Reconstructive Surgical Treatment of Post Burn Trophic Wounds of the Plantar Surface in Foot Burns
- 1. Burn department of RSCUMA, Samarkand State Medical Institute, Uzbekistan
Abstract
Burns to the feet can cause significant morbidity, pain and difficulty in walking due to the location of injury and the specialized anatomy of skin on the sole of the foot. Skin on the sole of the foot is highly specialized and is difficult to reconstruct after a severe burn injury. The method of closure should be chosen according to both severity and localization of the injury, using local uninjured tissues and soft scars to make shaped flaps and free grafts placed on the area of the excised scars. The grafts were viable, sensibility was preserved and no marginal necrosis was noticed. Patients can take up their work by 1.5–2.0 months after surgery.
Keywords
• Post burns
• Surgery
• Wound
• Foot
Citation
Shakirov BM (2017) Reconstructive Surgical Treatment of Post Burn Trophic Wounds of the Plantar Surface in Foot Burns. JSM Foot Ankle 2(1): 1022
INTRODUCTION
Although the feet involve only a small percentage of the total body surface area (3.5 %), they play an important role in daily life because of their motion and weight-bearing function. Burns to the feet can cause significant morbidity, pain and difficulty in walking due to the location of injury and the specialized anatomy of skin on the sole of the foot [1-5]. Glabrous skin on the sole of the foot is highly specialized and is difficult to reconstruct after a severe burn injury. It has a thicker epidermis, a compact, less elastic dermis and is cushioned with a fat pad. This makes it more durable and able to withstand force, pressure and shearing.
MATERIAL AND METHODS
A total of 21 patients have been under our observation at Samarkand Inter-Regional Burn Center, Uzbekistan, for prolonged trophic wounds of soft tissues of the plantar surface of the foot, one or another method of reconstructive surgery are planned.
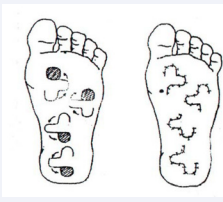
Therefore, after elimination of the limited surface defects of the plantar surface located in the area of central loading of the foot (heel), we performed bilobed skin flat flaps pasties in ten patients. The significance of bilobed skin-flap plasty is to use the most appropriate local tissues to fill the defects in the supporting foot area; these are the tissues of the supporting foot area. This method allows dissipating the tension of tissues when closing the donor wound in a large area remote from the center of the defect. This results in complete recovery of the skin, resistant to exertion, and without atrophy or newly formed scars (Figure 1).
Figure 1: Scheme before and after the operation.
In deep wounds penetrating to the calcaneum, thickness of cutaneous flaps is insufficient for complete recovery of tissues defect and formation of supportive surface. In deep defects reaching the heel bone in two patients, we performed a combined plasty – a muscular one in combination with transfer of the skin fat flap or a free skin graft.
When placing the scars in the heel area and in distal part of the plantar surface directly on the bone, we used tube grafts in five cases. The Filatov and gluteal-femoral graft method of plastic surgery by tube grafts is to transfer tissues on the sole.
In plastic surgery by a flat Filatov graft at the first stage, the skin-fat bond is cut out with preservation of both hands. The donor wound is sutured and the tube wound is closed by split skin. After 20-25 days later the distal hand is cut off, the tubed graft is flattened by longitudinal incision on the transplant, maintaining a uniform thickness not less than 1 cm. With this thickness of the tubed graft, the scars are excised in the area of the hand and the last is wrapped by the tubed graft after connecting the posterior surface. After stable living (3-4 weeks), the proximal hand is cut off, the remainder of the tubed graft is flattened, the scars are in sected on the posterior surface of the sole and plastic surgery is completed. In observations, a good result was achieved and no complications were noted. The grafts were viable, sensibility was preserved and no marginal necrosis was noticed (Figure 2).
Figure 2: Plastics of Filatov graft
In calcaneal area defect reconstruction of the heel soft tissues on the supportive side of the foot by a medial calf flap of the opposite leg used to bear the load, in four cases we have performed two-stage reconstruction of the heel soft tissues by medial calf flap of the opposite leg.
RESULTS
We observed a good result with no complications. The grafts were viable, sensibility was preserved and no marginal necrosis was noticed. Gradually the operation efficacy improved as the cicatrices became softer. In only one patient, a marginal necrosis was noted and the necrotised area was removed and the wound was closed by split skin without influencing the good result of the operation.
CONCLUSION
Burns to the feet can have major effects in daily life, caused by prolonged bed rest, hospitalization and high risk of both early and late complications. Treatment of defects of the plantar surface of the foot due to contact burns (sandal burns) is a difficult problem since there is always a lack of soft tissue, suitable for plasties in this area [6-8].
Wounds are located mainly on the supportive surfaces above the heel bone and the heads of metatarsal bones. They can be widespread, occupying also the lateral and posterior surfaces. The skin around the wound and non-bearing surface of the foot can be healthy. Therapeutic gymnastics begins after assessment of the patient’s condition by the physician – rehabilitator the day after surgery. The main goal of physical exercises is rehabilitation of the foot function. In development of superficial abrasions on the flap, the patients were recommended to rest during 5-7 days and as a rule, the wounds epithelised themselves after that period. Patients can go to work in 1.5 months after the operation, but full adaptation of the flap and its good engraftment occurs at 2 - 3 months.