A Retrospective Review for Evaluating the Treatment of Hallux Rigidus Utilizing the Arthrosurface Total Toe Implant System
- 1. Precision Orthopedic Specialties, Inc., University Hospitals Department of Podiatric Medicine and Surgery, USA
Abstract
Hallux rigidus is a condition, which is defined as degenerative arthritis of the first metatarsophalangeal joint. Hallux rigidus occurs due toe repetitive micro trauma or wear and tear on the first MPJ. The surgical treatments for the condition are thought of in two ways: joint salvage or joint destruction. The total implant discussed throughout this paper is a joint salvage technique. Joint salvage procedures aim to preserve the motion of the first MPJ. This study was conducted using the Arthrosurface ToeMotion Total Toe System™. The study consisted of using 17 implants in a total of 14 patients. The Arthrosurface ToeMotion Total Toe System™ is comprised of a poly-metal interface as opposed to some the earlier designs utilized for first metatarsal phalangeal joint implantation. In considering treatment implications, it is to be noted that the patients in this study were either a Coughlin stage 3 or 4.
During follow up the patients were assessed clinically and radiographically. The goal of surgical intervention was to achieve a 50% improvement of patient’s symptoms and function of the first metatarsal phalangeal joint. All patients were available for follow up and their outcomes, which were assessed using modified AOFAS scores. Throughout the years there have been numerous total implant designs. The benefits of using the Arthrosurface ToeMotion Total Toe System™ are that it preserves the length of the first ray as opposed to other techniques, which require resection of bone prior to implantation.
Keywords
• Hallux Rigidus
• Toe Implant
• Arthroplasty
Citation
Mendeszoon M, Jones C (2017) A Retrospective Review for Evaluating the Treatment of Hallux Rigidus Utilizing the Arthrosurface Total Toe Implant System. JSM Foot Ankle 2(1): 1020.
BACKGROUND
Physical exam
When the patient presents with pathology of the 1st MPJ, one of the most common complaints is pain. During the examination, the physician typically finds that the pain is at the end range of motion with plantar flexion and dorsiflexion. Occasionally there can be an associated dorsal prominence over the first MPJ, which usually indicates there are bone spurs associated with the pathomechanics of the first metatarsal phalangeal joint. Crepitus is another finding of 1st MPJ pathology. Crepitus is defined as grinding sound or sensation produced by friction between bone and cartilage. In the later stages of hallux rigidus, there is a complete lack of motion [1].
Radiographic studies
Before any treatments are offered a series of radiographs should be taken to assess the pathology of the first MPJ. This usually consists of the lateral, anteroposterior, and the medial oblique views of the affected foot. The AP view allows the practitioner to assess the joint space, while the lateral and MO views will show any associated spurring around the joint as well as the joint space. Occasionally loose bodies or sub chondral cysts are seen in any view taken. Sclerosis of the bone may also be seen on the radiographic studies since this is one of the ways that the bone tries to heal itself (Figure 1-4).
Figure 1: Pre operative Radiographs. This is a radiograph of a patient that presented to the clinic with a previous attempt at a 1st MPJ fusion that has failed. The patient elected to undergo a revisional procedure with the Arthrosurface total implant.
Figure 2: In this radiograph you can see the flattened appearance of the metatarsal head as well as significant joint space narrowing.
Figure 3: This is the radiograph of a patient whose initial surgery consisted of a hemi implant. The patient was not doing well with this type of implant and decided to undergo a second procedure and have it converted using the Arthrosurface total implant
Figure 4: In this radiograph, there are substantial cystic changes occurring in the first metatarsal head. There is also a significant loss of the joint space
Treatments
For the early stages of hallux limitus/ rigidus, it may be appropriate to treat the patient conservatively. This usually entails non-surgical treatments. Shoe modification is one of these modalities. Extra depth shoes can be utilized to accommodate spurring of the 1st MPJ (Figure 5).
Figure 5: This patient presented as a surgical consult for bilateral hallux rigidus pain and elected to have both 1st MPJ’s reconstructed with the Arthrosurface total implant.
