Biomechanical Analysis of UCBL or Articulated AFO in Stage II Posterior Tibial Tendon Dysfunction
- 1. Department of Orthopedics and Rehabilitation at Jackson Memorial Hospital, University of Miami Miller school of Medicine, USA
- 2. Department of Pediatrics, Mount Sinai Medical Center & Miami Heart Institute, USA
- 3. Department of Pediatrics, Jackson Memorial Hospital, USA
- 4. Max Biedermann Institute of Biomechanics, Mount Sinai Medical Center, USA
Abstract
Background: Weakening and partial rupture of the posterior tibial tendon (Stage II PTTD), is a common precursor to posterior tibial tendon rupture which leads to pes planus followed by a high probability of a need for surgical interventions and ultimately triple arthodesis. Early detection of the Stage II PTTD can prevent this vicious cycle of biomechanical failure. The goal of early intervention is to prevent pronation and valgus motion at the subtalar joint.
Hypothesis: An ankle-foot orthosis (AFO) with a UCBL footpiece and articulated ankle joint (UCBL/AFO) will maintain a physiological anatomical position of the hindfoot, midfoot, and forefoot without sacrificing free ankle range of motion in dorsiflexion and plantarflexion.
Methods: Four human cadaver legs had Stage II PTTDsimulated with a scalpel by the same surgeon (ACB) through a small incision over the medial aspect of the foot and ankle. Surgical classification of posterior tibial tendon rupture Type 11 is a partially torn, attenuated tendon. (Classification system with CT and MR imaging with surgical correlation. Radiology, 169: 229-235, 1988). Each leg was casted and a mold was modified upon which a UCBL/AFO was custom fabricated. Ten Nm dorsiflexion, plantarflexion, varus and valgus loads were applied to the cadaver foot while fluoroscopy imaged the positions of the subtalar joint/hindfoot complex both with and without the UCBL/AFO. Measurements were made from the images with Image pro software.
Results: The UCBL/AFO had minimal effect on sagittal ROM: 47.6º ± 19.8 without; and, 45.5º ± 21.6 with the UCBL/AFO. The UCBL/AFO controlled coronal plane ROM (p < 0.002): 27.0º ± 9.0 without; and, 9.7º ± 3.3 with the UCBL/AFO. The UCBL/AFO was most effective at reducing valgus motion: 19.4º ± 8.5 vs. 5.1º ± 1.1, which was only 27.7% ± 13.2% of the unsupported motion, (p < 0.002); compared to varus motion: 7.7º ± 2.5 vs. 5.6º ± 2.2, which was 74.3 ± 44.2%, (not significant).
Conclusions: The UCBL/AFO is a functional brace that effectively controls the pathological valgus motion that occurs in the subtalar joint/hindfoot complex when there is a stage II PTTD, while maintaining physiologic sagittal motion at the ankle joint and MTP joints.
Level of Evidence: Not applicable, this was a biomechanical study in cadaver limbs.
Keywords
• PTTD
• Foot-ankle
• Valgus
Citation
Diamond M, Bonner AC, Pedroso D, Milne E, Latta L (2016) Biomechanical Analysis of UCBL/Articulated AFO in Stage II Posterior Tibial Tendon Dysfunction. JSM Foot Ankle 1(2): 1007
INTRODUCTION
The most common cause of adult acquired flatfoot arises as a result of PTTD. Typically, this develops unilaterally in middle aged women with other comorbidities such as obesity, Diabetes Mellitus, prolonged steroid use and or local steroid injection infiltration. More recently, quinolone antibiotic usage has been implicated as an etiology of spontaneous tendon ruptures in the lower extremity. In Posterior tibial tendon dysfunction, the tendon often becomes chronically inflamed, weakened and either tears or ruptures creating a painful a propulsive gait and dysfunctional limb. The Tendon pathology is typically classified according to grade of tendon morphology i.e. inflammation, partial or incomplete tear and finally complete tear.
A common clinical examination (“Jack’s test”, Ewen A. Jack, BJBJS 1953) is available to determine the normal function of the posterior tibial tendon (PTT). If the patient has a tight Gastrocnemius or Tendo Achilles, then this test will be compromised and will probably not be of clinical significance. The patient will stand on their toes and the examiner will observe the position of the heel from the rear. If the heel goes into varus, (i.e. inverts), then the posterior tibial tendon is more likely functional. If the heel stays in neutral or valgus position, then the PTT is most likely dysfunctional. With the patient standing in normal base of gait, the examiner can stand behind the patient and observe the forefoot. The appearance of” too- many- toes|” on the affected side with dysfunction is commonly observed. This is attributed to the excessive pronation of the hindfoot with concomitant internal compensated tibial rotation, allowing visualization of the forefoot which assumes an abducted position [1-4].
