and restabilization of the first metatarsal, and release of contracted distallateral soft tissues for further HV correction if necessary.
After more than 130 different surgical techniques, there is still lack of consensus among surgeons [3]. A large surgical armamentarium is required to manage different deformity severities and no single technique is regarded superior to the others [4,5]. Poorer long term results than expected are still being reported lately and more than 25% of patients are dissatisfied [6,7].
Direct repair or reconstruction of the failed medial ligaments has not been proven effective. Surgical correction of hallux valgus deformity has primarily been relying on the many different osteotomy procedures [8,9] despite the fundamental pathology is in the ligaments, not bones. The concept of rearranging normal bones by osteotomies to correct or compensate for an underlying soft tissue problem may be questionable.
A more ideal and physiological approach is probably to re-align the first metatarsal in its entirety to preserve its normal anatomy. This has already been demonstrated possible by the intermetatarsal cerclage suture technique [10]. After losing its ligamentous support, first metatarsal is unstable and even hyper mobile. This hypothesis has been shown correct, regardless of the severity of MPV deformity [11-13].
Syndesmosis procedure is a soft tissue procedure that uses the intermetatarsal cerclage-suture technique to realign first metatarsal. It also specifically addresses the first metatarsal instability and re-stabilization issue by creating a soft tissue bonding or syndesmosis-like connection between first and second metatarsals in the first intermetatarsal space. Its minimal traumatic and effective re-alignment and re-stabilization of first metatarsal has also been attributed to its fewer complications and consistent function restoration [14].
This case report is to demonstrate that the soft tissue syndesmosis procedure was able to not only correct a severe HV foot and salvage another failed osteotomy procedure at the same time but also restored their function and prevented deformity recurrence.
CASE PRESENTATION
A 61 years old female presented with a severe right HV foot and a left failed osteotomy foot for syndesmosis procedure tomainy resolve her intolerable bilateral transfer metatarsalgia (Figure 1).
Figure 1: Pre-syndesmosis procedure deformities – Relatively, left foot was less deformed than un-operated right foot.
It could be appreciated by her metatarsal calluses (Figure 2)
Figure 2: Pre-syndesmosis procedure metatarsal callus– Left foot had a bigger and thicker metatarsal callus than her right foot.
despite wearing mostly trainers only. She also felt her balance was becoming worse. Her full weight bearing standing AP view x-ray revealed the typical medial displacement of first metatarsal head, widened intermetatarsal space and forefoot of her un-operated right foot. She had undergone a shaft osteotomy procedure of left foot three years earlier that unfortunately did not help its metatarsalgia. Despite its excellent IMA correction to 8.1° (Figure 3),
Figure 3: Pre-syndesmosis procedure standing x-ray: Severe deformities of right un-operated foot were evident by HVA of 52.9°, IMA of 22.7°, complete lateral sesamoid dislocation, incongruent first MPJ and TMTJ and also second MPJ dislocation. Her left foot evidently had undergone a shaft osteotomy procedure previously with residual HVA of 24.9°, IMA of 8.1°,lateral sesamoid dislocation, incongruent TMT joint but congruent first MTP joint
it had still a large intermetatarsal gap and dislocated lateral sesamoid. However, her left MPJ was congruent after osteotomy procedure but not the TMT joint. The advanced severity of her right foot was radiologically evident also by the dislocation of its lateral sesamoid and second MPJ.
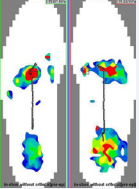
The plantar pressure study by F-Scan® (Ultrathin & Software v6.3, Tekscan, USA) of her feet revealed the same poor force distribution of both feet in walking. Her small stride and flat footed gait was evident by the standing-like pressure pattern of minimal or no force recording under the lateral aspect of mid foot and toes (Figure 4).
Figure 4: Pre-syndesmosis procedure plantar pressure study by F-Scan® – Both feet had an abnormal study. Both great toes could not contribute any force (no pressure registration by colors) for push-off at the end of stance phase. The highest pressure areas (red in color) were registered under mid metatarsal heads in both feet. A normal function foot would have red color registered mostly under the first metatarsal head and great toe. (Pressure color code: red strongest, blue weakest).
The abnormal gait was likely resulted from the severely compromised function of her first rays and avoidance of the push-off phase lest additional metatarsalgia. The pressure and force concentration in the mid metatarsal region verified her metatarsal calluses and metatarsalgia. Her surgical expectation was similar to other suffers to be able to enjoy daily walking activities again [15] (Figure 5).
