Open-System Colon Irrigation Bowel Prep for Colonoscopy is a Safe and Effective Alternative to Oral Prep
- 1. Gastrointestinal Associates and Endoscopy Center, Jackson, USA
- 2. Ohio Gastroenterology and Liver Institute, Cincinnati, USA
Abstract
Background: Colonoscopy is the most common practice for the evaluation of the lower gastrointestinal tract. High-quality bowel preparation is imperative to ensure adequate visualization and surveillance of colon neoplasia. It has been reported that approximately 20% of outpatients have inadequate colon preparation, in part due to difficulties associated with the traditional purgative-based oral prep. An FDA-cleared, prescription-based, open system to purge the colon with water before colonoscopy is available and provides an alternative to oral prep.
Aim: Evaluating the clinical outcomes, safety, adequacy, and patients’ satisfaction of the high-volume colon irrigation bowel prep for colonoscopy prescribed by physicians from two independent endoscopy centers.
Methods: This retrospective study provides data analysis of 3,050 consecutive bowel prep procedures prescribed by 35 gastroenterologists. Patients’ demographics and safety data were recorded by the technical staff following stringent protocols. The examining physician provided bowel preparation adequacy, and patients’ satisfaction was recorded using post-procedure surveys.
Results: The high-volume colon irrigation provided 97% adequacy with no serious adverse events, reflecting its efficacy and safety. The study presented excellent patients’ satisfaction and willingness to repeat. The outcomes were maintained regardless of the patients’ age, gender, pre-prep regime, and underlying diseases.
Conclusion: Open system high-volume colon irrigation used under stringent standardized protocols is a favorable strategy for colonoscopy prep. Adopting this technology can lead to increased effectiveness and improved patients’ procedural experience, thus reducing the healthcare system’s costs associated with canceled, failed, and inadequate colonoscopies.
Citation
Hogan RB II, Underwood JA, Wright C, Lestina LS, Mangels DG, et al. (2021) Open-System Colon Irrigation Bowel Prep for Colonoscopy is a Safe and Effective Alternative to Oral Prep. JSM Gastroenterol Hepatol 8(1): 1098.
Keywords
• Bowel prep
• FDA
• Colonoscopy
• Colon preparation
• Colonoscopy quality
INTRODUCTION
Colorectal Cancer (CRC) is the third most common malignancy globally and the second most common cause of cancer death in the United States [1]. Colonoscopy is the most common practice for evaluating the lower gastrointestinal (GI) tract and is often preferred by physicians as it stands alone in its ability to be both diagnostic and therapeutic [2,3]. Inadequate Bowel Preparation (BP) for colonoscopy is associated with adverse outcomes including lower adenoma detection rates, increased procedural time, elevated direct (procedure-related) and indirect (e.g., transportation, loss of productivity) costs to the healthcare system [4,5]. Hence, BP for colonoscopy was studied by several international societies that published guidelines, and a call was made for more stringent quality performance thresholds for BP [6-8].
Factors related to BP inadequacy include age, comorbidities (e.g., diabetes, gastroenterology diseases), obesity, opioid use, and neurological conditions [7,9]. Other factors include demographics and noncompliance with BP instructions [10-14]. The recommended standard of care for colonoscopy BP is a split dose of oral purgative administration unless the colonoscopy is done the same day [7]. The inconvenience following this standard of care protocol includes disruption in daily routine, loss of sleep, and interference with work commitments. Although oral purgative BPs are considered safe and well-tolerated, there is a recognizable burden on the patients. These might be associated with complications such as nausea, vomiting, and electrolyte disturbances [7]. High-quality BP is imperative to ensure quality visualization of the colonic mucosa and the identification and removal of lesions for prevention, detection, and surveillance of CRC. Unfortunately, approximately 20% of outpatient and up to 60% of inpatient procedures are associated with inadequate BP, despite taking an oral prep [15-18]. Inadequate BP was a cited factor in 20% to 70% of incomplete colonoscopies. Recognizably, an inadequate BP is also associated with low patient satisfaction, which inevitably reduces compliance with guidelines for screening and follow-up colonoscopies. It also necessitates repeat examinations earlier than would be recommended with adequate BP.