In 1989, Johnson and Strom have developed guidelines for staging of PTTD describing physical and radiographic appearance with their potential treatments as can be seen in Table (1).
Table 1: Johnson and Strom Classification of PTTD.
| Stage 1 | Stage 2A- Early | Stage 2B- Late | |
| Physical Appearance | Medial rear foot pain Localized swelling to course of posterior tibial No positional change in arch |
Medial rear foot pain Tendon swelling, warmth, tenderness+/- perform single heel raise Rear foot valgus; too many toes |
Same as 2A-Early Positional change in arch; rear foot valgus Lateral pain; sinus tarsi, sub fibular tenderness |
| Radiographic Appearance |
X-Ray: no change
MRI: tenosynovitis
US: fluid around tendon |
X-ray: peritalar subluxation; increased talar 1st MT angle MRI: tenosynovitis; attenuation of tendon; tendinosis US: tenosynovitis; attenuation of tendon; tendinosis |
X-ray: Same as 2A-Early; progressive angular changes MRI: Same as 2A-Early; TP rupture; early DJD (subchondral edema) US: Same as 2A-Early; tendon rupture |
| Treatment Options |
Nonsurgical: Short-leg cast or walking boot; physical therapy; orthoses Surgical: Synovectomy |
Nonsurgical: orthoses
Surgical: synovectomy; tendon transfer; osteotomies; arthroereisis |
Nonsurgical: UCBL; AFO
Surgical: same as 2A-Early; isolated rearfoot fusions; medial column fusion |
MRI is the gold standard for diagnosis of this condition (Table 2).
Table 2: Conti et al classification of Magnetic Resonance Imaging of Posterior Tibial Tendon ruptures.
| Stage | Characteristics |
| Type IA | The MRI shows one or two fine longitudinal splits in the posterior tibial tendon without evidence of intrasubstance degeneration. The splits are frequently on the undersurface of the tendon. Clinically, this appears to correlate to a short period of symptomatology of less than 6 months, with minimal tendon tenderness or swelling and no heel valgus on physical examination |
| Type IB | The MRI demonstrates an increased number of longitudinal splits with an increase in tendon width with mild surrounding fibrosis. There is no significant tendon degeneration. The clinical symptoms are similar to that of type IA, but have been presents for 6 to 12 months. |
| Type II | The posterior tibial tendon is narrowed on the MRI, with long longitudinal splits and intramural degeneration. Often, the tendon has bulbous appearance distal to attenuated portion. This corresponds to the onset of increased hindfoot valgus and a history of symptoms of 1 to 1/1/2 years. |
| Type IIIA | This is notable for more diffuse swelling of the posterior tibial tendon, with uniform degeneration becoming a prominent feature. There are few strands of the intact tendon through the area of the degeneration. The patient at this stage demonstrates minimal inversion strength and marked heel valgus. The generally have had symptoms for more than 2 years. |
| Type IIIB | There is complete rupture of the posterior tibial tendon on MRI with, with complete replacement of the tendon by scar tissue. At this stage, the patient demonstrates the classic findings of a complete posterior tibial tendon rupture, with symptoms exceeding 2 ½ years in duration. |
(RSNA (2012) Nov 27/Chicago Illinois). Photo of a MRI demonstrating a Type II tear of the posterior tibial tendon with arrow annotating bulbous intrasubstance appearance on Sagittal TI image (Figures 1-3).
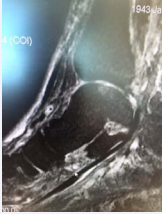
Figure 1: Frontal T2 fat suppression MRI image of 67-year-old female with chronic left ankle pain with marked edema and partial tear of Posterior tibial tendon. Note the valgus position of the calcaneus
Figure 2: Sagittal T2 Fat suppression MRI image of a 62-year-old female with partial tearing of the Posterior tibial tendon. Note the inflammation along the posterior tibial tendon in the typical zone of injury, 1-2 centimeters from the medial malleolus
Figure 3: Axial T2 Fat suppression MRI image of 62-year-old female demonstrating posteriortibial tendon partial tear with edema and fraying noted.
