Jackhammer Esophagus - Symptom or Diagnosis? Review
- 1. Medical Center for Rehabilitation and Geriatrics, Israel
Citation
Levin M (2023) Jackhammer Esophagus - Symptom or Diagnosis? Review. JSM Gastroenterol Hepatol 10(1): 1118.
INTRODUCTION
Jackhammer esophagus (JE) is relatively rare disease. The confusion in this matter begins with the definition. Is JE a manometric characteristic (symptom) or a diagnosis? In a review by Triggs and Pandolfino, although JE is called a disease, it is also seen in gastroesophageal reflux disease (GERD) and eosinophilic esophagitis (EoE). “Jackhammer esophagus is diagnosed on the basis of two swallows with a DCI value above 8000 mm Hg*s*cm, is a very heterogeneous classification. Meeting these criteria, however, is not enough evidence to refer patients for invasive treatments. This pattern can be associated with obstruction at the EGJ and is also seen in the context of gastroesophageal reflux disease (GERD) and EoE. Given this heterogeneity, further workup focused on ruling out an obstruction and empiric trials with smooth muscle relaxants should precede referral for myotomy. Many patients with diagnosed jackhammer esophagus will have a benign course, especially when this pattern is found incidentally during a pre-operative workup for GERD and thus observation and follow-up may also be reasonable” [1].
Thus, JE describes the manometric characteristics in different parts of the esophagus.
Analysis of “High Resolution Manometry”
High resolution manometry (HRM) was developed with the large methodological flaws.
(?) The decisions of the Chicago Classification version 4 (CCv4.0) about esophageal HRM have nothing to do with science, as they were taken by vote. «Co-chairs and sub-group members were tasked with developing statements to define a conclusive diagnosis of the motility disorder assigned to their sub-group. These statements were based on literature review and expert consensus. After two rounds of independent electronic voting thee statements were considered appropriate when meeting ≥80%agreement and are included in the final CCv4.0» [2].
(b) The selection of the norm was made based on the absence of painful symptoms according to the examined person [3]. This is a gross mistake, since it is known that GERD can occur without clinical manifestations in almost 30% of patients [4,5]. An example of such an error that led to unjustified conclusions is the example from Kwiatek et al. (Figure 1) [3].
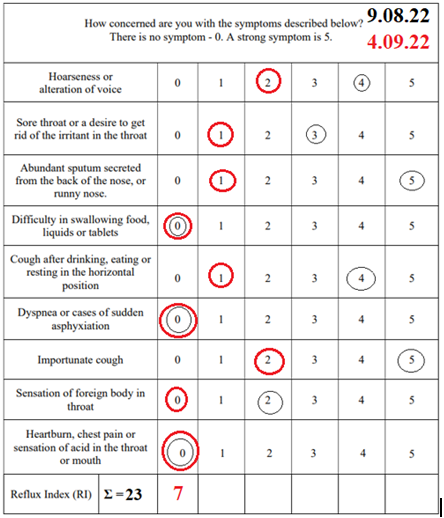
Table 1: Questionnaire foe the screening of gastroesophageal reflux disease.
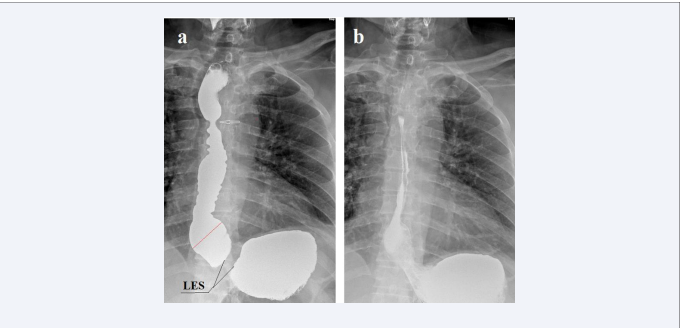
Figure 1: Simultaneous X-ray study with HRM of a person from the control group from article by Kwiatek et al [3]. Formation of a phrenic ampulla is shown, which is closed proximally by the contractile deceleration point (CDP) to create high pressure, open the LES, and inject a bolus into the stomach. This contraction zone is shown on the HRM. The authors argue that the endoclip, attached to the squamocolumnar junction (SCJ), shifted cranially during the emptying of the ampulla, which allegedly confirms the idea of shortening the esophagus. In fact, the endoclip has not shifted. In both images, it is located to the left of the lower angle of the 10th thoracic vertebra. But the distance between the stomach and the clip somewhat decreased because of the opening of the intra-abdominal part of the LES. In both images, the length of the LES is shorter than the norm (1.5 vs. 3.6 cm). {the height of the 10-thoracic vertebra (red line) is about 2 cm long}.