An FDA-cleared open-system technology to purge the colon by controlled gravity fed, low pressure, water infusion provides an alternative to overcome the well-established issues with the oral purgative colonoscopy BP. This system enables performing BP method that has been indicated well-tolerated and effective for colonoscopy BP [19] in hundreds of patients (Austin gastroenterology, Austin, TX) [20]. The BP is prescriptionbased and performed by highly trained personnel operating under stringent Standard Operating Procedures (SOPs). This retrospective analysis reviews the clinical outcomes, safety, adequacy, and efficiency of 3,050 BPs prescribed by 35 physicians in two independent centers (Jackson, MS, and Cincinnati, OH) performing this high-volume colon irrigation BP. The study also analyzed patients’ satisfaction and willingness to repeat, which are critical elements for optimizing colon preparation and overall clinical experience and outcomes.
METHODS
High-volume colon irrigation bowel prep
The high-volume water irrigation BP is used to purge the colon by water infusion before colonoscopy [19,20]. It is FDA-cleared and intended for use when medically indicated, such as before radiological or endoscopic examination. The BP is performed by trained personnel and under stringent Standard Operating Procedures (SOPs). During the BP, the patient is seated on the disinfected basin, and a sterile, disposable nozzle is inserted about 1 inch into their rectum. Gravity-fed water (37°-39°C) flows into the bowel, loosening stool and allowing the patient to evacuate their colon. Water continues to wash and clean the colon until the patient is notified that the BP is completed. The BP takes approximately one hour and is automatically stopped if the water temperature exceeds the safe range of 37°-39 °C. As a pre-BP regiment, patients were asked to follow a Clear Liquid Diet (CLD) the day before and the day of their colonoscopy (similar to instructions given for oral purgative based BP). They were also instructed to take a stimulant laxative (bisacodyl, 2 X 5 mg) twice on the day before the BP (noon and evening) and once on the morning of their high-volume colon irrigation BP and colonoscopy. The physicians (n=16) from GI Associates (GIA, Jackson, MS) also instructed the patients to take magnesium hydroxide (gentle laxative and antacid) several days (1-5) before their BP. The magnesium hydroxide instruction was not given by the physicians (n=19) at the Ohio Gastroenterology and Liver Institute (OGI, Cincinnati, OH).
Collection of clinical data and demographic information
This is a retrospective review of the patients’ demographic data and medical history who underwent high-volume colonic irrigation BP for colonoscopy. Clinical and demographic data were collected from two centers: GI Associates (GIA)-Hygieacare Center in Jackson, MS (MS, October 2017-December 2019), and Ohio Gastroenterology and Liver Institute (OGI)-Hygieacare Center in Cincinnati, OH (February 2017- December 2019). Procedures were prescribed by 35 physicians, 19 in Cincinnati and 16 in Jackson. The demographic and self-reported clinical data were collected via the patients’ responses to questionnaires. Since this is a retrospective descriptive study, in a standard FDA and unchanged approved procedure, deidentified and with patient consent, no IRB was required. The examining physicians provided the BP’s adequacy for the colonoscopies, and the data were fed to the database directly by an employee of the endoscopy center.
Recording and analysis of adverse events
All adverse events that occurred during and immediately after the high-volume colonic irrigation BP procedures were documented by the center’s staff. The adverse events recorded included nausea, vomiting, dizziness, and abdominal cramping.
Data collection for the sensitivity of the BP to different pre-prep regimes
Pre-colonoscopy BP instructions are usually prescribed to patients by their doctors, regardless of the chosen method. These include a clear liquid or low residue diet (CLD or LRD) and oral purgatives. The pre-preparation for the high-volume colon irrigation BP typically involves these dietary restrictions coupled with a laxative such as bisacodyl, given at various doses. The sensitivity of the high-volume colon irrigation BP adequacy to these pre-prep regimes was determined by retrospectively studying the center’s database for prep adequacy trends in correlation with the patients’ compliance to the pre-prep orders they received from the physicians. Data from 2,626 patients (888 from GIA, 1,738 from OGI) was collected for dosage and the total amount of the stimulant laxative (bisacodyl) taken before the BP. For the MS center, data for pre-prep consumption of magnesium hydroxide (not utilized at the OH center) was also collected.
