The Efficacy of Prophylactic Single Dose Intravenous Antibiotics vs. Multi Dose Intravenous or Oral Antibiotics in Elective Foot and Ankle Surgery
- 1. Department of Orthopedic Surgery, Tel Aviv University, Israel
Abstract
A prospective evaluation of wound healing of 675 patients who underwent elective foot and ankle surgeries between 2011 and 2015 at a single hospital clinic was performed to evaluate the effect of two prophylactic antibiotic regimens. Only those patients who were having elective foot or ankle surgery and were being followed up at the hospital’s outpatient clinic, patients had a traumatic or non-traumatic cause for their surgery. The ASEPSIS classification system was used to define wound healing with a grade of more than 20 considered an infection. Two hundred and twenty patients (32.6%) patients received a single dose preoperative antibiotic and 455 (67.4%) patients received a prolonged prophylactic treatment. Of the 455 patients who received a prolonged antibiotic treatment, 444 had unimpaired healing (97.8%), 3 had impaired healing and the rest (8 patients, 1.5%) had postoperative infections. Among the single dose antibiotic group, 181 (82.7%) had normal healing, 24 (10.9%) had impaired healing and 15 (6.8%) had an infection. The intergroup difference was significant (ANOVA, p<0.001). The results suggest that prophylactic intravenous antibiotic use combined with post-operative treatment in routine elective foot and ankle surgery might be expected to reduce the complication rates and impaired wound healing.
Keywords
• Prophylactic antibiotics
• Foot and ankle surgery
• Wound infections
• Impaired wound healing
Citation
Yassin M, Garti A, Heller E, Robinson D (2016) The Efficacy of Prophylactic Single Dose Intravenous Antibiotics vs. Multi Dose Intravenous/ Oral Antibiotics in Elective Foot and Ankle Surgery. JSM Foot Ankle 1(3): 1017.
INTRODUCTION
There is a controversy regarding the appropriateness of single dose pre-operative antibiotics in foot and ankle surgery though it is well documented that skin preparation does not eliminate surgical site bacteria in most elective foot operations [1]. More than 70 percent of patients have a positive culture at the hallux following skin preparation, and even at the ankle more than 15 percent is contaminated after skin preparation [1]. Some studies indicate that preoperative antibiotics have a positive effect on the prevention of postoperative wound infections in certain high risk foot procedures [2], while other studies failed to indicate an advantage for antibiotic prophylaxis [3]. Especially in diabetic patients the organisms tend to be resistant to cefalosporins, perhaps explaining some of the increased infection risk in that group. A recent task force of the American College of Foot and Ankle Surgeons stopped short of clear cut recommendations regarding antibiotic prophylaxis in elective foot surgery [4], though suggesting that antibiotic prophylaxis routine prophylaxis will likely be continued at most institutions, because few complications have been reported with the practice.
Although the incidence of postoperative wound infection is low in elective orthopaedic surgery, if an infection does occur, the final outcome can lead to unfortunate consequences. The incidence of infection rate in clean orthopaedic surgery is between 0.5% to 9.2% [5,6], depending on the author and procedure. Apparently the higher range of infection rates occur in foot surgery possibly due to operative site contamination that appears to be very common in foot surgery [1].
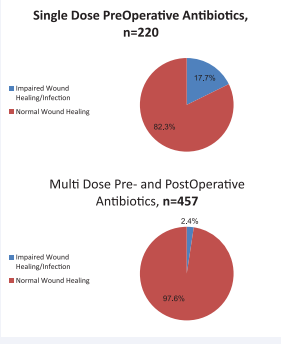
A drawback of antibiotic prophylaxis might be the generation of highly antibiotic resistant bacteria and thus routine antibiotic surgery in low infection risk patients has been questioned [7,8]. However most foot surgeries are not low-risk as a large proportion of patients are diabetic, elderly or with some degree of circulatory deficiency. In addition, there is a significant risk of contamination by multi-drug-resistant bacteria of surgical scrubs [7] that might indicate a risk of contamination by the medical team rather than bactermia that appears to be rare in foot surgery [9] (Figure 1).