Figure 5: Schematic illustration of syndesmosis procedure: This surgical sketch demonstrates two of the usual three drill holes in distal first metatarsal and one of three cerclage sutures, scarified opposing cortices for connective tissue in growth and release of lateral collateral ligament. Lateral metatarsosesamoid ligament release was not drawn
SURGICAL TECHNIQUE
Syndesmosis procedure has been well described elsewhere in the past [10-14,16] and its technical details will not be repeated here. Briefly, both feet underwent the same intermetatarsal cerclage suture technique to re-align the first metatarsal of MPV deformity by using #1 PDS® sutures (Ethicon Inc, Somerville, NJ, USA) that were passed through drilled holes in the distal half of first metatarsal after a dorsal first intermetatarsal incision and then around the second metatarsal displacing the partially excised interosseous muscle plant arward. The cerclage sutures were then tied to pull first and second metatarsals together after the usually contracted lateral collateral and metatarsosesamoid ligaments having been released and opposing cortices scarified with osteotome earlier. Complete release of capsular and ligamentous contracture of the right second MPJ and its extensor tendons lengthening were also carried out through the same dorsal incision. A separate medial elliptical excisional incision was also made of her right foot to remove bunion exostosis and redundant soft tissues.
Postoperatively, custom-made removable foot cast-braces were worn for protected walking for three months. As usual, unrestricted extreme activities and high heel shoes were not allowed until six months after surgery.
RESULTS
Clinical
At the patient’s postoperative 6-year follow-up visit, she was very much pleased with her functional results. She had no more metatarsalgia of her right foot or her previously failed left osteotomy foot. Her metatarsal calluses were subsided and did not recur (Figure 6).
Figure 6: 6-year post-syndesmosis procedure photo of soles - Preoperative metatarsal calluses of both feet have mostly subsided in support of resolution of her preoperative metatarsalgia
Her feet felt sturdier and stronger. Her balance was much improved, especially in walking down the stairs. She had since been able to wear all shoes that she could not before without pain, although she had shied away from any high heel shoes and was still having occasional spasm of her left second toe.
Radiological
Full weight bearing standing AP-view x-ray (Figure 7)
Figure 7: 6-year post-syndesmosis procedure standing x-ray – Her right foot HVA was reduced to 25.4°, IMA to 8°. Her left foot HVA was reduced to 14.1° and IMA to 0.7°.
revealed satisfactory re-alignment of first metatarsals of not only improved IMAs but also much narrowed first intermetatarsal gaps that had been maintained by the hypothetical intermetatarsal syndesmosis. Her left foot was also satisfactorily realigned despite its previously failed osteotomy procedure and there were no more signs of MPV recurrence. There was however moderate residual right hallux valgus deformity due to the increased DMAA by reason of the much restored congruence of MPJ (Figure 8).
Figure 8: 6-year post-syndesmosis procedure standing x-ray – Right foot was revealed a DMAA of 20.9° and left 9.1°. Congruence was restored for her MTP and TMT joints in both feet.
It, however, did not affect much of its cosmetic result (Figure 9).
Figure 9: 6-year post-syndesmosis procedure photo–Both feet appeared narrower and slimmer than before. Dorsal surgical scars are evident
Dorsal dislocation of her right second MPJ was well reduced and maintained also.
Biomechanical
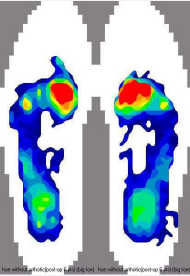
Plantar pressure study by F-Scan® (Figure 10)
Figure 10: 6-year post-syndesmosis procedure plantar pressure study by F-Scan® - The highest pressure/force registration was medialized from mid metatarsal heads to under the first as of normal feet. The pressure tracing similar to normal heel-to-toe gait through lateral borders was mostly restored (pressure color code: red highest, yellow medium, blue lowest)
confirmed biomechanical improvement of her feet to correlate with the disappearance of metatarsal calluses and metatarsalgia and also improved balance. There was marked return (medialization) of plantar pressure back under first metatarsal as of normal feet and away from the preoperatively collapsed metatarsal arch in mid-metatarsal area. However, there was still lack of function of her great toes due probably to prolonged severe preoperative disuse atrophy of flexor hallucis muscles and insufficient rehabilitation exercises on her part. Her heel-to-toe gait was mostly restored although it stopped just short of the hallux.