Analysis of patients’ reports on oral purgative bowel preparation
Of the procedures completed at both centers, in 2,310 database entries (n=870 for MS, n=1,440 for OH), patients report having previously had a colonoscopy prep using oral purgatives. Out of those 1,063 patients (n=423 for MS; n=640 for OH) chose to respond to an open-ended question asking them to describe problems they have experienced with oral purgative prep, regardless of the specific oral prep they used in the past. Analysis of these open-ended answers was done using word cloud analysis using the DisplayR software (displaayr.com).
Patients satisfaction analysis and willingness to repeat the high-volume colon irrigation BP
To estimate patients’ satisfaction, all patients were provided with a post-BP satisfaction survey that included four questions referring to the high-volume colonic irrigation quality: 1. Was the check-in welcoming and efficient; 2. Were the explanation received from the staff about what to expect clear and to the point; 3. Were the techs available as needed and adequate privacy kept; 4. Were the prep room and system clean to their satisfaction. The survey also included one question regarding their patients’ willingness to repeat the high-volume colon irrigation BP for their next colonoscopy. The answers to the survey questions were ranked: definitely agree, agree, disagree, or definitely disagree. The responses to the survey were analyzed by counting responses in each category for each of the centers, and the results are presented per rating and satisfaction percentages.
Also, patients were provided with a space to respond in an open-ended format describing their BP experience. To analyze these open-ended answers, we used the DisplayR (displaayr. com) software, utilizing both world cloud analysis and Artificial Intelligence (AI) analysis based on Natural Language Processes (NLP) algorithm to represent the patients’ responses. Results are presented as a word-cloud visual, which summarizes the most repeating words in the open text boxes. For the BP evaluation, sentiment analysis was done to provide an additional, unbiased estimate of the overall patients’ responses to their BP. For the open-ended questions, 2,468 responses were analyzed.
RESULTS
Clinical outcome, demographic data, and adverse events
For the study time analyzed, the two centers performed 3,050 high-volume colonic irrigation BP procedures to prepare patients for colonoscopy. Of those, 1,152 and 1,883 procedures were performed at MS and OH, respectively (Table 1).
Table 1: A summary of all high-volume colon irrigation procedures performed in two centers, Jackson, MS (October 2017-December 2019), and Cincinnati, OH (February 2017-December 2019).
| Centers performing high-volume colon irrigation procedures | Both centers combined | ||
| MS center | OH center | ||
| Number of patients | 1,117 | 1,833 | 2,950 |
| Procedures performed in the center | 1,167 | 1,883 | 3,050 |
| Procedures with outcome reports | 1,099 (94% of total) | 1,856 (99% of total) | 2,955 (97% of total) |
| Adequate procedures | 1,064 (97% of reported) | 1,811 (98% of reported) | 2,875 (97% of reported) |
| Age | 62±14 (n=1,027) | 62±11 (n=1,837) | 63±10 (n=2,864) |
| Gender | Male – 318 (31%) Female – 709 (69%) (n=1,027) |
Male – 572 (34%) Female – 1,125 (66%) (n=1,697) |
Male – 890 (32%) Female – 1,834 (68%) (n=2,724) |
| Patients with underlying diseases | 571 (51% of total patients) | 850 (46% of total patients) | 1,421 (48% of total patients) |
| Patients self-reporting regarding having had previous colonoscopies | 501 (77% of responses) | 1,376 (98% of responses) | 1,877 (91% of responses) |
| Patients that have had multiple HygiPrep Procedures | 18 (total of 37 procedures) | 31 (total of 71 procedures) | 49 (total of 108 procedures) |
The patients’ age ranged from 18 to 92, with a mean and standard deviation at 63±10 (62±14 at MS, and 62±11 at OH). The gender distribution was 68% female and 32% male and was similar between the centers. Patients’ self-reported medical history revealed that 48% (n=1,421 patients) of total patients had various underlying diseases, including diabetes, Crohn’s disease, ulcerative colitis, celiac, and chronic constipation (Table 1). The procedures yielded adequate BP in 97% of patients, regardless of demographic data and reported medical history. Table 1 summarizes all the clinical outcomes and demographic data.