The presence of an ampulla and a sharp shortening of the LES indicates GERD. As a result of the erroneous selection of individuals in the control group, the authors took the shortening of the LES, due to its weakness, as a shortening of the esophagus.
(?) “The key HRM metrics utilized in the CCv4.0 consist of assessment of deglutitive relaxation across the LES/EGJ using integrated relaxation pressure (IRP), vigor of esophageal body contraction using distal contractile integral (DCI), contractile wavefront integrity at 20 mmHg isobaric contour setting, and latency of deglutitive inhibition using distal latency (DL)” [2]. These characteristics of the manometric graph have no physiological meaning. They were suggested by the engineers of the manufacturer’s company, who tried to determine the difference in relation to the norm. But the control persons were selected erroneously.
(d) The confidence of the new method is checked when comparing it to the results with the previously applied methods. Before the introduction of HPM, diagnostics was carried out by the X-ray method. However, comparative studies of HRM with X-ray examination were not carried out.
Manometric Characteristics are not a Diagnosis
It is obvious that the results of HRM are a manometric characteristic of the disease, which led to a sharp change in pressure. The review authors clearly indicate that GERD is the cause of JE, i.e., a disease that leads to abnormal pressure in the esophagus. This definition is fundamental, since it is not a symptom that needs to be treated, but a disease - not an increase in pressure in the esophagus, but an inflammatory process, because of which it rises. Early acid perfusion studies have demonstrated the ability of acid to induce esophageal spasms, suggesting a role for GERD in the pathogenesis of JE [6,7]. Also in JE patients, a high incidence of GERD was found, and it was shown that hypertensive peristalsis has been shown to improve with suppression of gastric acid [6,8,9].
Woo et al decided to test if pathologic acid exposure is associated with JE. They retrospectively compared the results of the examination (HRM and pH monitoring) of JE patients with the control group, which included “patients” defined as symptomatic patients with normal manometries (no disorders of EGJ outflow obstruction, major or minor disorders of peristalsis)” [10]. Statistical analysis showed that between groups “There were no differences seen in any other acid reflux parameters” [10]. From this, the authors concluded: “Pathologic acid exposure does not appear to be associated with JE [10].These two findings contradict the material of Woo et al. In comparing the two groups, they ignored diagnoses.
Article Analysis
The two groups of patients differed from each other only in the manometric index (DCI value was < or > 8000 mm Hg*s*cm). All (100%) patients with JE had typical symptoms of GERD. All control patients had gastroesophageal reflux. Since pH monitoring only diagnoses very severe forms of GERD, in a significant percentage of patients with GER, reflux is considered physiological, which is contrary to common sense, since the border of pH monitoring was worked out on patients without clinical symptoms. There is no doubt that the control group consisted of patients with GERD. Thus, the absence of differences between the two groups suggests that patients with JE manometric symptom had GERD. To draw a correct conclusion, it was only necessary to correctly diagnose the symptomatic patients selected for the control group. The analysis of the peer-reviewed article convincingly proves that:
1. The JE manometric symptom is the result of GERD.
2. pH monitoring should be excluded from both scientific and practical research.
3. Treatment should be directed to the disease (GERD) and not to the manometric symptoms.
Jackhammer Esophagus in x-ray image
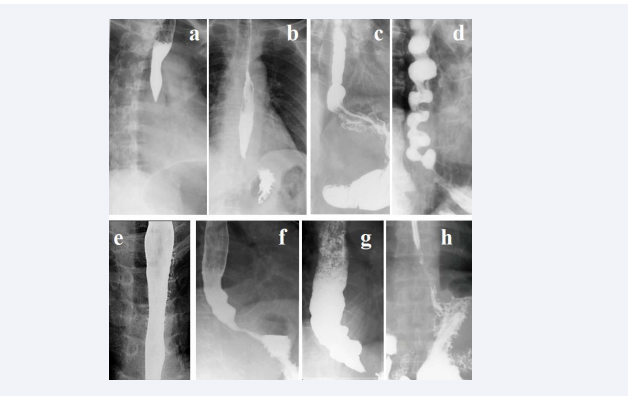
I found 7 radiographs in the articles about JE (Figure 2).
