Application of the Alvarado Score in the Suspicion of Acute Appendicitis. Prospective and Protocolized Study
- 1. Assistant Professor of the General Surgery Service at the Central Guard of the National Hospital of Clinics, National University of Córdoba (UNC), Argentina.
- 2. Assistant Professor of the General Surgery Service Room 3/5. “PABLO LUIS MIRIZZI” of the National Hospital of Clinics, National University of Córdoba (UNC), Argentina
- 3. General Surgery Residents Room 3/5. “PABLO LUIS MIRIZZI” of the National Hospital of Clinics, National University of Córdoba (UNC), Argentina.
- 4. Head of the General Surgery Room 3/5. “PABLO LUIS MIRIZZI” of the National Hospital of Clinics, National University of Córdoba (UNC), Argentina.
Summary
Background: Acute appendicitis neither suspected nor diagnosed could develop a perforation or otherwise it would take to removing of a normal appendix.
Objectives: Utilization of a clinical score system for aided diagnosis of this pathology and can reduce a negative appendicitis.
Setting: Central Guard Service and General Surgery Service room 3/5 “Pablo Luis Mirizzi”. National Clinical Hospital. Córdoba. Argentina.
Design: Prospective and protocoled study.
Material and Methods: It comprises 1119 patients studied between August 2005 and December 2024. Of these, 588 were male and 531 female, with an average age of 25.3 years. All patients underwent the Alvarado Score at admission surgical exploration was decided in 1061 patients (94.80%). Of the remaining 58 (5.18%), they were excluded due to another pathology. The diagnosis of acute appendicitis was confirmed by surgical findings and pathological anatomy.
Results: Operative findings found that 962 patients (90.60 %), had acute appendicitis. There was no postoperative mortality. In relation to morbidity, there were 2.2% of medical complications and 16.30% of surgical complications. The pathological report showed a normal cecal appendix in 99 patients. Therefore, the incidence of negative appendectomies was 9.3%.
Conclusions: The utilization of score related to the surgical and anatomo pathology finding confirmed it was appreciable from 6 points to acute appendicitis diagnosis.
Keywords
• Acute apendicitis
• Alvarado scores
• Negative appendectomies
Citation
Mariot D, Rojas A, Saliba J, Martinez Peluaga J, Moretti M, et al. (2025) Application of the Alvarado Score in the Suspicion of Acute Appen dicitis. Prospective and Protocolized Study. JSM Gen Surg Cases Images 7(1): 1051.
INTRODUCTION
One of the most common surgical emergencies that are admitted to an on-call service for clinical evaluation, diagnosis and treatment is pain in the right iliac fossa with probable suspicion of acute appendicitis. This undiagnosed pathology can evolve into perforation, with this complication ranging from 15 to 37% [1].
In 1986, Alvarado [2], described a simple Score system, from a clinical point of view, that can be performed by general practitioners and surgical residents in the event of suspicion of acute appendicitis, which will allow a correct diagnosis in the vast majority of cases.
In order to try to reduce the number of normal appendectomies and at the same time not increase the number of appendicular perforations, different types of Scores have been mentioned in the world literatura [3], for the diagnosis of acute appendicitis, but they have been difficult to implement for this pathology.
Undoubtedly, with the use of complementary methods such as abdominal ultrasound and computed tomography in this pathology, it has been possible to reduce the incidence of negative appendectomies [4,5], as well as other modified Alvarado scores [6-9], with varied results.
In our experience, with respect to the subject in different publications [10-13], the objective of which has been to evaluate patients with pain in the right iliac fossa with probable suspicion of acute appendicitis, which has decreased negative appendectomies, which were always controlled with the pathology report.
MATERIAL AND METHODS
Between August 2005 and December 2024, a prospective and protocolized study was carried out at the Central Guard Service and General Surgery Service room 3/5 “Pablo Luis Mirizzi” of the National Hospital of Clinics, whose objective was to evaluate patients with pain in the right iliac fossa region and probable suspicion of acute appendicitis by means of a Score system.