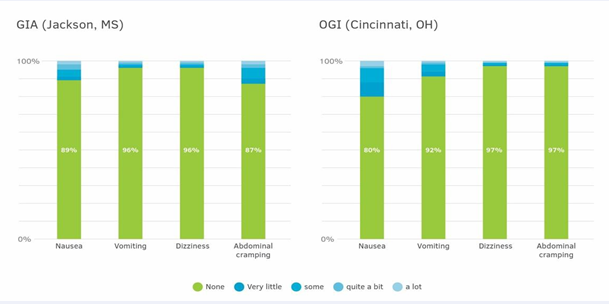
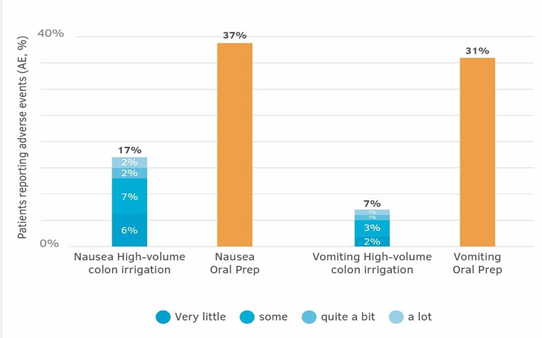
Adverse events are monitored continuously at the centers by the nurses and technicians. The referring physicians reported no serious adverse events (SAE) in 3,035 consecutive procedures. Expected adverse events (AE) during the procedure, as defined in the consent forms, were reported by the attending professional and included various levels of nausea, vomiting, dizziness, and abdominal cramping. No AEs were reported in 66% of all the procedures held at the MS center and 90% of those performed at the OH center. The different AE were individually recorded in 4%-13% of the procedures done at the MS center, and 3%-10% of the patients performed at the OH (Figure 1).
Figure 1: Percentage of specific adverse events by their intensity in both studied centers. The total number of patients: MS - n=1091-1097, OH- n=1818-1833. The variability of the number of recorded patients is due to the specific adverse events.
Clinical outcome was provided for 560 high-volume colonic irrigation procedures reported to have had AE in both centers. Of those, 550 (98%) were indexed with an adequate BP, and 10 (2%) had an IBP.
The sensitivity of the high-volume colonic irrigation BP to different pre-prep regimes
A retrospective analysis was performed to determine the correlation between stimulant and osmotic laxative pre-prep regimes and the clinical outcome of the high-volume colonic irrigation BP on 2,626 patients (888 from MS, 1,738 from OH). The analysis revealed that 90% of the patients (n=2,363) followed the prescribed laxative bisacodyl instructions, which are three doses of two tablets each (each tablet is 5 mg). The other 10% (n=259) were randomly taking the laxative, and their consumption ranged from one dose of two tablets to four doses of three tablets at a time. The total amount of laxative taken by the patients was 0 to 60 mg bisacodyl. Regardless of the total amount of bisacodyl taken, the clinical outcome of BP allowed physicians to complete the colonoscopy. Additional data were analyzed to consume the various amounts of magnesium hydroxide during the days before the BP, as prescribed in the MS center. Out of a total of 1,064 patients reported to have had adequate BP, 69% (n=731) patients have taken magnesium hydroxide. Of the 35 patients who reported having an inadequate BP, 63% (n=22) have taken magnesium hydroxide. A statistical analysis of the colonoscopy outcome’s adequacy between patients that have taken magnesium hydroxide and those who have not yielded a p=0.25 (one-tailed equal-variance t-test), which proves that no significantly statistically clinical outcome depended on this utilization strategy.
Patients’ reports on oral purgative bowel preparation
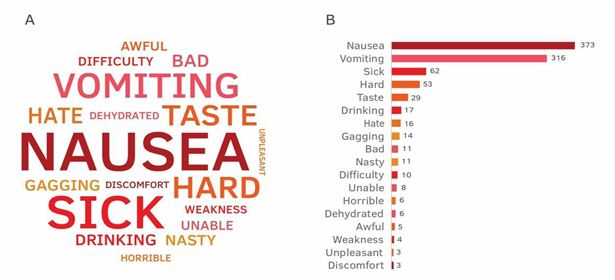
For 2,060 of the 3,035 high-volume colonic-irrigation procedures indexed, patients answered the question, “Have you previously had a colonoscopy?” (654 at MS, 1,376 at OH). Of the reported, 77% of the 654 survey responders at the MS center, had previous colonoscopies. At the OH center, 98% of 1,376 survey respondents reported having had previous colonoscopies. The patients were also asked whether they had difficulties with taking an oral purgative and were provided an open-ended question asking them to elaborate on any possible challenges they have experienced. Responses from 1,019 patients pointed that nausea (37%), vomiting (31%), difficulties drinking the liquid of the oral purgative (10%), and sickness (6%), were associated with the oral prep (Figure 2A and 2B)
Figure 2: Patients’ feedback (n=1,019) on past colonoscopy bowel preps done using oral purgative. Feedback was provided as a response to an open- ended question asking them to describe their previous experience with taking an oral purgative bowel prep. The analysis was done on the combined responses from both studied centers. A: Word-could descriptive analysis based on the abundance of all the words in the patient’s responses. B: A bar graph abundance analysis for the top 18 words repeated in the patients’ open-ended responses.