Shoes with a rocker sole in the ball of the foot can also be used so that there is less need for the joint to flex, which prevents painful motion of the 1st MPJ. Another non-surgical treatment option is the use of NSAIDs to decrease the amount of inflammation in the area. Functional orthotics is another treatment modality that may be utilized in mild 1st MPJ arthritis. One of the most common orthotic devices used is a Morton’s extension. The way this device works is that if prevents motion in the first MPJ by decreasing the ROM needed for function. Since the device is rigid, there is less movement in the joint, which results in less pain for the patient since the arthritic surfaces are not gliding against each other as much as it would without the device in place [2].
JOINT DESTRUCTIVE PROCEDURES
Keller Arthroplasty
The Keller arthroplasty is a procedure indicated for a reduction of joint pain and has been a mainstay of hallux limitus and rigidus surgery for many years. The procedure is still useful and effective in selected patients, particularly as an alternative to an implant. The Keller arthroplasty may be considered as a salvage procedure for iatrogenic complications or arthritic joints. In the Keller arthroplasty, the proximal 1/3 of the proximal phalanx is rejected while the first metatarsal head is left intact, although any osteophytes may be removed.
First MPJ arthrodesis
For many, first MPJ arthrodesis is thought of as the gold standard for treatment of hallux limitus/ rigidus. Arthrodesis of the first metatarsophalangeal has been considered for significant degenerative changes at the first metatarsophalangeal joint and evidence of instability at the first metatarsophalangeal joint. This is done by resecting portions of the 1st metatarsal head and the proximal phalanx then bringing those surfaces together and fixating them with screws or a combination of screws with a plate.
JOINT PRESERVATIVE PROCEDURE
Cheilectomy
Cheilectomy is the removal of the osteophytic proliferation about the metatarsal head or the proximal phalangeal base. In some cases, the dorsal ¼ to 1/3 of the metatarsal head is transected to increase the motion of the first metatarsal phalangeal joint (Figure 6 & 7).
Figure 6: Right and left feet prior to 1st MPJ Arthrosurface Total Toe implant.
Figure 7: Incision placement. Dorsal and slightly medial to EHL tendon.
Hemi and total implants
Implant arthroplasty has played a major role in the advancement of surgery for painful arthritic joints. Implants for the first metatarsophalangeal joint have provided thousands of patients with the opportunity to ambulate with a pain-free functional first ray. Some authors have applauded the versatility and effectiveness of implants for hallux rigidus. The two types are the total and the hemi implant. The total implant has segments for both the first metatarsal and the proximal phalanx, while the hemi may only have a segment for the proximal phalanx [3].
The Arthrosurface implant consists of a metatarsal component and a phalangeal component designed for resurfacing the 1st metatarsal head and the base of the proximal phalanx. These two implants replace the metatarsophalangeal joint by complete functional preservation of the joint and maintaining of the sesamoid complex (Figure 8).
Figure 8: Drill guide is placed on the metatarsal head.
Surgical procedure
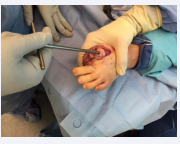
The patient is placed supine on the operating table, with the operative extremity in a well-padded position. The procedure can be done with either general anesthesia or monitored anesthesia care [4]. Depending on the patient, a regional block may also be utilized in the form of a popliteal or ankle block. Generally, an ankle tourniquet is also utilized along with the use of an Esmarch bandage wrapped around the foot carried to the ankle, prior to tourniquet inflation (Figure 9,10).
Figure 9: Wire is driven into the 1st metatarsal
Figure 10: Surface reamer is placed over the guide pin and reamed until the laser line is flush with the cartilaginous area.
A dorsal incision is then made with a #15 blade over the first metatarsal phalangeal joint, slightly medial to the extensor hallucis longus tendon. To expose the joint capsule a combination of sharp and blunt dissection is used through the subcutaneous tissues. Care is taken to protect the neurovascular structures and electrocautery is used as needed. The extensor hallucis longus tendon is freed from the capsule and retracted laterally to keep the tendon within its sheath. A longitudinal arthrotomy is made along the medial border of the joint, and the capsule is elevated off the bone. A complete release of the collateral ligaments, sesamoidal suspension ligaments, and capsule should be made so that the entire joint, including the sesamoids, is easily visualized [5,6]. It is very important to visualize the articular edge of the sesamoid crista on the metatarsal head because this is the landmark for placement and sizing of the implant. A curved osteotome, freer or Mc Glammary elevator can be used to release these plantar adhesions. Care should be taken to avoid damage to the metatarsal-sesamoid articulation (Figure 10,11).