Figure 1: The percentage of patients acquiring a wound infection by type of antibiotic regimen used. Note the percentage of patients having impaired wound healing or having an infection was significantly higher in the single dose preoperative antibiotic group than in the prolonged multi dose antibiotic treatment group
MATERIALS AND METHODS
A prospective wound evaluation of 675 patients receiving elective foot and ankle surgeries 2011 and 2015 at a single hospital clinic was performed to evaluate the effect of two prophylactic antibiotic regimens by one of the authors (D.R.). All patients had a preoperative evaluation by one of the foot and ankle surgeons (n = 2) at the outpatient clinic of the hospital. The evaluation consisted of a history and physical examination, preoperative foot radiographs, and laboratory studies when indicated. All surgeries were performed by the both surgeons who performed the preoperative evaluation.
GROUP DESIGNATION
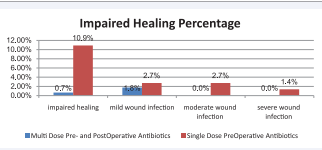
The series represents a sequential series of patients operated by both surgeons and followed up in the hospital outpatient clinic. Up to May 2013 patients were treated by single dose preoperative antibiotics. From May 2013 onward, due to a change in departmental policy due to an impression of a high wound complication rate, a multi-dose antibiotic treatment regimen was used. Patients were excluded from the series if they had a prior history of open wounds, infection, or open fractures of the foot or ankle. All patients were followed up postoperatively at the hospital’s outpatient clinic by one of the authors. Postoperative care included physical examination, wound inspection, foot radiographs on a routine basis with laboratory work-up reserved for cases of postoperative infection and/or complications (Figure 2).
Figure 2: Distribution of ASEPSIS wound score by type of antibiotic regimen used. It appears that the major groups that are improved by the prolonged antibiotic treatment regimen are the impaired wound healing group as well as the moderate to severe infection groups.
CLASSIFICATION OF OPERATIVE PROCEDURE
It was assumed that closed and endoscopic surgery might be associated with less infection risk, and that longer hindfoot procedures might carry a higher risk of infection than forefoot surgeries. Thus, the 675 charts were divided into several surgical categories to include forefoot surgery with implants and without implants as well as percutaneous forefoot surgery. Mid foot surgery either open or closed and hindfoot surgery again divided between closed percutaneous approaches and open surgeries. A last category was endoscopic surgery at all foot regions. Patients who had more than 1 procedure performed at the time of their surgery (eg, first metatarsal osteotomy and correction of hammertoes) were assigned according to the procedure that was of the presumed higher risk category. Both groups had similar proportion of endoscopic cases (about 20%). The multi-dose group had a higher percentage of high risk procedures (open hind-foot 21%) than the single dose group (11%, Wilcoxon-Rank test, p<0.03).
DATA EXTRACTION
From the patient charts, the following data were extracted: prophylactic antibiotic use, age, gender, presence of diabetes (defined as either fasting blood glucose higher than 125 mg/dl or an A1C level of 6.5 percent or higher), and use of implants. Additionally, the ASEPSIS wound healing score [10] was available for analysis.
SURGICAL TECHNIQUE AND FOLLOW-UP PROCEDURE
All patients undergoing foot and ankle surgeries were scrubbed and draped in the same manner according to the hospital’s policy. Skin preparation included scrubbing twice with chlorhexidine gluconate (Septal Scrub, Teva Medical Ltd, Israel), drying with a sterile towel, and painting twice with Chlordhexidine Alcohol solution (Chlorhexidine gluconate 0.5%W/, Isopropanolol 70% V/V, Teva Medical Ltd, Israel). Preoperative prophylactic intravenous antibiotics were administered 30-60 minutes before skin-cut for all patients. Cefazolin sodium 1 gram (Cefamezin 1 gram, Teva Medical Ltd. Israel) was administered for all patients without a known allergy to penicillin. In 67 patients with previous history of penicillin allergy, clindamicin 300 mg IV (Dalacin-C, Teva Medical Ltd., Israel) was administered. Post- operative treatment depended on time of discharge and known penicillin allergies. According to department policy, patients were discharged if they were discharged from recovery at 13:00 or earlier, Patients operated later in the day were hospitalized overnight. Routine post-operative treatment included intravenous cefazolin sodium 1 gram (Cefamezin 1 gram, Teva Medical Ltd. Israel), every eight hours for 24 hours for patients hospitalized overnight (128 patients) followed by amoxicillin trihydrate 875 mg / potasium clavulanic acid 125 mg (Smithkline Beecham Plc, UK) twice a day for one week. Patients who were same-day discharged were treated by oral augmenting alone. Penicillin-allergic patients were treated by oral clindamycin 600 mg twice a day for one week.