Patient satisfaction and willingness to repeat
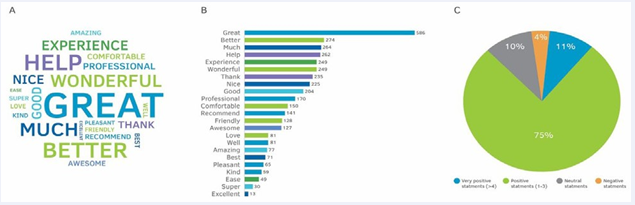
The patient satisfaction survey revealed that patients in both centers were satisfied with the high-volume colon irrigation procedure (Table 3). The questions included inquiries about the check-in procedure, the technicians’ explanations, technicians’ availability, adequate privacy, and cleanliness of the room. The overall average satisfaction (“very good and “good”) was 99% for each of the centers. The rating was “very good” for 94%-99% for all questions between the two centers, and 1%-4% were rated “good”. The patients were also provided an open-ended question where they were asked to state their opinion on their experience with the high-volume colon irrigation BP. Figure 3
Figure 3: Text analysis of patients’ (n=2,468) feedback on their opinion of the high-volume colon irrigation bowel prep (BP). Feedback was provided as a response to an open-ended question asking them to describe their experience during the BP post-procedure. The analysis was done on responses from both centers that participated in the study. A: Word-could graphic analysis based on the abundance of all the words in the patient’s responses. B: A bar graph describing the abundance analysis for the top 23 words repeated in the patients’ open-ended responses. C: Natural language process (NLP)-based Sentiment analysis of all the open-ended responses for understanding the patient’s opinion on the high-volume colon irrigation BP procedure.
represents the analyses of the 2,468 responses received at both centers. A wordcould analysis revealed that the words: “better”, “much”, and “helpful & help” appeared in 11% of the responses. The words: “wonderful”, “experience”, and “thanks & thank you” appeared in 10% of the responses (Figure 3A and B). We ran the responses through an artificial intelligent natural-learning-processes (AI NLP)-sentiment analysis algorithm to avoid analysis-bias of the open-ended responses. The results show that 11% of the responses have multiple (>3) positive statements, 75% of the responses had one-to-three positive statements, 10% of the responses were neutral, and 4% had negative statements (Figure 3C). Overall, 86% of the statements provide positive and highly positive sentiment analysis for the high-volume colon irrigation BP.
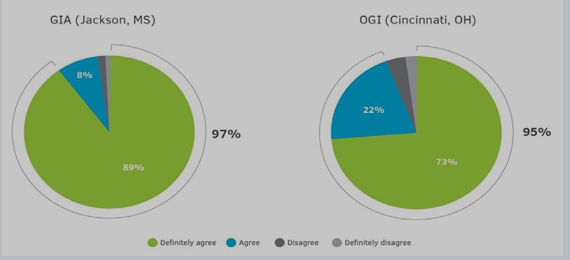
An additional multiple-choice question evaluated patients’ willingness to repeat. Overall, 97% of the patients said they would choose this FDA-cleared high-volume colon irrigation BP for their next colonoscopy. Only 2% of the MS center and 5% of the OH center stated that they would not select this BP for their next colonoscopy. Of the patients stating that they will choose this BP for their next colonoscopy, 89% and 73% of the patients from MS and OH centers, respectively, said they would “definitely agree” to choose this BP for their next colonoscopy prep (Figure 4).
Figure 4 : Willingness to repeat the high-volume colon irrigation bowel preps as reflected from the patients’ response to the statement, “For my next
colonoscopy, I would choose this bowel prep again” (n= 995 for MS, n=1448 for OH).
An additional 8% and 22% of the patients (MS and OH centers, respectively) stated they would “agree” to choose this BP for their colonoscopy’s preferred BP.