Ultrasound is also utilized for diagnosis of this tendon pathology and it is readily available, however, it is operator dependent. Plain radiographs are helpful but they are not usually diagnostic. When visualizing plain radiographs, there is a declination in the calcaneal inclination angle and the cyma line will demonstrate a talar navicular break. These findings are readily apparent on the lateral weight bearing radiograph with an associated pes planus valgus deformity.
Treatment of PTTD can be surgical, i.e. medial calcaneal displacement osteotomies, Peroneal tendon augmentation repair, triple arthrodesis, or non-surgical with a cast or functional brace. The latter provides a much less invasive and less costly option to the patient. The surgical optionscan be explored if the initial conservative treatment does not suffice and the patient has no improvement or deteriorates after trying an initial period of immobilization or bracing (usually 6 months). There are not any current valid studies demonstrating the cost effectiveness of functional bracing versus surgical correction of the dysfunctional posterior tibial tendon [5]. Time out of work necessary for surgical intervention would certainly be a consideration in choosing the treatment modality for this common pathological entity. The rehabilitation after this surgery can be exhaustive requiring extensive physical therapy and continued bracing. Moreover the patient’s activity expectations need to be taken into consideration when determining the most beneficial and cost effective method of treatment [6-8].
In order to construct the brace, the orthotist casts the live patient in a neutral heel (i.e. no calcaneal valgus or varus) neutral subtalar joint position. Clinically, hindfoot valgus or pronation causes further stretching and injury to the posterior tibial tendon by placing this structure under stressful physiological tension. As a preventative measure, the orthotist casts the patient by capturing the medial column before it reaches a pathological position i.e. excessive hindfoot valgus or pronation and thus captures the foot before it causes further stress and potential damage to the pathological tendon. This is highly subjective and depends upon the expertise of the orthotist and his communication with the patient. The ability of the orthotist to manipulate the hindfoot into valgus is critical. When the manipulation reaches a point of subjective discomfort in the posterior tibial tendon, the valgus (pronatory) stress is slightly reduced and the patient is casted in this asymptomatic position. This is an important concept and technique because the ankle and subtalar jointsare“functionally” braced in a position which does not endanger or aggravate the dysfunctional posterior tibial tendon. (ACB) The tendon is prevented from obtaining the position which is likely to cause further physiological tension, tearing and discomfort. The deforming pronatory valgus action across the talar-navicular joint is neutralized while allowing free dorsiflexion and plantarflexion. The brace is fabricated from the positive cast of the patients’ foot-ankle complex (Figure 4).
Without this conservative functional bracing, it is believed that the tendon, if left unprotected, will eventually succumb to valgus pronatory hindfoot stresses causing a likely complete rupture and potential advancement to stage 111 dysfunction or end stage adult acquired flatfoot deformity with associated Peroneal tendon pathologies and arthritis. The hindfoot will assume a fixed and non-reducible valgus position and oftentimes require surgical intervention via combinations triple arthrodesis, calcaneal osteotomy, and tendinous augmentation or repair in select patients. Other conditions such as sinus tarsi syndrome and peroneal tendon pathology are commonly observed in stage III dysfunction and represent other pathologies associated with PTT. The loss of ambulatory status is significantly altered in this condition and the patient develops an extremely antalgic gait pattern with compensation at the affected knee, hip and lower back [9,10].
Purpose
This study was designed to address the question of whether a UCBL with articulated AFO can limit the subtalar joint complex from reaching maximum pronation or valgus with functional bracing. The purpose of controlling pronation and valgus is to decrease further damage to the PTT in stage II PTTD. Furthermore, this study will seek to measure if functional bracing of the foot-ankle complex can maintain the talus/calcaneus (hindfoot) beneath the tibial plafond which should prevent further valgus stress/eversion of the hindfoot which might create more stress and damage to the dysfunctional posterior tibial tendon (Stage 11 PTTD). The authors recognize that a significant limitation of this study is the use of cadaveric specimens with their inherent stiffness and lack of normal tissue flexibility. Moreover, the ability to determine whether these cadaveric specimens were void of any underlying connective tissue disorders or other contributing pathologies was not possible. The use of this orthosis i.e. the UCBL with articulated AFO, represents a conservative method of treating the complex entity of Posterior tibial tendon dysfunction stage 2 via functional bracing and the results of this study in cadaveric specimens are presented. A prospective study of this pathological entity obtained withvideo gait analysis in live patients with utilization of the UCBL with articulated AFO presents an area of clinical interest.