Figure 11: Insertion and removal of the trail cap.
SURGICAL TECHNIQUE: FIRST METATARSAL PREPARATION
I. Once the incision is made and the area is thoroughly dissected the drill guide is placed on the first metatarsal head with the plantar portion of the guide just below the crista. Next, a guide wire is driven into the 1st metatarsal. Proper placement is then checked via fluoroscopy.
II. The drill is then guided over the pin and drilled until the proximal portion is flush with the articular surface of the first metatarsal head
III. On the tap there is an etchedline, which indicates how far it needs to be tapped in. Use a mallet until that line is flush with the first metatarsal head.
IV. Place the driver into the taper post and advance it until the line on the driver is flush with the cartilaginous area of the first metatarsal head making sure that it is central to the defect.
V. Clean the taper and then place the trial cap into the post. Adjust the depth of the trial cap if needed, and use caution to make sure it is not above the area of the deficit.
VI. Remove the trial cap then place the centering post into the taper. Next place the contact probe over the centering shaft. Read the contract probe then select the appropriate size for the articular component via the sizing chart
VII. Take the corresponding reamer and ream the central portion of the first metatarsal shaft where the implant will be seeded
VIII. The dorsal reamer guide is then placed into the taper. Drive the Surface Reamer over the Guide Pin until it contacts the top surface on the Taper Post.
IX. Place the Dorsal Reamer Guide into the taper of the Taper Post. The Guide should be oriented such that the Dorsal Reamer is at the 12 o’clock position. Advance the Dorsal Reamer to the depth stop. Once the Dorsal Reamer has advanced to the handle, remove the Dorsal Reamer Guide.
X. Place the Sizing Trial into the defect that matches the offset profile of the chosen DF Articular Component. Make sure the trial is congruent with the edge of the surrounding articular surface. Check the range of motion making sure you are able to achieve 90 degrees of dorsiflexion. Removal of all osteophytes and non-essential bone on the metatarsal head.
XI. Next, remove osteophytes from the phalanx. If needed, defer osteophyte removal until Phalangeal Component is positioned.
XII. Align the DF Articular Component on the Implant Holder. The etch marks on the back of the DF Articular Component should be aligned with the etch mark on the handle of the Implant Holder. Make sure the off sets for each portion are aligned, and then insert the taper into the Taper Post.
XIII. Tap the Impactor to seat the DF Articular Component until the Articular Component is firmly seated on the bone and into the Taper Post (Figure 12).
Figure 12: Insertion of both implant components.
SURGICAL TECHNIQUE: PROXIMAL PHALANX PREPARATION
I. Using the Pin Drill Guide, place the 1.5mm Guide Pin central to the phalangeal surface, in line with the axis of the bone. Confirm placement with fluoroscopy.
II. Introduce the Reamer over the guide pin and advance until the Reamer depth indicator is flush to the phalangeal articular surfaces.
III. Introduce the Tap over the guide pin and advance, until the Tap depth indicator is flush to the level of the phalangeal articular surface.
IV. Next, insert the trial to determine the phalangeal insert for the Fixation Component. The medial and lateral offset of the Phalangeal Insert should match the medial and lateral offset of the DF Articular Component.
V. Perform final range of motion evaluation (Figure 13).
Figure 13: Final placement of the Hemi CAP DF Articular Component and DF Articular Component prior to closure.
RESULTS
There were 14 patients involved, (eight females and 6 males), in this study. Of the 14 patients, this was a secondary procedure for four of them. Three patients had bilateral implants placed, while 11 patients had a single implant placed for a total of 17 implants. The average age of the patient was 60.8 years with the range being from 54-69, and the median age being 61 years old. Radiographs were taken pre and post operatively to assess each patient’s affected joint. Following surgical intervention, the patient’s progress was reassessed in the clinic at each postoperative appointment. The postoperative appointments were scheduled for 1 week, 2 weeks, 6 weeks, 3 months, and 6 months (Figure 14).