DISCUSSION
The clinical outcome and demographic data (Table 2)
Table 2: A summary of all adverse events as recorded in both studied centers, Jackson, MS (October 2017-December 2019), and Cincinnati, OH (February 2017-December 2019). Results are presented as percentages of the patients’ population that have experienced an adverse event at a certain intensity level, as noted and indexed by the nurses and technicians performing the high-volume colon irrigation procedure.
| MS ( n=1091-1097) | OH ( n=1818-1883)1 | |||||||||
| None | Very little | Some | Quite a bit | A lot | None | Very little | Some | Quite a bit | A lot | |
| Nausea | 2% | 2% | 4% | 3% | 1% | 80% | 8% | 8% | 1% | 3% |
| Vomiting | 96% | 1% | 1% | 1% | 1% | 92% | 3% | 4% | 1% | 1% |
| Dizziness | 1% | 1% | 1% | 1% | 1% | 97% | 1% | 1% | 0% | 1% |
| Abdominal cramping | 87% | 3% | 6% | 2% | 2% | 97% | 1% | 1% | 0% | 1% |
The variability of the number of recorded patients is due to the specific adverse events.
show that despite the age range, gender, and other patient demographic differences, the FDA-cleared high-volume colon irrigation approach, utilizing stringent operating procedures, yielded highquality bowel prep (BP) for colonoscopy in 3,035 consecutive procedures. A minimum of one underlying disease was reported for 48% of the patients in both centers. These diseases included gastrointestinal and metabolic disorders such as diabetes, inflammatory bowel disease, celiac, and chronic constipation, often considered poor BP risk factors [7,21]. Although 48% of the patients had at least one underlying disease, the high-volume colon irrigation BP consistently provided an adequate BP that far exceeds national benchmarking thresholds for colon preps of 85% adequacy [7]. This BP was agnostic to pre-prep regimes, where various regimes of the laxative bisacodyl and magnesium hydroxide consumption proved to have no significant statistical influence on the adequacy outcome of the colonoscopy. Patients’ compliance with prescribed ancillary pre-prep regimes has been a recognized factor for attaining a satisfactory result [22]. Thus, we conclude that the high-volume colon irritation BP, agnostic both to various pre-prep regimes and multiple well recognized poor BP risk factors, is to be considered a favorable and potentially preferential choice for BP.
Importantly, the high-volume colon irrigation preparation for colonoscopy is a beneficial BP for both the patient and the prescribing physician. This high-volume colon preparation’s economic impact has been demonstrated to have significant potential favorable financial savings for the healthcare system [23]. A key issue is always focused on safety, and, in over 3,000 procedures performed in both centers since 2017, there have been no serious adverse events. Other AEs reported include various levels of nausea, vomiting, dizziness, and abdominal cramping (Figure 1). The traditional oral purgative-based BPs, although generally considered safe and effective, have both acute and permanent toxicities and are known to possibly promote nausea, vomiting, dehydration, dizziness, palpitation, abdominal discomfort, electrolyte imbalance, fatigue, and headache [7].
The AEs from oral BP formulations are reported by up to 58% of the patients. While AE following oral purgative BP is usually not considered a health threat, the AE can be potentially serious [24-26]. Based on the patients’ reports on AE during their previous oral BP experiences, the most common were nausea (37%) and vomiting (31%) (n=1,019, Figure 2B). These numbers are 2-3-fold higher than those reported for the 3,035 patients who underwent high-volume colon irrigation BP (Figure 5).
Figure 5: Percentage of patients reported to have experienced vomiting or nausea during high-volume colon irrigation bowel prep procedure and while taking an oral purgative prep. For the high volume colon irrigation prep, data were collected from the patients’ adverse events (AE) reports
- n=2,930 patients for nausea and n=2,927 for vomiting (for both centers included in the study). For the oral prep, data were collected by asking patients to provide information regarding past experiences with taking an oral prep, n=1,019.
This study showed that using high-volume colon irrigation BP, performed under stringent SOPs, significantly reduced BPassociated AE prevalence. We found no correlation between the AE and the clinical outcomes of the high-volume colon irrigation BP. The constant adequacy achieved in patients choosing this BP can provide advantageous predictability for physicians and endoscopy centers and can decrease the number of canceled procedures.