Figure 2: Radiographs of patients with GERD, with JE manometric symptom. In all cases, there were typical clinical symptoms and radiological signs of GERD. Erupted esophagitis was caused by spasm at the level of anatomical narrowing of the esophagus caused by aortic arch pressure on radiographs (a,b,c). A significant shortening of the LES relative to the norm is determined on radiographs (b, d, f, g, h). Esophageal dilatation with LES deformity caused by peptic stenosis is seen on radiographs (f,g). Signs of severe esophagitis are seen on radiographs (d,e).
Below is a detailed analysis of the case presented in Figure 1.a.
Case 1. From Choi et al [11]. A 53-year-old woman hadodynophagia and regurgitation. The final diagnosis ????? HRM was medication refractory (no information about treatment) Jackhammer esophagus without involvement of LES. The patient underwent HRM-guided superficial partial circular muscle myotomy. After the procedure, the patient’s symptoms dramatically improved and post-POEM HRM was within the normal range. During a 1-year follow-up period, patient was in good health and remained symptom free.
Odynophagia is due to esophagitis, which could be seen on gastroscopy (not done) and barium passage distal to the spasm (No).
This operation was meaningless, firstly, because the spasm is a transient condition, especially after pathogenetic treatment. Second, the muscle was cut 5 cm proximal to the spasm (Figure 2). Therefore, relief of symptoms is unlikely to be due to muscle dissection.
Below is a similar case of GERD from my practice. A 72-year-old man had with complaints of a debilitating cough, a change in voice, and a feeling of a foreign body in the throat for 4 months. Very rarely, small pieces of food appear in the mouth. Within a month, he wakes up at night, as he chokes on saliva. He does not feel any acid or bitterness in his mouth. He has not heartburn, pain, or dysphagia. He noted the symptoms in detail in the questionnaire (Table 1). About 15 years ago he had heartburn and chest pressure. PPI treatment did not bring relief. The symptoms disappeared immediately after he swallowed contrast tablet with diameter 3 cm. Since then, he felt healthy, did not go to the doctors, did not take any treatment, and did not follow any dietary restrictions. In the table 1, the patient rated the severity of symptoms before treatment with a black circle and 25 days later with a red one.
X-ray examination of the esophagus, upper (UES) and lower esophageal sphincter (LES)
This method is based on the physiology of the esophagus and the esophageal sphincters. It is known that a significant increase in gastric pressure causes a reduction in both UES and LES [12,13]. Secondly, an increase in the tone of the LES causes a slowdown in the rate of esophageal peristalsis [13].
METHOD
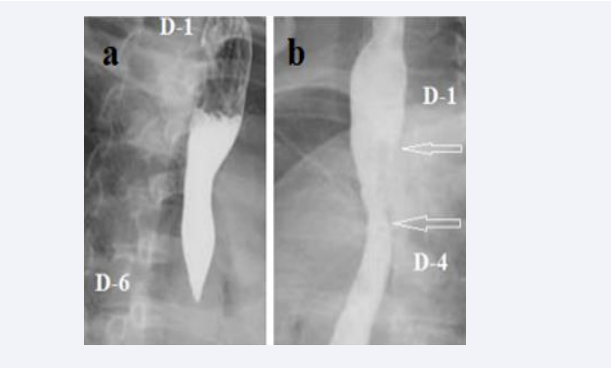
There is no restriction on pre-study meals. The patient lies on the X-ray table. Near his head is a jar with 200 ml of barium suspension. The patient drinks barium without interruption, and when the barium runs out, he lifts his straightened legs high. At this point, the first radiograph is taken (Figure 4 a).
Figure 4: a. High pressure in the stomach led to a reflex contraction of the UES and LES. Tight filling of the esophagus between the UES and LES is determined. LES is significantly shorter than normal (1.7 cm versus 3.6 cm).The phrenic ampulla (red line) is sharply dilated (4.4 cm versus 1.5 cm in normal). The walls of the esophagus are uneven with asymmetric waviness. At level D-4, a symmetrical constriction 6 mm wide with smooth contours is determined (arrow). Barium lodged in the hypopharynx is visible at the very top of the x-ray. The patient swallowed a 1.9 cm tablet, which passed into the stomach immediately, which confirmed the absence of stenosis. Spasm of the esophagus at the border of the upper and middle thirds indicates a high tone, i.e., high intraluminal pressure. b. After 5 minutes, at the rest, a spontaneous reflux of barium from the stomach into the esophagus is seen with a wide opening of the EGJ. The proximal sphincter, which most often closes the ampulla proximally, does not function in this case (on both images). Uneven longitudinal folds visible in the esophagus. But the barium didn’t go above D-4 where there was constriction in the first radiograph. I believe that this is a functional sphincter that prevents acid from refluxing into the proximal esophagus. At this x-ray also seen barium stuck in the hypopharynx.