A total of 1,119 patients were hospitalized, of whom 588 were male (53%) and 531 female (47%), with an average age of 25.3 years (range between 15 and 91 years) (Table 1).
Table 1: Sex.
All patients underwent the Alvarado Score at admission, which is based on three clinical symptoms, three physical signs, and two laboratory findings as shown in Table 2.
Table 2: Alvarado's score
|
ALVARADO SCORE |
POINTS |
|
SYMPTOMS Migratory pain in L.R.Q Nausea and vomiting. Anorexia. |
(1) (1) (1) |
|
SIGNS Defense in L.R.Q Fever > 37º C. Painful decompression |
(2) (1) (1) |
|
LABORATORY Leucocitosis (> 10 x 109L). Neutrophil left deviation. |
(2) (1) |
|
TOTAL |
10 |
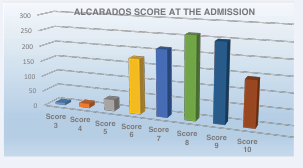
The time between the onset of symptoms and admission to the emergency room was between 1 and 9 days, with the vast majority consulting within 48 hours of admission to the emergency room. (71,4%). On admission, a first Alvarado Score was made, which showed 7 patients with a score of 3 points, 24 with 4 points, 37 with 5, 178 cases with 6, in 214 cases with 7, there were 263 with 8 points, 250 with 9 and finally 146 with 10 points (Table 3).
Table 3: Alvarado’s Score at Admissión.
All patients were hospitalized, and abdominal ultrasound was performed in 569 patients (50.8%). Of these, 210 were negative for diagnostic suspicion (36.9%) and 359 were positive (63%). Finally, 13 abdominal CT scans (1.16%) were performed.
Based on the clinical findings, physical examination, laboratory, and a second assessment with the Alvarado Score, surgical exploration was decided in 1,061 patients (94.8%), of whom 902 had a preoperative suspicion of acute appendicitis (85%), 135 with localized peritonitis (12.7%), and 27 with generalized peritonitis (2.54%).
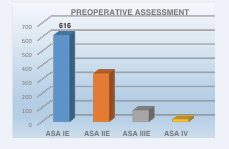
Of the remaining 58 patients of the total (5.18%), 32 cases (2.85%) suffering from gynecological disease and 26 patients (2.32%) with renal pathology were excluded. In relation to the preoperative assessment according to the ASA. Of these, 616 were ASA IE, 344 ASA IIE, 82 ASA IIIE, and 19 ASA EVI (Table 4).
Table 4: Preoperative Assessment.
Finally, the diagnosis of acute appendicitis was confirmed by the surgical findings and the pathological report.
RESULTS
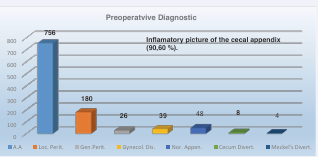
Of the 1061 patients operated on, 962 had an inflammatory picture of the cecal appendix (90.60%). Distributed as follows: 756 patients had acute appendicitis (71.45%), in 180 cases it was localized peritonitis (16.96%) and in 26 with generalized peritonitis (2.45%). Of the remaining 99 patients operated on, 48 cases were normal appendages without other abdominal pathology (4.52%), in 39 women had a gynecological disease (3.67%), 8 with acute cecal diverticulitis in which a right hemicolectomy was performed (0.75%) and finally in 4 with Meckel’s diverticulitis (0.37%) who also had their cecal appendix resected (Table 5).
Table 5: Intra operative diagnosis.
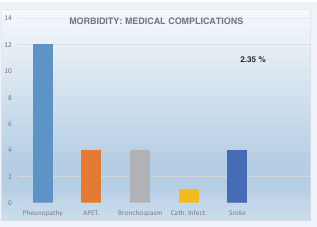
There was no operative mortality. Morbidity was 19 patients (18.66%) Medical complications were 25 patients (2.35%) that included 12 Pheunopathy 4 stroke, 4 APET, 4 Bronchospasm,finally 1 Catheter Infections (Table 6).