Postoperative follow-up was performed at the outpatient clinic at one week post operative, two weeks post operative and six weeks postoperative. The ASEPSIS score was graded at every visit and the worse score recorded was used in the current analysis.
DATA ANALYSIS
The data obtained from the clinical follow-up and chart reviews of each patient were grouped according to whether or not single dose preoperative antibiotics were administered or a combination of preoperative antibiotics and postoperative treatment. Descriptive statistics consisting of means and standard deviations for the quantitative data were then obtained.
Frequencies for the categorical data were calculated for each of the study groups. t tests were conducted to determine if any differences existed between the 2 study groups with respect to their mean age, gender or the presence of diabetes. Additionally, chi-square tests of association were performed to determine if the antibiotic regimen used was associated with any of the study factors (gender, metal fixation use, surgical category, and presence of diabetes). All statistical testing was conducted by using the Analyze-it software package (version 2.30, Excel 12+).
RESULTS
A total of 675 charts were reviewed; Two hundred and twenty patients (32.6%) patients received a single dose preoperative antibiotic until a change in departmental policy took place. Since then455 (67.4%) patients received a prolonged multi dose prophylactic treatment (Table 1).
Table 1: Patient Demographics. |
||
|
Parameter |
Single Pre-Operative Dose |
Multiple Post-Operative Treatment |
|
Number of Subjects |
220 |
455 |
|
Females |
131 (39.6%) |
275 (60.4%) |
|
Males |
89 (40.4%) |
180 (59.5%) |
|
Age Average ±SD (Range) |
41±19 (18-92) |
44±22 (18-89) |
|
Diabetes |
65 (29.5%) |
141 (31%) |
|
Procedure Classification |
||
|
Forefoot Percutaneous |
20 (9%) |
67 (15%) |
|
Forefoot With Implants |
66 (30%) |
107 (24%) |
|
Forefoot Open No Implants |
46 (21%) |
46 (10%) |
|
Mid Foot Open |
11 (5%) |
24 (5%) |
|
Mid Foot Closed |
0 |
12 (3%) |
|
Hindfoot Open |
24 (11%) |
95 (21%) |
|
Hindfoot Closed |
7 (3%) |
21 (5%) |
|
Arthroscopic |
46 (21%) |
83 (18%) |
The distribution of the type of the procedures was not similar in both groups (Kruskal-Wallis test, chi-square 5.68, p<0.02) with more open forefoot procedures without implants in the single antibiotic group and more open hindfoot procedures in the multiple antibiotic group (Table 1).
Administration of single dose antibiotic was associated with higher impaired healing rates in patients with implants as well as in patients without implants as compared to multiple dose antibiotic treatement (Kruskal-Wallis’ statistic 108.8, p<0.001).
ASEPSIS score was significantly higher in the single dose preoperative antibiotics group (5.4 ± 9.2) versus the multiple dose antibiotic treatment groups (0.83 ± 3.7).
Of the 455 patients who received a prolonged antibiotic treatment, 444 had unimpaired healing (97.8%), 3 had impaired healing and the rest (8 patients, 1.5%) had postoperative infections. Among the single dose antibiotic group, 181 (82.7%) had normal healing, 24 (10.9%) had impaired healing and 15 (6.8%) had an infection (Table 2).