Patients’ satisfaction was exceptional, with 99% of the patients stating that they liked the high-volume colon irrigation BP and over 95% of the patients expressing willingness to repeat the procedure for their next colonoscopy. Many patients also expressed their satisfaction with this BP in their open-ended responses when asked about their post-BP experience Table 3
Table 3: A summary of patients’ responses to the multiple-choice satisfaction survey was presented at the end of the high-volume colon irrigation bowel preps. Results are presented as the percentage of responses. For the MS center, the number of responses was 1,037-1,040, and for the OH center, the number of responses was 1,652-1,657 (variability due to the variable number of responses in the survey.
| MS center | OH center | |||||||
| Definitely agree | agree | disagree | Definitely disagree | Definitely agree | agree | disagree | Definitely disagree | |
| Check-in was welcoming and efficient | 97% | 2% | 0% | 1% | 94% | 4% | 0% | 1% |
| Explanation received from my tech about what to expect was clear and to the point | 98% | 1% | 0% | 1% | 96% | 3% | 0% | 1% |
| Techs were available as needed; adequate privacy was kept | 98% | 1% | 0% | 1% | 97% | 2% | 0% | 1% |
| Prep room/system were clean to my satisfaction | 99% | 1% | 0% | 1% | 96% | 2% | 0% | 1% |
| Average satisfaction | 98% | 1% | 0% | 1% | 96% | 3% | 0% | 1% |
Patients that had used an oral purgative for past colonoscopies expressed their unhappiness with that prep and described common issues with the traditional prep (Figure 2). Providing a BP that is preferable to patients can increase the likelihood of these patients to return for scheduled recommended subsequent colonoscopies, as advised by the professional associations [21,27]. Doing so will reduce the patients’ risks, improve CRC prevention, and potentially reduce the subsequent overall costs for the medical healthcare system [21,23].
This study has several strengths and weaknesses. It is the first robust analysis reporting thousands of patients undergoing a physician-prescribed open-system colon irrigation BPs (n=3,050). The patients were prescribed the high-volume colon irrigation BP by 35 physicians from two independent endoscopy centers, and almost half of the patients had underlying diseases (Table 1). Therefore, the consistent clinical adequacy (97%) in both centers regardless of any demographic and medical parameter is strong evidence for this BP’s benefits. A weakness of this study is that it reports retrospective data. Additionally, we examined various data entries that included reporting by the performing nurses and tech team, self-reporting patients, and the endoscopy center staff. When looking at 3,000 procedures, it is expected to have “noise” introduced to such data. At the same time, we also see this as one of the biggest strengths of the manuscript as we report results for a minimum of 1,000 patients in each of our individual analyses.
The two centers studied in this retrospective review reported outstanding BP adequacy for colonoscopy regardless of the patients’ age, gender, pre-prep regime, and underlying diseases. The satisfaction results, and almost ubiquitous willingness to repeat, attest that this is a preferable BP approach for patients, even though this procedure is currently an out-of-pocket expense. The consistent clinical outcomes position this technology to be an excellent alternative to the traditional oral purgative prep, and patients, physicians, and payers would greatly benefit if patients had access to this BP with insurance allowed coverage. Highvolume colon irrigation BP has been shown safe and effective with excellent patient-reported satisfaction and no SAE in over 3,000 procedures. We suggest that utilizing this BP technology can reduce canceled, aborted, or early repeat colonoscopies with the associated direct and indirect losses. These combined advantages have significant recognizable values to the patients’ willingness to have colonoscopy and repeat procedures as well as the physicians and healthcare systems providing these services.
ACKNOWLEDGMENT
All the data for this retrospective study were provided by Dawn Burleson, RN MBA CRA, and Orly Levitan, PhD, from Hygieacare Inc. (Norfolk, VA, USA). We are thankful to David A. Johnson, MD MACG FASGE MACP, for providing his comments and insights on our manuscript. There was no external funding for this study.
Authorship statement: The guarantor of the article is Dr. Reed Hogan, MD. The specific author’s contribution was as follows: R.H. led the efforts of putting together the manuscript, J.A.U. and T.O. contributed their perspective on the study and colonoscopy bowel preparation, R.H., J.A.U., C.W., L.S.L., D.G.M., and T.O., all took equal parts in performing many of the reported procedures of the study and providing clinical data and perspective. All authors are hereby stating that all authors approved the final version of the manuscript.