Table 6: Morbidity. Medical Complications.
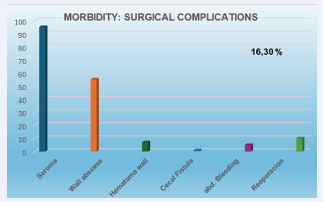
On the other hand, there were 173 patients (16.30%) with surgical complications, among them, 95 cases presented a seroma of the surgical wound (8.95%), 55 a wall abscess (5.18%),7 a hematoma of the abdominal wall (0.65%),1 patient with cecal fistula that evolved favorably with medical treatment (0.65%), 5 abdominal bleeding, plus another 10 total (0.94%) that required reoperation, which include 2 cases of abdominal sepsis, 2 cases of perforated gastric ulcer, 2 cases of acute cholecystitis, 2 cases of intestinal occlusion, and 2 cases of intra-abdominal hemorrhage (Table 7).
Table 7: Morbidity: Surgical complications.
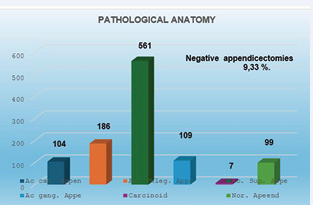
The pathological anatomy of the surgical specimens showed in 104 cases acute catarrhal appendicitis (9.80%), 186 with acute phlegmonous appendicitis (17.5%), 561 with acute suppurative appendicitis (52.87%), 109 with acute gangrenous appendicitis (10.27%), 7 with low-grade neuroendocrine carcinoma or carcinoid carcinoma (0.65%), and 99 patients with a normal cecal appendix (9.33%). Among them, 39 had a gynecological disease (3.67%), 4 had Meckel’s diverticulum (0.37%), 8 had acute cecal diverticulitis (0.75%), and 48 patients had a normal appendix (4.52%). Therefore, the incidence of negative appendectomies was 9.33%, if we compute the total of the normal anatomopathological appendages studied (Table 8).
Table 8: Anatomo.pathological findings.
However, we must draw attention to only 48 patients with normal cecal appendix (4.52%), without other pathology, confirmed by pathological anatomy.
Hospitalization was a mean of 1.33 days. For our study, the use of the Alvarado Score in relation to the anatomopathological findings confirms the diagnosis of acute appendicitis based on an Alvarado´s Score of 6 points.
DISCUSSION
Acute appendicitis (AE) remains the most common abdominal emergency in all emergency departments [14], being more frequent between 10 and 20 years of age, with a preponderance in males [15]. The diagnosis of this pathology is still clinical.
In an effort to reduce this percentage of negative appendectomies, as well as to reduce the time to diagnosis so as not to increase the average number of appendicular perforations, different systems of clinical scores [16,17], abdominal ultrasound [18,19], computed tomography [20,21], various laboratory tests [22,23], have been mentioned in the literature. but we believe, like Denizbasi et al. [24], that when diagnostic imaging methods are not available, we try to use a clinical score system such as the Alvarado Score, which is accessible in our daily work, in order to suspect the pathology.
We believe that, like other authors [25], the findings of abdominal ultrasonography should not influence the clinical judgment of the surgeon in patients with a high probability of AE. We also think that this method should be performed in those patients who will benefit from this study. On the other hand, different authors [17,26], propose the use of abdominal CT in diagnostic studies routinely in patients with pain in the right iliac fossa and suspected AE, in order to further reduce the incidence of negative appendectomies, which would be less than 3%. We, believe, as do Hong et al. [27], that abdominal T.A.C. should not be considered routine for the diagnosis of acute appendicitis. However, it should be taken into account in patients with complicated and advanced acute appendicitis, where they would benefit from this study for diagnosis and probably for initial non-operative treatment [28].