Table 2: Healing of Surgical Incisions by Type of Antibiotic Treatment. |
|||
|
Healing Grading |
ASEPSIS Score |
Single Pre-Operative Dose (%) |
Multiple Post-Operative Treatment (%) |
|
satisfactory healing |
0-10 |
181 (82.3%) |
444 (97.6%) |
|
impaired healing |
11-20 |
24 (10.9%) |
3 (0.6%) |
|
mild wound infection |
21-30 |
6 (2.7%) |
8 (1.7%) |
|
moderate wound infection |
31-40 |
6 (2.7%) |
0 (0%) |
|
severe wound infection |
>40 |
3 (1.3%) |
0 (0%) |
|
Total |
220 (100%) |
455 (100%) |
|
The overall intergroup difference was significant (ANOVA, p<0.001). Most intergroup difference was in the impaired healing group.
Preoperative single dose antibiotic use was associated (P <0.01) with postoperative impaired wound healing and infection in a post-hoc analysis of the entire cohort. Overall, diabetic patients had higher ASEPSIS scores (3.7 ± 9) than non-diabetic patients (1.7 ± 4.7) and the difference was significant (ANOVA, F=14.5, p<0.001). Diabetic patients in the single antibiotic dose group had a significantly worse ASEPSIS score (8.4 ± 12.6) than non-diabetic patients (4.2 ± 6.9, ANOVA, F-Statistic 37.7, p<0.001), but ASEPSIS scores were similar in the multiple antibiotic dose group (Table 3).
Table 3: The effect on antibiotic regimen on the ASEPSIS score by presence of diabetes.
|
ASEPSIS SCORE by diabetes and antibiotics |
Number of Cases |
Mean ± SD |
|
single & no diabetes |
155 |
4.2±6.9 |
|
single & diabetes |
65 |
8.4±12.8 |
|
multiple & no diabetes |
314 |
0.5±2.7 |
|
multiple & diabetes |
141 |
1.6±5.3 |
|
Source of variation |
Sum squares |
DF |
Mean square |
F statistic |
p |
|
Diabetes And Antibiotics |
4041.2 |
3 |
1347.1 |
37.68 |
<0.0001 |
|
Single & No Diabetes V Single & Diabetes |
-4.2 |
-6.5 |
to -1.9 |
(significant) |
|
|
Single & No Diabetes V Multiple & No Diabetes |
3.7 |
2.2 |
to 5.2 |
(significant) |
|
|
Single & No Diabetes V Multiple & Diabetes |
2.6 |
0.8 |
to 4.4 |
(significant) |
|
|
Single & Diabetes V Multiple & No Diabetes |
7.9 |
5.8 |
to 10.0 |
(significant) |
|
|
Single &Diabetes V Multiple &Diabetes |
6.8 |
4.5 |
to 9.1 |
(significant) |
|
|
Multiple & No Diabetes V Multiple & Diabetes |
-1.1 |
-2.7 |
to 0.5 |
Use of implants was not associated with increased rates of impaired wound healing (2.0 ± 6.1) as compared to operations without implants use (2.3 ± 6.7, ANOVA F-statistic 1.82, p>0.17). ASEPSIS score correlation to other factors was calculated. There was a negative correlation (r=-0.33) with the antibiotic regimen, as well as arthroscopic and closed procedures (r=-0.22), and positively correlated with the presence of diabetes (r=0.15)
A total of 14/675 patients required formal wound revision in an operative room setting. 3/455 in the multiple dose group versus 11/220 in the single dose group (the difference is significant with p<0.001 Wilcoxon-Mann-Whitney test). The odds ratio of the need for revision in the multiple antibiotic dose group compared with the standardly used single dose was 0.12 with the Miettinen-Nurminen 95% Confidence Interval at 0.037-0.47). Multivariate analysis was employed to assess the possible interaction effect of the need for wound revision with the presence of diabetes, antibiotic treatment and the presence of implants. Pearson’s r was calculated using Fisher’s z method at the 90% confidence interval level. The only significant factor appeared to be the presence of implants and the type to antibiotic treatment (r=0.07, p<0.05).