MATERIALS AND METHODS
Four fresh frozen grossly normal appearing cadaver legs were selected and thawed to the point that the ankle and subtalar joints could be moved into the appropriate position for casting. It was not possible to determine whether these cadaveric specimens had any particular connective tissue disorder. A plaster mold was made of the foot, ankle and the distal calf. Each leg was then refrozen for later testing. The mold was delivered to the Prosthetics Laboratory, (Jackson Memorial Hospital/ Dept of Orthopaedics and Rehabilitation, Miami. Fl.), where the orthotist, Dennis Pedroso, poured a positive plaster mold, modified the mold and fabricated a custom USB footplate, a calf shell and a polyaxial articulated ankle joint with Gillette joints assembled into a UCBL/AFO (Figure 4).
Figure 4: UCBL with Articulated AFO.
IRB approval was obtained through Mt Sinai Medical Center for this cadaveric research study. The UCBL/AFO was taken to the Max Biedermann Research Institute/ Biomechanics Laboratories Mt Sinai Medical Center, Miami Beach. The frozen cadaveric leg was thawed and the tendon rupture (partial) stage II, was simulated by the same surgeon (ACB). A longitudinal cut was made with a scalpel in the posterior tibial tendon of each cadaveric ankle to simulate a tear that would be representative of a Stage II PTTD (Figure 5).
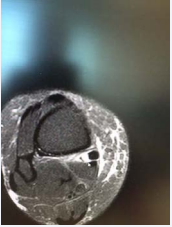
Figure 5: Posterior tibial tendon demonstrating partial longitudinal tear of the Posterior Tibial Tendon. This is created on a cadaveric specimen to demonstrate Type 2 Partial Tear of Posterior Tibial Tendon approximately1-2 centimeters distal to the medial malleolus
This simulated tear was located in the distal aspect of the posterior tibial tendon between the medial malleolus and the tuberosity of the navicular, where the pathology in the tendon typically occurs in MRI and physical examinations. Clinically, these tears are often longitudinal in direction and they typically represent incomplete or partial tears of the tendon.
Testing was performed with the cadaveric limb in a tennis shoe that was firmly secured with 1/2 inch (12.5 mm) steel bolts to a piece of 5/8 inch (16 mm) plywood (Figure 5), 50 X 30 cm. A 1 inch (25.4 mm) square block was mounted on the bottom of the plate and aligned to the center of the projected axis of the tibial diaphysis (Figure 6).
Figure 6: Laboratory Set-up of test platform with AFO/UCBL applied to inverted cadaveric limb and secured to test platform.
Four marks were made on the bottom of the plate: each one 10 cm from the center of the block, one medial, another lateral, another anterior and the last one posterior.
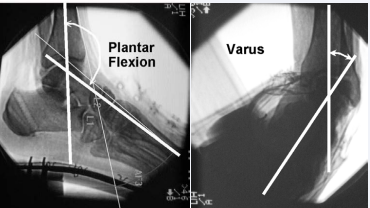
A force of 100 N was applied perpendicular to the plate at each of the 4 spots with a digital dynamometer to create a 10 N-m moment in each direction; varus, valgus, dorsiflexion and plantar flexion. Next a torque wrench was mounted to the block and a 10 N-m internal rotation was applied, followed by a 10 N-m external rotation moment. The loading cycles were recorded by the fluoroscopic c-arm on video in the sagittal and frontal planes. Single images from the fluoroscopic video were captured at the peak of each load cycle in plantar flexion, dorsiflexion, valgus, varus, and internal and external rotation for joint position analysis. Then, the foot was placed in the UCBL/AFO articulated ankle, and the same testing and recordings were repeated (Figure 7).
Figure 7: Fluroscopic frames captured from the video and measured with Image Pro.
Image pro’ software was used to analyze the angles of joint positions for each frame captured from the fluoroscopic videos. The angle between the tibial shaft and the calcaneus were used to define the varus and valgus angles from the frontal plane views. The angle between the tibial shaft and the 2nd metatarsal on the sagittal plane frames were used to define the range of plantar and dorsiflexion.
