Risk Stratification Tool for Predicting Postoperative Outcomes in Patients Undergoing Esophagectomy: A Prospective Study
- 1. The 3rd Affiliated Teaching Hospital of Xinjiang Medical University (Affiliated cancer Hospital), China
Abstract
Purpose: Frailty, a clinical syndrome characterized by a reduced physiological reserve and decreased resistance to stressors, is extremely common in oncology patients. Given that esophagectomy is associated with significant postoperative adverse outcomes, the early identification of high-risk patients is critical. This study compared the utility of the Modified 5-Factor Frailty Index (mFI-5) and the Modified Charlson Comorbidity Index (mCCI) in predicting postoperative outcomes in patients undergoing esophagectomy.
Method: We reviewed the records of patients who underwent esophagectomy between 2019 and 2022. Two validated risk stratification tools measured the burden of comorbidity: mFI-5 and mCCI. The primary outcomes included a prolonged postoperative hospital stay and major and minor postoperative complications.
Result: A total of 359 patients were included (mean age 63.1±8.6 years; 74.4% were males). The length of postoperative hospital stay was 30.0 (IQR 25.0, 39.5) days, with 37 patients (10.3%) experiencing major postoperative complications and 192 patients (53.5%) experiencing minor postoperative complications. In multivariate analysis, mCCI remained a significant predictor of major postoperative complications (OR=1.52, 95% CI 1.01–2.3, p=0.046), but was no longer a significant predictor of prolonged postoperative hospital stay or minor complications. In addition, the mFI-5 score was no longer a significant predictor of any of the three postoperative outcomes.
Conclusion: This is the first study to compare the utility of the mFI-5 and mCCI in predicting adverse postoperative outcomes in patients undergoing esophagectomy. Our findings suggest that mCCI is a valid predictor of major complications in this patient group, whereas the role of mFI-5 is limited. This should be further investigated in a prospective multicenter cohort study.
Keywords
• Frailty
• Gastrointestinal cancer
• Modified frailty index
CITATION
Yan R (2023) Risk Stratification Tool for Predicting Postoperative Outcomes in Patients Undergoing Esophagectomy: A Prospective Study. JSM Gastroenterol Hepatol 10(2): 1122.
INTRODUCTION
Esophageal cancer is the eighth most common cancer worldwide and the sixth leading cause of cancer-related deaths due to its highly aggressive nature and low survival rate [1]. With the progression of an aging population and the increasing incidence of esophageal cancer, the number of older adult’s patients with esophageal cancer will increase dramatically [2]. Despite the use of multimodal neoadjuvant treatments such as radiotherapy or chemotherapy, esophagectomy remains the only curative treatment for esophageal cancer [3]. Esophagectomy is associated with significant postoperative complication rates, mortality, and prolonged hospital stay [4,5]. The incidence of surgical complications after esophagectomy ranges from 30–70%, with a mortality rate of 1-5% [6,7]. Early identification of high-risk patients can prevent poor outcomes and prolonged hospital stays by adapting clinical care pathways [8]. Therefore, an accurate and comprehensive preoperative risk assessment is an essential guide to selecting clinical treatment options and predicting postoperative complications. Frailty is a clinical syndrome defined as a reduced physiological reserve and decreased resistance to stressors and is a commonly used indicator of a patient’s physiological status [9]. Frailty is strongly associated with poor patient outcomes in the postoperative period [10]. Recent studies have introduced a simplified 5-factor Modified Frailty Index (mFI-5) consisting of five clinical conditions: functional status, diabetes history, chronic obstructive pulmonary disease, congestive heart failure, and hypertension; each condition is assigned a value of 1, with a minimum score of 0 and a maximum score of 5. Higher scores imply more severe debilitation [11,12]. Studies have shown that the mFI may be helpful in the preoperative identification of patients who may beat high risk of morbidity and mortality following esophagectomy [4]. Another common preoperative risk stratification indicator is the Charlson’s Comorbidity Index (CCI), which is also used to assess the comorbidity burden of patients [13]. The CCI has been shown to predict long-term mortality in different clinical populations, including medical, surgical, intensive care units, trauma, and cancer patients [14]. However, to date, there has been no clear consensus on the most effective risk stratification method for predicting adverse postoperative outcomes in patients undergoing elective esophagectomy for esophageal cancer. Therefore, this study aimed to compare the utility of the mCCI and mFI-5 in predicting postoperative outcomes in patients undergoing esophageal cancer.
