Extended Lymph Dissection in Recurrent Colon Cancer - An Alternative to Chemotherapy.
- 1. Department of surgery, Naval hospital of Varna, Bulgaria
Abstract
Introduction: Local recurrences following radical resections of the colon are generally unlikely. The relapse is most often retroperitoneal; these are, in fact, unresolved during the operation regional lymphatic metastasis or distant lymph metastasis, such as retropancreatic, which do not enter the volume of operative intervention.
Case presentation: We present the case of a 52-year-old man operated in our clinic for recurrent colorectal cancer and we discuss lymphatic dissection in colon cancer and present enlarged lymph dissection and extirpation of retroperitoneal tumor as an alternative to chemotherapy and as a safe strategy for treatment in certain cases of relapse.
Conclusion: Survival in patients with local recurrence and peritoneal metastasis treated with systemic chemotherapy alone is extremely unsatisfactory and 5 years survival in patients with peritoneal metastasis of colorectal carcinoma treated only systemic chemotherapy is only achieved as an exception.
In such cases, extended lymphatic dissection is an alternative to chemotherapy, with very good close results and satisfactory distant results, especially in patients categorically refusing non-adjuvant or adjuvant chemotherapy
Citation
Nikolaev E, Nikolov N, Mankov N, Kostov D (2018) Extended Lymph Dissection in Recurrent Colon Cancer - An Alternative to Chemotherapy. JSM Gen Surg Cases Images 3(1): 1045.
INTRODUCTION
The number of metastatic lymph nodes is a significant factor determining survival. The significance of the total number of lymph node-derived lymph node dissections is also highlighted, the greater the number of lymphoid dissection lymph nodes, the greater the guarantee of accurate lymphatic status determination.
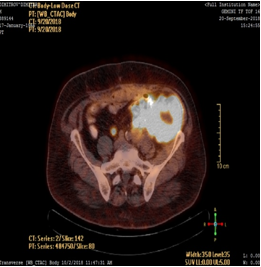
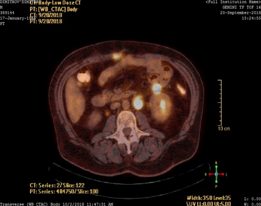
We report a case of a man who has suffered in the past by emergency resection of a colon sigmoideum for carcinoma. Due to the urgency of the disease (ileus) or because of the surgeon’s inexperience, standard lymphatic dissection (pT3NxMx) has not been performed. The patient came to us a few years after the first surgery with a large retroperitoneal tumor and several satellite tumor formations in the course of the large vessels found on PET scan (Figure 1,2).
Figure 1 Retroperitoneal tumor.
Figure 2 Satellite tumor formations in the course of the large vessels.
We performed extirpation of the retroperitoneal tumor with enlarged lymph dissection along the left aortic edge, the left iliac vessels, the left kidney vessels and the lower edge of the pancreas.
We discuss lymphatic dissection in colon cancer and present enlarged lymph dissection and extirpation of retroperitoneal tumor as an alternative to chemotherapy and as a safe strategy for treatment in certain cases of relapse.
BACKGROUND
In colon sigmoideum cancer, the lymphatic collector of the rectosigmoid region, the collector of whole colon sigmoideum and colon descendens is removed. This is achieved by ligating a. mesenteric inferior at the base, and v. mesenteric inferior under the pancreas. The presence of lymphogenic metastases at the base of a. mesenteric inferior also requires prophylactic paraaortal lymph dissection, and when there are paraaoraltal metastases, healing paraaorortal lymphatic dissection is made [1].
Local recurrences following radical resections of the colon are generally unlikely. The relapse is most often retroperitoneal; these are, in fact, unresolved during the operation regional lymphatic metastasis or distant lymph metastasis, such as retropancreatic, which do not enter the volume of operative intervention. According to data from Macintosh E [2] Reighley M [3] Makela J [4] retroperitoneal recurrences are from 1 to 8% after radical colon tumor operations.
Clinical trials in England and Germany have undoubtedly demonstrated that the surgeon’s qualifications and experience play a significant role in the recurrence rate of colorectal cancer. This factor can affect the effect of the operation by 30%, with the most experienced recurrences being 10%, while in the most inexperienced they are 40% [5]
CASE PRESENTATION
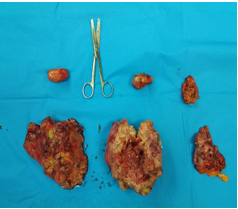
A 52 year old man, operated at our clinic for a 220/180mm retroperitoneal tumor, with the presence of enlarged lymph nodes in packs around the left iliac vessels, left of the aorta, around the left kidney vessels, the lower edge of the pancreas and the presence of a tumor formation on the anterior abdominal wall. The tumor was located retroperitoneally deeply on the left m. iliopsoas by infiltration of a mesocolon descendens and pushing it ventrally, infiltrated a middle third of the left ureter approximately 3 cm across, and pressed the left n. femoralis. Exploration did not reveal metastasis in the liver, but as a random finding a small 25 mm tumor was found in the jejunum about 20 centimeters under the ligament of Treitz. In the past, the patient has been operated sequentially for several years for carcinoma of sigmoid colon and carcinoma of the coecum (2010 - Hartmann sigmoid resection, right hemicolectomy in 2014). He has conducted 10 courses of adjuvant chemotherapy. Comes urgently due to strong and uncontrollable pain in the left hip area. The PET scan found a large retroperitoneal formation and several smaller satellite lesions along the large vessels and the pancreas. The patient definitely refused chemotherapy. He is operated after a short anti-allergic preparation. Intraoperatively, the retroperitoneal tumor and all lymph nodes along the vessels and the lower edge of the pancreas were removed, a part of the colon descendens, proximal rectum and the infiltrated part of the left ureter are resected, the wedge-shaped resection of the junum is performed, the tumor from the anterior abdominal wall is excised (Figure 3).