DISCUSSION
To sufferers, hallux valgus deformity is not just about bunion pain and dilemma with shoes but mainly function problems due to breaking down of the all-important first ray biomechanics. Patients’ expectations have been found different from those of surgeons. Improved walking ability is their most important expectation and then followed by reduced bunion pain and resumption of regular shoes [15].
The ultimate goal of all hallux valgus surgeries is restoration of normal foot function which should be reflected clinically by unrestricted activities and shoes without pain and deformity recurrence. To be able to bear and propel the entire body weight for all common but often stressful activities, the windlass mechanism first ray is complex and structurally it has to be exact. Any surgical technique that alters normal anatomical structures for the sake of straighter great toes is basically a cosmetic endeavor that may not only fail to achieve but even possibly compromise the function objective of HV surgery. A functional HV surgery should be validated biomechanically by objective plantar pressure studies which can also be reflected by spontaneous resolution of biomechanical malfunction related secondary conditions like metatarsal calluses, metatarsalgia and also any flexible lesser toe deformities.
Traditionally, osteotomy procedures have by far been the most popular approach. But this break-n-shift concept of normal first metatarsals to try to correct primarily a soft tissue issue has not been proven biomechanically effective for function improvement [17-20]. This case report demonstrated how this patient’s left foot osteotomy procedure did provide satisfactory first metatarsal re-alignment by definition of its IMA measurement but still failed to resolve her metatarsal callus and transfer metatarsalgia. It also demonstrated that the soft tissue syndesmosis procedure could restore function and resolve transfer metatarsalgia for her severe right foot deformity and also her failed left osteotomy foot by truly re-aligning the first metatarsal to reduce not only IMA but also the actual intermetatarsal gap. Another mechanical reason for her osteotomy procedure had failed to restore proper foot function was probably due to the persistent sesamoids dislocation and impaired windlass mechanism.
Dayton et al have also tried to explain that architecturally the osteotomy paradigm may not be sound or effective3 , but short of implicating also the functional deficiency after a quasi re-alignment of first metatarsal. Their recommendation of a more effective re-alignment technique by Lapidus procedure has also failed to recognize possible functional implications by sacrificing a normal TMT joint. For the minimally traumatic intermetatarsal cerclage suture technique to correct a severe and likely also milder deformities, it is probably only because all HV deformities share the same underlying pathology and are thus all amendable by the same surgical technique if it is accurate in surgical principle.
The increased DMAA, long first metatarsal and oblique TMT joint conditions have all been put forth to justify osseous procedures such as osteotomy and Lapidus procedures, but they have mostly been afterthoughts without prior evidence that these infrequent conditions are abnormal variances that are incompatible with normal foot function and their corrections are necessary. This case report also demonstrated that the increased DMAA (Figure 8) of right foot could be a normal variance because its function was not much compromised after the first metatarsal was truly re aligned, MTP and TMT joint congruence properly restored and sesamoids reduced.
Besides re-alignment, re-stabilization of the first metatarsal is equally relevant to a successful surgery for MPV recurrence prevention and function restoration. This case report demonstrated that without any specific mechanism to restabilize first metatarsal by osteotomy14 of her left foot, there was persistent and possibly recurrent widening of the IMT gap that could have accounted for its abnormal F-Scan study until after the syndesmosis procedure. The syndesmosis assumption had provided her feet with more than 6 years of first metatarsal stability without any signs of impending failure. Syndesmosis procedure enlists body’s natural reparative reaction to form fibrous connective tissues in the first intermetatarsal space to reconnect first metatarsal to the second metatarsal to prevent MPV recurrence. This phenomenon has been consistently observed and shown to be lasting also [12,13,16].
Medial deviation of first metatarsal of the MPV deformity would change the orientation and congruence of MTP joint at its distal end and that of TMT joint at its proximal end (Figure 3). The function implications and need for incongruent MTP joint correction has been much discussed, but not for TMT joint yet. To re-orient both MP and TMT joints at the same time, first metatarsal needs to be re-aligned in entirety by non-osteotomy means like the syndesmosis procedure (Figure 7). Restoration of normal congruence to TMT joint should be regarded equally important as to MTP joint for normal foot function until proven otherwise.
The purpose in presenting this particular case was not to prove the syndesmosis procedure but to help surgeons look at the HV condition from a less viewed angle and a less considered surgical principle. HV is fundamentally and pathologically a soft tissue issue and in principle best dealt with by soft tissue means, if possible, to preserve anatomical integrity of normal bones for maximal function restoration. Hopefully, this case report can help provoke more thinking and discussion of HV corrective surgery outside of the osteotomy box.