MATERIALS AND METHODS
Patient characteristics
This study was reviewed and approved by the hospital’s medical research ethics committee, and enrolled 387 patients who underwent elective surgical treatment for esophageal cancer between May 2019 and March 2022. All patients were pathologically confirmed to have esophageal cancer after surgery and biopsy samples were collected using the surgical anesthesia system, while electronic medical records were queried to collect data for statistical analyses. Inclusion criteria for the study were the following [1]. Patients who attended the Xinjiang Medical University Cancer Hospital and had complete case information [2]; all surgeries were elective and the postoperative diagnosis of esophageal cancer was confirmed by the Department of Pathology of the Cancer Hospital of the Xinjiang Medical University; and [3], enrolled patients were over 18 years of age. The following patients were exclude from the study: [1] patients who underwent emergency esophageal cancer resection [2]; patients with incomplete clinical data or those who were lost-to follow-up; and [3], patients who were confused and unconscious, had communication difficulties, and were uncooperative.
Observation Indicators
Clinical information related to the perioperative period was collected and extracted from the surgical anesthesia system and the electronic medical record system, and included sex, age, body mass index (BMI), ASA classification, preoperative serum albumin concentration, smoking history, type of cancer, preoperative transfusion history, intraoperative bleeding volume, intraoperative urine volume, total rehydration volume, duration of anesthesia and duration of surgery. The electronic medical record system was queried for patient medical history, including diagnoses of diabetes, chronic obstructive pulmonary disease, congestive heart failure, hypertension, functional status, cerebrovascular disease, myocardial infarction, peripheral vascular disease, and hemiplegia. The presence of renal disease, liver disease, and/or any history of metastatic tumors were recorded. The frailty status of the patients was evaluated using the Modified Frailty Index (mFI), and the comorbidity burden was evaluated using the Modified Chalcedonic Comorbidity Index (mCCI) [4-14].
The length of hospital stay and postoperative complications within 30 days were collected and recorded. If the length of the patient’s postoperative hospital stay (LOH) was <30 days, a telephone call was made. The main complications were defined as one or more of the following: pulmonary embolism, acute renal failure, cerebrovascular accident, myocardial infarction, deep vein thrombosis, sepsis, infectious shock, or death. The outcomes of minor complication were defined as one or more of the following: superficial incisional, pneumonia, progressive renal insufficiency, and urinary tract infection [15].
Statistical analysis
All statistical analyses were performed using the statistical software R and Wind Reach. Normally distributed measures are expressed as means and standard deviations (x±s), while nonnormally distributed measures are expressed as median (M) and interquartile range (IQR). Statistical data were expressed as percentages (%). One-way and multi-way logistic regression models were used to compare the predictive capacity of mFI 5 and mCCI on postoperative complications, and OR and 95% confidence intervals (CI) were calculated. Statistical significance was set at p<0.05. Subject receiver operating characteristic (ROC) curves were generated for the mFI-5 and mCCI on the postoperative results. The area under the curve (AUC), which indicates the predictive power of the test, was calculated for each ROC curve.
RESULT
A total of 387 patients who underwent esophagectomy were included: 28 cases had incomplete clinical data, and 359 cases had complete data. Of these, 267 were males (74.4%) and 92 were females (25.6%), with ages ranging from 34 to 88 years (63.1±8.6). The BMI was 24.2±3.8. ASA classifications were mainly grades 2 and 3, 215 (59.9%) and 132 (36.8%), respectively. The LOS was 30.0 days (25.0, 39.5), with 10.3% of patients experiencing major postoperative complications and 53.5% experiencing minor postoperative complications. Table 1 provides a summary of the patient demographics and perioperative profiles.
The univariate analysis [Table 2], revealed that significant predictors of major complications were a higher mCCI score (p=0.015), older age (p=0.002), higher ASA classification (p=0.007), history of smoking (p=0.040), longer duration of surgery (p=0.013), and longer duration of anesthesia (p=0.017). A higher BMI was a significant predictor of minor complications (p=0.036). Significant predictors of LOS were a higher mFI 5 score (p=0.035), a higher mCCI score (p=0.033), older age (p=0.024), a higher ASA classification (p=0.002), preoperative blood transfusion (p=0.018), longer surgery time (p=0.004), and longer anesthesia (p=0.003).