The most determining prognostic factor in AA is appendicular perforation, implying drastic changes in its morbidity and mortality, so much so that the literature shows a mortality of 4% in perforated appendicitis vs. 0.7% in non-perforated appendicitis, in the same way that morbidity varies from 24% in perforated appendicitis to 4% in non-perforated appendicitis [29]. For all of the above, we believe that a timely, early and safe diagnosis represents the key starting point towards correct and effective treatment.
A surgeon familiar with the disease establishes the diagnosis with 97% sensitivity and specificity, comparable to imaging methods [27,30,31]. Alvarado’s score with a score of 6 was close to the diagnosis in 80% of cases, with 7 points in 90%, with 8 points in 93%, with 9 points 95% and with 10 points 100% in our experience.
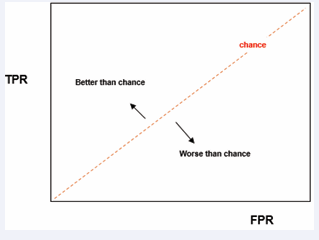
To better understand our results, the ROC curve [32], that combines the True Positive (TPR) and false positive (FPR) ratios is very useful. An ROC space is defined by the relationship between FPR and VPR as x-axes and y, respectively, and represents the trade-offs between true positives (in principle, benefits) and false positives (in principle, costs). Since VPR is equivalent to sensitivity and FPR equals 1-specificity, the ROC graph is also known as the sensitivity vs. (1-specificity) representation. Each prediction result represents a point in the ROC space (Graph 1).
Graph 1: Interpretation of the ROC Curve.
The diagonal divides the ROC space. Dots above the diagonal represent good results, i.e. better than chance, on the contrary, dots below this line represent worse results than chance. This is why, in healthcare, ROC curves are often called diagnostic performance curves.
In our work, we compared the performance of a clinical diagnosis with the score, using the pathological anatomy to determine which were the false positives and false negatives. Thus, the area below the ROC curve found was 0.652. As this is a value higher than 0.50, he indicated that the Alvarado Score made it possible to distinguish true positives from false positives. The CI (95%) was [0.58; 0.72], which confirms that the area would be greater than 0.50 and could reach a value of 0.72 (Graph 2).
Graph 2: Roc curve found in our work.
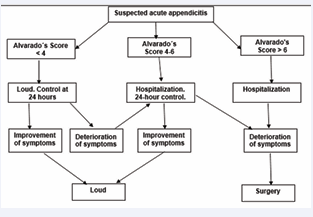
Finally, we believe that based on our findings in this prospective and protocolized study we have decided to carry out a diagnosis, hospitalization and treatment algorithm (Graph 3).
Graph 3: Diagnosis, hospitalization and treatment algorithm.
In patients who have an Alvarado Score of less than 4 points, they should not be hospitalized and will be monitored after 24 hours, to observe their clinical evolution. Those who have a score between 4-5 points should be hospitalized for clinical control for 24-48 hours, and according to their evolution, whether their symptoms have improved, they will be discharged or, on the contrary, the clinical deterioration and the increase in the Alvarado score should be treated surgically. Finally, patients with 6 or more stitches should also be admitted, in order to decide on a surgical procedure as soon as possible. In some publications [2,7,33-36], on clinical assessment of the acute abdomen in patients with suspected acute appendicitis, applying this Score, they have shown a result of 97% of positive diagnosis with a Score equal to or greater than 7, and 86% with a Score equal to or greater than 5 points.
As conclusions, we think that the Alvarado Score is a simple clinical tool to apply in medical practice that can be performed by non-specialized physicians, such as generalists and residents in surgery. In addition, it is a system that has allowed us from a clinical point of view, to reach the diagnosis of the suspicion of Apendicitis and thus reduce negative appendicitis by 9.3%, in the total group with other pathologies such as acute cecal diverticulitis, Meckel’s diverticulum, gynecological processes. But it only decreases to 4.2% when they are taken for suspicion of acute appendicitis where they were negative. We believe that the use of the algorithm presented above, added to a good clinical judgment in the surgical abdomen, was what allowed good results to be obtained in the suspicion of this pathology.