DISCUSSION
Surgical infection is an important and deleterious complication of foot and ankle surgery. It is particularly common in cases of implant removal where a up to ten percent infection rate can be expected [11]. The high frequency of surgical site infections (SSI) combined with the large number of foot and ankle procedures performed creates a major healthcare and financial burden. Unfortunately limited data is available regarding optimal strategies of decreasing SSI’s in foot and ankle surgery. The optimal surgical preoperative cleaning regimen is not well defined and there is only weak evidence that the type of surgical scrub and anti-sepsis solution used affects surgical infection rates [12]. The importance of pre-operative antibiotics in foot and ankle surgery is not well established either, and there is some controversy regarding optimal prophylactic agent choice [13]. The study results seem to indicate that the type of antibiotic prophylaxis affects the frequency of impaired wound healing and infection in clean foot and ankle surgery. In our specific institute the rate of diabetes mellitus is high, a disease that has been associated with almost doubling of complication rates [14]. Due to high infection rate, a new concept was developed, assuming that the foot and ankle surgical case is clean-contaminated and treating with a full antibiotic course instead of prophylactic treatment as is commonly use. This study is unique in the approach of treating the supposedly clean surgical patient as potentially infected and treating the patient pre-incision and for a week after operation. The concept is due to the relatively high frequency of infection and impaired wound healing in clean foot surgery [5]. Following anti-septic surgical field preparation the majority of toes are still colonized by potentially pathogenic bacteria [1]..
Traditionally, studies investigating antibiotic prophylaxis in foot and ankle surgery compared frequency of infection between groups with and without antibiotic prophylaxis [15] and failed to show a clear cut advantage. Other studies have not shown an advantage of one antibiotic over the other [16]. However these studies have not used the ASEPSIS score [10] as an endpoint. The advantage of this score is that it is sensitive enough to define a group with impaired wound healing and allows diagnosis of three times as many clinically infected wounds as evaluations based on the presence of pus alone [17]. In additions the ASEPSIS score appears to correlate quite well with the definitions of the Center for Disease Control [18]. A few studies have looked at multi dose versus single dose treatment especially in trauma settings and seem to indicate that a single dose is equivalent to multi dose therapy in open tibial fractures [19]. The population treated in the current study is very different than the one treated by the open tibial fracture study. The definition of infection in the Patzak is study was presence of fever, erythema, wound discharge and positive wound culture [19]. This definition would exclude many cases of impaired wound healing as defined by the ASEPSIS criteria and tend to underestimate the frequency of impaired wound healing. On the one hand the risk of infection is apparently higher as in this group of open tibia fractures, the patients were younger (average age 33 years in the cephalosporin group). Another major difference in the treated population of the current study is the high prevalence of diabetes at our institute, while the Patzak is study does not mention the frequency of diabetes in their population, the prevalence in the current study population is very high and the advantage of the multidose therapy appears to be in reducing the rate of impaired wound healing subjects with ASEPSIS scores of 10 to 20 and reducing the excess risk of infection in diabetic patients. Thus, it is possible that the results in open tibial fractures do not reflect the optimal treatment regimen in elective foot and ankle surgery.
In order to define the potential clinical significance of reduction in the number of these impaired wound healing cases, an analysis of the need for wound revision was carried out. Confirming the preliminary study hypothesis, multi-dose antibiotic therapy was found to decrease the number of formal wound revisions. This finding might tip the balance in favor of multi dose antibiotic treatment as this might offset the increased cost of secondary surgery.
The current study has the advantage of being a consecutive series of cases performed by a single surgical team using the same techniques. As in any single center study, there is a legitimate concern whether the results can be generalized to other localities and centers. Another disadvantage of the current study is the lack of randomization. While RCT remain the gold-standard of clinical trials, their cost is quite prohibitive. Also there is a definite advantage to a ‘real world’ consecutive series of patients, as compared to the bias often introduced by sophisticated inclusion\exclusion criteria, making generalization to the general population difficult.
In conclusion, it appears reasonable to conclude that due to the high risk of skin contamination in foot and ankle surgery even after surgical skin preparation reported to vary between 20-75% depending on exact protocol, the surgery should be considered clean-contaminated and wound healing and infection rates can be reduced by prophylactic administration of a one week long multi dose antibiotic treatment.