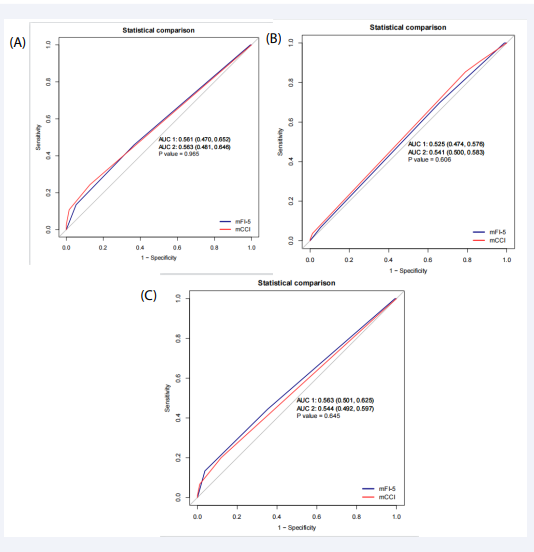
In multivariate analyses, the mFI-5 was no longer found to be a significant predictor of major postoperative complications, minor complications, or prolonged LOS. In multivariate analyses using mFI-5, the ASA grade (OR=2.45, 95% CI 1.23-4.86, p=0.011) was a significant predictor of major postoperative complications [Table 3]. There were no significant predictor variables associated with minor postoperative complications using the mFI-5 [Table 4]. Only the ASA grade (OR=1.99, 95% CI 1.22-3.24, p=0.006) was a significant predictor of a prolonged postoperative hospital stay [Table 5]. The ROC curve analysis produced an AUC of 0.561 for major postoperative complications, 0.525 for minor postoperative complications, and 0.563 for prolonged postoperative LOS [Figure 1].
Figure 1: ROC curves of the multivariable models used to predict the effect of frailty on major complications (A), mimor complications (B) , and prolonged LOS (C).
In multivariate analysis, the mCCI remained a significant predictor of major postoperative complications (OR=1.52, 95% CI 1.01-2.3, p=0.046), but was no longer significant for prolonged postoperative LOS or minor complications. In multivariate analysis using mCCI, ASA (OR=2.31, 95% CI 1.17–4.57, p=0.016) remained a significant predictor of major postoperative complications [Table 3]. There were no significant predictive variables for minor postoperative complications using the mCCI [Table 4]. The ASA grade was also a significant predictor of prolonged postoperative LOS (OR=2.02, 95% CI 1.24-3.27, p=0.005) [Table 5]. The ROC curve analysis yielded an AUC of 0.544 for prolonged postoperative LOS, 0.563 for major complications, and 0.541 for minor complications [Figure 1].
DISCUSSION
This study included 359 patients who underwent elective esophagectomy at the Cancer Hospital of the Xinjiang Medical University between January 2019 and June 2022. This was the first study to compare the predictive values of mCCI and mFI 5 for postoperative outcomes in patients undergoing elective esophagectomy. This study found that mCCI was an independent predictor of major postoperative complications, whereas the mFI-5 could not predict prolonged postoperative LOS or major or minor complications. As the mCCI includes a wider range of comorbidities that may be present in patients, our findings suggest that assessing a patient’s overall comorbidity burden may be more beneficial in predicting postoperative outcomes than the debilitating index.
A growing number of studies have indicated that inadequate physiological reserve is an essential determinant of postoperative outcomes in patients undergoing surgery. During the surgical decision-making process, emphasis should be placed on the patient’s physiological reserve, as improvement in the patient’s postoperative quality of life depends on the ability to tolerate the physiological damage associated with surgical intervention [15]. Esophagectomy causes more surgical trauma than that caused by general surgery, often involving the chest, abdomen, and neck, and may cause postoperative respiratory complications and immunosuppression, leading to postoperative infections in patients with suppressed immunity [4,16]. Therefore, physiological reserve is paramount in patients treated with esophagectomy, and selecting suitable patients for surgical resection is equally critical.