Figure 14: Checking proper implant placement and range of motion via intraoperative flouroscopy after insertion of the Arthrosurface total toe implant
The patient’s were then categorized into two groups: primary procedures and secondary procedures. A person undergoing a primary procedure meant that this was their first surgical intervention for addressing their hallux rigidus. A person in the secondary group meant that they had previous surgical intervention. A scoring system similar to that of the AOFAS scoring system was used, but tailored to the first metatarsal phalangeal joint. The three main categories of the scoring system were pain, function, and alignment. The higher the patient’s score total, the better the outcome of the procedure (Figure 15).
SUBJECTIVE DATA
Pain Scale: 20 points total
| No Pain (20 points) | Mild/ occasional (10 points) | Moderate/ daily (5 points) | Severe/ all the time (0 points) |
| 7 | 6 | 3 | 1 |
Daily shoe gear: 10 points total
| Any shoes (10 points) | Comfortable shoe (5 points) | Modified shoe or brace (0 points) |
| 9 | 8 | 0 |
Activity limitations: 15 points total
| No limitation (15 points) | Mild to moderate limitation(7points) | Severe limitation (0 points) |
| 12 | 4 | 1 |
Joint Motion: 10 points total
| No restriction (10 points) | Mild to moderate (5 points) | Severe restriction (0 points) |
| 16 | 1 | 0 |
OBJECTIVE DATA
Statistical analysis was then utilized and determined a p value of 0.152. Based on the patient scores, no statistically significant difference was found between those who had undergone a primary or secondary procedure. However, it is interesting note that while the calculated scores may be low for some, the patient was still satisfied with the outcome with the exception of one patient.
MPJ ROM: 20 points total
| Normal: 75 degrees or more (20 points) | Mild to Moderate Restriction: 30 - 74 degrees (10 points) | Severe Restriction: Less than 30 degrees (0 points) |
| 4 | 11 | 2 |
Joint alignment: 15 points total
| Good (15 points) | Fair (7 points) | Poor (0 points) |
| 10 | 7 | 0 |
Callus formation on radiographs: 5 points total
| No callus (5 points) | Callus (0 points) |
| 16 | 1 |
Implant stability: 5 points total
| Stable (5 points) | Unstable (0 points) |
| 17 | 0 |
DISCUSSION
The patients that participated in this study lead relatively active lifestyles. Almost all patients in the study work full time, with only one being retired. For those that are employed they work an average of 40 hours a week with a significant portion of that time standing or doing a job that requires some degree of motion at the first metatarsal phalangeal joint. This is due to the fact that they may have to stoop or crouch down. Outside of their employment gardening and farming were common hobbies that the patient’s partake in. In doing these activities, it is imperative that there be some degree of motion at the first metatarsal phalangeal joint, and most importantly, lack of pain with doing so.
Numerous characteristics were taken into consideration while carrying out this study. The first category that we broke the patient’s into was whether this was a primary or secondary procedure. A primary procedure means that this was the first surgical intervention to treat hallux rigidus, while secondary means that they had had prior intervention. For those that fell into the secondary category the previous interventions consisted of a silicone implant, hemi implant, and non-union of 1st MPJ fusion.
When a patient chooses to undergo surgery, there are inherent risks associated with doing so, in which every precaution is used to ensure that complications do not arise. The most common complications associated with correction of hallux rigidus are infection, non-union, mal union, improper function or complete loss of function.
It is necessary to point out that the scale used to assess patient’s outcomes in the postoperative period were more subjective than objective. While radiographs were analyzed to prove that joint space was preserved and clinical evaluations were done to prove that joint range of motion was increased, overall success of the surgery was based on how patient’s felt in regards to how they felt prior to surgical intervention.
Due to the subjective nature of the study, the statistical results would benefit from a larger sample size. The goal of the study was to determine if those who had undertaken the procedure had at least a 50% improvement from what they were prior to surgical intervention.
CONCLUSION
All patients were available for follow up, and most were satisfied with their outcomes, with only one patient seeking to have the implant removed. The Arthrosurface ToeMotion Total Toe System™ preserves the length of the first MPJ, re-approximates anatomy, and conserves bone and soft tissue by using the Metatarsal based Hemi CAP DF and an inlay, screw-based Phalangeal component. This creates an environment for the first MPJ to be mobile while other types of implants are fixed at one component. As this is a relatively new product, we look forward to seeing the long term follow up results. However, after analyzing the results thus far, they appear promising, and we will continue to use this product. The future goal of this study is to eventually have a large enough population size to illustrate more statistically significant results.