Statistical comparison of all measures was made for each measure of joint position comparing the supported vs. unsupported condition of each limb. The unsupported limb measures were considered to be the controls and the supported measures, the dependant variable. Comparisons were made by paired student’s t-test of the % difference for each individual limb [11,12].
RESULTS
The UCBL/AFO had minimal effect on sagittal ROM: 47.6º ± 19.8 without; and, 45.5º ± 21.6 with the UCBL/AFO. The UCBL/ AFO controlled coronal plane ROM (p < 0.002): 27.0º ± 9.0 without; and 9.7º ± 3.3 with the UCBL/AFO. The UCBL/AFO was most effective at reducing valgus motion: 19.4º ± 8.5 unsupported vs. 5.1º ± 1.1 supported, which was only 27.7% ± 13.2% of the unsupported motion, (p < 0.002); Varus motion was 7.7º ± 2.5 unsupported vs. 5.6º ± 2.2 supported, which was 74.3 ± 44.2%, (not significant).
DISCUSSION
The data obtained through this study, supports our hypothesis that the UCBL/articulated ankle AFO significantly limits subtalar joint/ hindfoot motion thus prohibiting further valgus stress and possible additional injury to the dysfunctional posterior tibial tendon in a surgically induced (Stage 11 PTTD). Moreover, this brace allows free ankle motion and increased functional stability to the pathological tendon in stage II PTTD while maintaining active dorsiflexion/plantarflexion of the ankle joint which significantly enhances the patient’s ability to independently ambulate. The concept of functional bracing allows the tendon to rest without allowing the hindfoot (calcaneus and subtalar joint) to excessively pronate thus placing further valgus stress, pathological stretching, and potential increased injury/tearing/rupture to the posterior tibial tendon. The posterior tibial tendon is allowed normal function without reaching a pathological position i.e. maximum hindfoot valgus or excessive subtalar joint pronation which could promote further tearing of the tendon in a most commonly longitudinal direction. An important difference in this brace and a solid custom molded AFO (e.g. the Arizona brace) is the ability of the UCBL/AFO articulated ankle to maintain “free” ankle dorsiflexion and plantarflexion while concurrently bracing the dysfunctional posterior tibial tendon in a position of comfortable function. The normal physiological balance of the tendons crossing the ankle joint is protected from excessive pronation and supination forces. A more normal hindfoot to midfoot and forefoot relationship is maintained. Normal ambulation without additional assistive devices such as canes and or walkers/wheelchairs is usually avoided. In vivo testing in live patients with PTTD utilizing the UCBL articulated ankle AFO with real time computer assisted gait analysis would be an area of further research and interest. Furthermore, a comparison cost analysis of the conservative functional bracing as presented here versus surgical intervention with respect to loss of time from work and rehabilitation to full recovery which can be extensive, would be an area of further research with the goal of cost effective therapy in today’s managed care environment.
Our data concludes with computer assisted analysis that the UCBL with AFO articulated ankle custom molded is a functional brace that effectively controls the pathological motion, hindfoot valgus or pronation that occurs in the subtalar joint/hindfoot complex when there is a partial rupture surgically created stage 11, of the posterior tibial tendon in a cadaveric specimen. This conservative treatment concept is a refinement of the principles proposed by Frey and Shereff, Myerson and Mann. Perhaps studies in a similar model could be used to directly compare other devices to the UCBL/AFO, for example: the Richie brace, Arizona brace (solid AFO) and MAFO (Maryland custom molded ankle-foot orthosis) as well as other solid AFO’S, casts and CAM walkers.
Limitations of the study are the small sample size. But the effects measured were so dramatic, that with the help of internal controls, there was statistical significance to the control of hindfoot valgus, the most important variable. Another limitation is that the cadaver limbs are less flexible than live subjects with regards to tissue laxity of the ankle and sutalar joint range of motion. Also, to the authors’ knowledge, no one has measured live subjects with Stage II PTTD to assess the extent of motion compared to normal ankles. There is no information currently available to validate our model of Stage II PTTD. The appearance of the PTTD pathology in clinical patients as visualized on MRI compared to the appearance of the simulated pathological tear along with the judgment of the surgeon (ACB) in this study was the only subjective validation of our model. It is the hope of the authors that clinical application of this conservative functional bracing as described will help those clinicians treating this disabling condition provides a conservative non-operative management of those patients who present as poor risks for surgical management.