REFERENCES
- Izbicki JR, Knoefel WT, Wilker DK, Mandelkow HK, Muller K, Siebeck M, et al. Accurate diagnosis of acute appendicitis: a retrospective and prospective analysis of 686 patients. Eur J Surg. 1992; 158: 227-231.
- Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986; 15: 557-564.
- Ohmann C, Yang Q, Franke C. Diagnostic scores for acute appendicitis. Abdominal Pain Study Group. Eur J Surg. 1995; 161: 273-281.
- Pinto F, Pinto A, Russo A, Coppolino F, Bracale R, Fonio P, et al. Accuracy of Ultrasonography in the Diagnosis of Acute Appendicitis in Adult Patients: Review of Literature. Critical Ultrasound J. 2013; 5: S2
- Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic Performance of Multidetector Computed Tomography for Suspected Acute Appendicitis. Ann Intern Med. 2011; 154: 789-796.
- Sarang R, Iqbal A, Bawa AP, Singh G, Mishra S, Nongmaithem M, et al. Evaluation of Raja Isteri Pengiran Anak Saleha Appendicitis score: A new appendicitis scoring system. Med J Dr. D.Y. Patil University. 2015; 8: 744-749.
- Gökçe ME, lhan Korkmaz II, Tekin YK, Yurtbay S, Demirta? E, Özsoy O, et al. Comparison of alvarado and ripasa scores in patients with acute apendicitis. CMJ Original Res. 2020; 42: 500-506
- Iqbal MZ, Ahmed Im, Malik NA, Kamra A, Qaiser MU, Riaz S. Comparison of Tzanakis and Alvarado Scoring System in Diagnosis of Acute Appendicitis, with Histopathology as Gold Standard. JRMC. 2020; 26: 290-294.
- Singh VK, Kharga B, Nishant K, Bhutia P, Sharma BK, Pandey NA. Prospective Comparison of Modified Alvarado Score (MAS) and Appendicitis Inflammatory Response Score (AIRS) as a Diagnostic Aid in Acute Appendicitis. Int J Surg Orthopedics. 2016; 2: 21-29.
- Lada PE, Ochoa S, Ternengo D, Sanchez M, Di Benedetto N, Carbonell JM, et al. Use of Alvarado´s Score for the early diagnosis of acute apendicitis. Prensa Med. Argentina. 2005; 92: 447-456.
- Canavosso L, Carena P, Carbonell J, Zuñiga C, Sánchez M, Lada PE, et al. Dolor en fosa ilíaca derecha y Score de Alvarado. Cir Esp. 2008; 83: 243-247.
- Pouget-Baudry Y, Mucci S, Eyssartier E, Guesdon-Portes A, Lada P, Casa C, et al. Le score clinicobiologique d’Alvarado dans la prise en charge d’une douleur de fosse iliaque droite chez l’adulte. J Visc Surg. 2010; 147: 128-132.
- Lada PE, Badra R, Janikow Ch, Massa M, Taborda B, Moretti G, et al. Alvarado Score in the diagnostic of pain in the right lower quadrant. Rev Fac de Cienc Méd. 2017; 74: 213-218.
- Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The Epidemiology of Appendicitis and Appendectomy in the United States. Am J Epidem. 1990; 132: 910-925.
- Humes DJ, Simpson J. Acute Appendicits. BMJ. 2006. 333: 530-534.
- Fenyo G, Lindberg G, Blind P, Enocchson L, Oberg P. Diagnostic decision support in suspected acute appendicitis: validation of a simplified scoring system. Eur J Surg. 1997; 163: 831-838.
- Rao PM, Boland GW. Imaging of acute right lower abdominal quadrant pain. Clin Radiol. 1998; 53: 639-649.