The patient gets up and lies down again after 5 minutes. At this moment, a second radiograph is taken at rest (Figure 4 b). Conclusion GERD with severe esophagitis. Pharyngitis.
The patient reported by phone that from the first night after taking the tablet, he did not get up at night and did not choke on saliva as before. The otolaryngologist found an inflammatory process in his pharynx and upper esophagus and prescribed an (3.6 cm), since its abdominal part opens in the stomach [3,4]. Thirdly, free reflux is visible in the second picture (Figure 3)
Figure 3: The radiograph shows a spasm of the esophagus at level D-6 after the first swallow and a large gas bubble of the stomach. The operation was prescribed only on the basis of HRM. The muscles dissection was done at level D-3 (Figure 3b- after surgery – arrows), i.e., = 5cm above spasm (Figure 3a)
in a horizontal position without pressure provocation. Therefore, he has episodes of reflux into the esophagus at night if the presence of chyme in the stomach. In milder cases, during reflux, the barium is retained in the ampulla, which is closed proximally by the functional sphincter. But this functional sphincter does not function in this case, but there is a functional narrowing at the level of the anatomical narrowing of the esophagus, due to the pressure of the aortic arch. Probably at night, when the patient had swallowing saliva, it accumulated between this functional sphincter at the level of the aorta (arrow in figure 4 a) and the upper esophageal sphincter. When the esophagus filled with saliva between sphincters, resulted in increasing pressure, the upper esophageal sphincter cannot handle the pressure and relaxes. This causes saliva to reflux into the throat. After the passage of the tablet through this functional sphincter, its tone decreased, which contributes to the free passage of saliva through this zone. This case confirms numerous reports that GERD can progress for a long time without noticeable symptoms. From the current definition of GERD, it follows that if a person has no significant complaints, then he does not have GERD. Obviously, this definition is wrong!
In the case described by Choi et al [11] (Figure 2 a), spasm of the esophagus is determined at the level of the aortic arch. The presence of a large gas bubble indicates sufficient patency of this zone of the esophagus. In 3 out of 7 observations (a, b, c) there is such a narrowing, which can be explained by a spasm of circular muscle fibers in response to hydrochloric acid stimulation. This is because the acid is trapped over the anatomical narrowing of the esophagus, which is caused by the depression of the aortic arch.
CONCLUSION
This mini-review shows that manometric changes in the esophagus, which without reason are considered a diagnosis(JE), are pathogenetic features of GERD. These patients should receive complex pathogenetic treatment against GERD. Replacing GERD treatment with PPI alone has been the cause of cases of refractory to acid-suppressing treatment. Therefore, in cases of resistance to standard treatment with PPI, this should not be the basis for operative intervention. Long-term complex treatment of GERD with the use of expansion of the spasm zone can significantly reduce the need for surgical treatment. There are no long-term outcomes after oral endoscopic myotomy (POEM) in the literature. Second, new trendy therapies are known to often experience a surge of positive feedback. It is already known that POEM in achalasia is associated with an increase in the incidence of GERD [14]. One can agree with these authors that “large sample, multi-center, long-term study reports are needed, and it promotes the development of NOTES technology” [15].
![Simultaneous X-ray study with HRM of a person from the control group from article by Kwiatek et al [3]. Formation of a phrenic ampulla is shown, which is closed proximally by the contractile deceleration point (CDP) to create high pressure, open the LES, and inject a bolus into the stomach. This contraction zone is shown on the HRM. The authors argue that the endoclip, attached to the squamocolumnar junction (SCJ), shifted cranially during the emptying of the ampulla, which allegedly confirms the idea of shortening the esophagus. In fact, the endoclip has not shifted. In both images, it is located to the left of the lower angle of the 10th thoracic vertebra. But the distance between the stomach and the clip somewhat decreased because of the opening of the intra-abdominal part of the LES. In both images, the length of the LES is shorter than the norm (1.5 vs. 3.6 cm). {the height of the 10-thoracic vertebra (red line) is about 2 cm long}.](https://www.jscimedcentral.com/public/assets/images/uploads/image-1691659436-1.PNG)