Notably, previous studies have shown that mFI-5 and mCCI are good predictors of postoperative complications [17 19]. In our study, mFI-5 and mCCI were general predictors of postoperative complications. In contrast, in the esophageal cancer cohort of Hodari et al., the mFI was an excellent predictor and showed the ability to identify patients with high complication morbidity and mortality after esophagectomy [4]. Differences in debilitating assessment methods may have contributed to the differences in predictive power. The mFI-5 debilitating assessment method used in the study by Hodari et al. was based on a single deficit, and was subsequently modified by Velanovich et al., to the mFI-11, which was based on a cumulative deficit model including 11 simplified variables [20]. mFI-11, whose score is calculated in the same way as the cumulative index of defects, with higher scores implying more severe frailty, has been shown to predict neurosurgery [21,22], thoracic surgery [23], orthopedic surgery [24,25], and gastrointestinal tumor resection [26,27], of postoperative outcomes. Compared with the mFI-5, the mFI-11 contains more preoperative comorbidities that may potentially influence postoperative complications in esophageal cancer. mCCI Although the mCCI contains many of the same variables as mFI-5, it measures the overall comorbidity burden of the patient, whereas the mFI-5 does not necessarily reflect the patient’s physiological reserve and ability to withstand surgical damage. Therefore, the burden of comorbidity may significantly affect postoperative outcomes more than debilitation. In our multidisciplinary model of care at our tertiary care center, 53.5% of the patients experienced minor postoperative complications, for which neither mCCI nor mFI-5 was a significant predictor. Lee et al. previously found that clinical debilitation adversely affected younger and older patients undergoing esophagectomy for esophageal cancer [28]. However, our findings are consistent with those of Gray et al., in that the mFI-5 could not adequately predict complications after esophagectomy [29]. This discrepancy may be due to differences in perioperative management in this complex patient population. PNI-based nomograms combined with clinical indicators can be used to predict major complications in the early postoperative period and help to enhance perioperative management [30]. In clinical practice, patients can be risk stratified according to risk stratification, early nutritional support can be provided to high risk patients, and perioperative management and monitoring can be strengthened to maximise benefit.
The ROC analysis of mCCI was similar to the ROC analysis of mFI-5. There were no statistically significant differences in the predictive value of postoperative outcomes. Notably, the mCCI significantly predicted major postoperative complications in multifactorial analysis. Although this study used the modified mCCI, the results were similar to those of Yamashita et al., where the CCI was significantly associated with the prognosis of patients with esophageal cancer who underwent curative esophagectomy [31]. This offers potential utility in predicting postoperative outcomes in patients with esophageal cancer to identify patients at high risk for disease progression and potential future surgery. Further validation in a multicenter prospective study is necessary to fully assess its utility.
Our study had some limitations. First, the sample size was small and this was a retrospective study. Second, a scientifically validated frailty rating system for the esophageal cancer population has not yet been established in China, and this, together with the fact that there are no large-scale epidemiological studies on frailty in surgically treated patients in China, all have an impact on the results of this study. Finally, our postoperative outcomes were limited to 30 days after surgery, and long-term follow-up data that recorded results after 30 days may have shown different results. However, the results of this study provide some evidence to elaborate on the predictive power of the mFI-5 and the mCCI for postoperative complications in patients undergoing esophagectomy and provide a basis for future prospective studies.
CONCLUSIONS
In summary, although both the mFI-5 and mCCI have been strongly associated with poor postoperative outcomes and have been widely used in prognostic studies, the results of this study suggest that both comorbidity indicators have a low predictive power for postoperative complications after esophagectomy. Preoperative debilitation significantly affects patients undergoing esophagectomy, and assessing the impact of preoperative debilitation on the outcome is beneficial for clinical decision-making. Therefore, more studies are needed to develop other indicators of comorbidity that may increase the predictive value of outcomes following esophagectomy, using additional relevant variables and a more extensive sample size database. The development of debilitating indicators can help guide treatment strategies and optimize prevention protocols to reduce adverse postoperative outcomes.
REFERENCES
9. Proietti M, Cesari M. Frailty: What Is It? Adv Exp Med Biol. 2020; 1216: 1-7.
12. Khalafallah AM, Huq S, Jimenez AE, Brem H, Mukherjee D. The 5-factor modified frailty index: an effective predictor of mortality in brain tumor patients. J Neurosurg. 2020; 14: 78-86.