- Gallego MG, Fadrique B, Nieto MA, Calleja S, Ais G, Gonzalez J, et al. Evaluation of ultrasonography and clinical diagnostic scoring in suspected appendicitis. Br J Surg. 1998; 85: 37-40.
- Jahn H, Mathieson FK, Neckelmann K. Comparison of clinical judgment and diagnostic ultrasonography in the diagnosis of acute appendicitis: Experience with score-aided diagnosis. Eur J Surg. 1997; 163: 433-443.
- Arnbjornsson A. Scoring system for computer-aided diagnosis of acute appendicitis. Ann Chir Gynecol. 1985; 74: 159-166.
- Kassem A, Malik A, Basnyat PS. Diagnosis of Acute Appendicitis in Adults: Role of a Simple Clinical Diagnostic Triad. Surg Sci. 2016; 7: 191-194.
- Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004; 91: 28-37.
- Gurleyik E, Gurleyik G, Unalmiser S. Accuracy of serum C-reactive protein measurements in diagnosis of acute appendicitis compared with surgeon’s clinical impression. Dis Colon Rectum. 1995; 38: 1270-1274.
- Denizbasi A, Unluer EE. The role of the emergency medicine resident using the Alvarado Score in the diagnosis in acute appendicitis compared with general surgery resident. Eur J Emerg Med. 2003; 10: 296-301.
- 25.Van Way CW, Murphy JR, Dunn EL, Elerding SC. A feasibility study of computer aided diagnosis in appendicitis. Surg Gynecol Obstet. 1982; 155: 685-688.
- Dearmond GM, Dent DL, Myers J, Chopra S, Mumbower AL, Kumar A, et al. Appendicitis: Selective use of abdominal CT reduces negative appendicectomy rate. Surg Infect. 2003; 4: 213-218.
- Hong JJ, Cohn SM, Ekeh AP. Prospective Randomized study of clinical assessment versus computed tomography for the diagnosis of acute appendicitis. Surg Infect. 2003; 4: 231-239.
- Oliak D, Yamini D, Udani V. Non-operative management of perforated appendicitis without periappendiceal mass. Am J Surg. 2000; 179: 171-181.
- Margenthaler J, Longo W. Risk factors for adverse outcomes after the surgical treatment of appendicitis in adults. Ann Surg. 2003; 238: 59- 66.
- Y?ld?r?m E, Karagülle E, K?rba? I. Alvarado scores and pain onset in relation to multislice CT findings in acute appendicitis. Diagn Interv Radiol. 2008; 14: 14-18.
- Douglas CD, Macpherson NE, Davidson P. Randomised controlled trial of ultrasonography in diagnosis of acute appendicitis, incorporating the Alvarado score. BMJ. 2000; 321: 919-922.
- Fawcett T. ROC Graphs: Notes and Practical Considerations for Researchers. Technical report. Palo Alto (USA): HP Laboratories. 2004.
- Krishnan MG, Konwar R, Borgohain D. Modified Alvarado Scoring System in diagnosing acute appendicitis in a tertiary care centre in upper Assam. IOSR J Dental Med Sci. 2023; 22: 39-46.
- Shah MK, Doliya T, Chaudhary S, Khan S, Mallik S. Validation of the Ramathibodi Appendicitis Score for diagnosis of appendicitis in clinically suspected appendicitis patients: An observational study from Western India. Surg Chron. 2022; 27: 490-494.
- Ohle R, O’Reilly F, O’Brien K, Dimitrov BD. The Alvarado Score for predicting acute apendicitis: A sistematic Review. BMC Med. 2011; 9: 139-153.
- González GC, ZahdiI JOR, De Araujo Santos Nigro MV, Ramos-Junior O,Coelho GA. CORRELAÇÃO ENTRE A ESCALA DE ALVARADO E O GRAUDE INFLAMAÇÃO NA APENDICITE AGUDA. Rev Méd Paraná. Curitiba,2021; 79: 93-96.