Figure 3 1 - a tumor with part of a left colon; 2 - retroperitoneal tumor; 3 - packet of paraaortal lymph nodes; 4 - pack of parailiac lymph nodes; 5 - pack of lymph nodes around the left renal vessels; 6 – pack of lymph nodes along the lower edge of the pancreas.
The patient was dehospitalised in very good condition on the 8th postoperative day. Histological analysis showed.
Investigations - PET scan
Treatment - Retroperitoneal tumor extirpation was performed in conjunction with a part of the m. iliopsoas sisnistra, a part of the left colon and a portion of the left ureter, as well as extended lymph dissection to remove all satellite lesions.
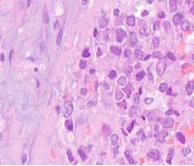
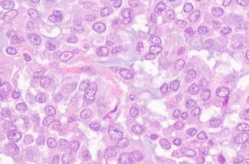
Histological analysis showed: fatty, fibrous and lymphatic tissue infiltrated by atypical cells, type, ring with stone“ with basophilic, mucus producing cytoplasm and vesicular nuclei with nest-forming nucleolus, solid sections and muddy lakes (about 20% of the cut surface) among which swim cells with morphology similar to the one described (Figure 4,5).
Figure 4 Histological analysis-I.
Figure 5 Histological analysis-II.
Histological diagnosis: Retroperitoneal mucus-producing adenocarcinoma (recurrence), infiltrating the colon, left ureter, retroperitoneal soft tissues and anterior abdominal wall. Metastases in the lymph nodes.
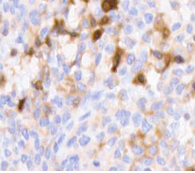
Immunohistochemistry examination:
- Tumor cells intensively express cytokeratin AE1/AE3; (Figure 6).
Figure 6 Tumor cells intensively express cytokeratin AE1/AE3.
- Lack of expression of synaptophysine; synaptophysin positive nerve fibers in the tumor tissue;
- Mild to moderate membrane expression of CD 138
Outcome and follow up: Complete recovery of the patient was observed after the operation and complete recovery after 6 weeks of follow-up.
DISCUSSION
Colorectal cancer is the third most frequent and fourth as the cause of cancer death globally [6]. Among the main causes of failed treatment and lethal outcome of colorectal cancer are local recurrences and peritoneal metastases. The volume of lymphatic dissection in colon cancer is relatively little discussed in the literature. It is noted that the volume of resection at the various tumor localizations is usually dependent on the specificity of lymphatic metastasis and on this basis are generally accepted standards, rarely including pools outside the mesenteric basin [1,7].
As a standard surgery for sigmoid cancer, it is recommended to resection the entire sigma and parts of the proximal rectum and the distal part of the colon descendens. A. mesenterica inferior is ligated to the base or after the separation of a. colica sinistra. If you keep part of a. mesenterica inferior lymphatic dissection is performed around it. Thus, both variants are equally oncologically endorsed. V. mesenterica inferior is always ligated high up to the edge of the pancreas [7].
In Japan extended lymphatic dissection was accepted as a standard tactic since 1976. According to the rules of the Japanese Society of Colorectal Cancer, it is recommended to extend lymphatic dissection to the extra-mesenteric lymph nodes. Regarding the use of adjuvant chemotherapy, patients with extended lymphadectomy in Japanese authors pretended not to do this, as lymphadenectomy was assumed to provide a sufficient degree of local control of the disease [8,9].
FOLFOX is currently a standard for adjuvant treatment in patients with resected colon carcinoma. Survival in patients with local recurrence and peritoneal metastasis treated with systemic chemotherapy alone is extremely unsatisfactory. Modern chemotherapy regimens, including biological agents in treatment protocols, are effective in metastatic colorectal carcinoma without peritoneal metastasis and result in some prolongation of survival in the presence of peritoneal metastases but 5 years survival in patients with peritoneal metastasis of colorectal carcinoma treated only systemic chemotherapy is only achieved as an exception.
When performing extensive lymphatic dissection, a number of operational and technical requirements must be observed to minimize the complications of the genitourinary system. In the absence of the necessary experience, the patient may be in the risk of recurrence.
Nobody doubts that lymph node dissection in colon cancer is needed; only the extent of this dissection is still under discussion. Since the individual stages of the oncology operation cannot be separated from each other, the analysis of the significance of lymph node dissection is difficult. It has been shown that the T category is directly related to the number and central distribution of lymph node metastasis. Micro-metastasis and isolated tumor cells can be detected in the lymph nodes by using special coloring techniques; their presence can significantly worsen the prognosis and bring it closer to UICC’s Stage III. The number of dissected lymph nodes and the ratio of lymph nodes with metastases to the total number of dissected lymph nodes were used as markers for the quality of the performed operation and a histopathological assessment. Recent results highlight the importance of technique and size of dissection. The mesocolon dissection should be performed in an embryonic plan without disrupting its integrity. In order to achieve the best oncology results while maintaining the quality of life, it is necessary to discontinue the vessels over fascia endoabdominalis for the maintenance of the central hypogastric nerves. Extensive lymphadenectomy is only oncology relevant when combined with removal of the primary tumor with adequate lengthening clearance, intact mesocolon and complete vascular pedicle to minimize the risk of tumor cell scarring and local recurrence [10].
CONTRIBUTORS
DG was the responsible consultant and operating surgeon along with SDC. All the authors were involved in elements of writing, and editing and submitting of this case.