Breaking Barriers to Heart Health: Harnessing the Power of Natural Products and Lifestyle Interventions in Combating Cardiovascular Disease
- 1. Department of Bioscience and Biotechnology, Banasthali Vidyapith, India
Abstract
Cardiovascular diseases (CVD) are the leading cause of mortality and morbidity worldwide, significantly contributing to the global burden of disease. CVD encompasses disorders of the heart and blood vessels, including coronary heart disease, heart failure, arrhythmia, myocardial infarction, and hypertension. While traditional risk factors such as genetics, hypertension, and hyperlipidemia are crucial, unhealthy lifestyle choices-including diets high in refined carbohydrates, fats, and salt, physical inactivity, smoking, excessive alcohol consumption, stress, and poor sleep habits-are major modifiable contributors to CVD. These factors promote conditions like atherosclerosis, where fatty deposits accumulate on arterial walls, restricting blood flow and causing serious cardiovascular complications.
This review examines the impact of lifestyle interventions-dietary modifications, physical activity, smoking cessation, and stress management-on cardiovascular health and their integration into routine practice. Heart-healthy diets like the Mediterranean and DASH patterns effectively reduce blood pressure, improve lipid profiles, and mitigate inflammation. Regular physical activity strengthens the heart, improves endothelial function, reduces arterial stiffness, and aids in weight management. Smoking cessation reverses many harmful cardiovascular effects of tobacco use, while stress management techniques such as mindfulness and cognitive-behavioural therapy alleviate the impact of chronic stress.
Despite these benefits, socio-economic disparities, cultural influences, and limited healthcare access hinder widespread adoption of these interventions. Public health strategies must create supportive environments through community programs, policy initiatives, and healthcare interventions. This review underscores the need for integrating lifestyle modifications with traditional medical therapies to globally reduce CVD risk and improve public health outcomes.
KEYWORDS
- Cardiovascular disease; Lifestyle choices, Prevention; Diet; Exercise; Smoking cessation; Stress management
CITATION
Dubey A, Rajpoot A, Sharma V (2025) Breaking Barriers to Heart Health: Harnessing the Power of Natural Products and Lifestyle Interven- tions in Combating Cardiovascular Disease. J Cardiol Clin Res. 13(2): 1214.
INTRODUCTION
Cardiovascular disease (CVD) encompasses a range of conditions affecting the heart and blood vessels, making it the leading cause of death worldwide. In India, CVD accounts for one-third of all deaths, with 220 million individuals suffering from high blood pressure, and only 12% effectively managing the condition [1]. Globally, CVD prevalence is rising, with young adults increasingly at risk due to factors like smoking, unhealthy diets, stress, and physical inactivity. Table 1 highlights the worldwide prevalence of CVD.
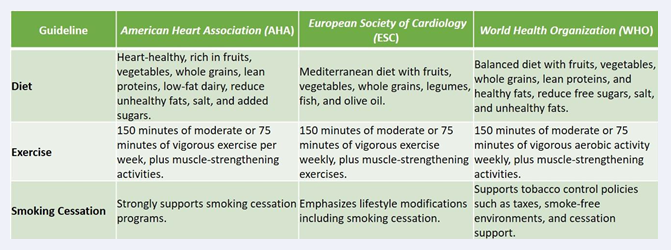
Table 1: Top Determinants of Cardiovascular Deaths and DALYs Worldwide in 2021 [1]
In the 21st century, CVD is a major cause of mortality and disability, particularly among individuals aged 65 and older. Poor lifestyle choices, including excessive alcohol consumption, smoking, and high-sugar diets, exacerbate CVD risk. A sedentary lifestyle and obesity further contribute to the burden. The type of diet directly influences cardiovascular health. For instance, the DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, and whole grains while low in saturated fats, significantly lowers CVD risk. Vegetarian diets are also beneficial, as they contain less cholesterol and saturated fat compared to omnivorous diets [2].
Although medications are critical for managing CVD, they can cause side effects like gastrointestinal issues, weight gain, and hypertension. Overuse of corticosteroids and nonsteroidal anti-inflammatory drugs can exacerbate these risks, necessitating careful management. A holistic approach combining heart-healthy eating, regular physical activity, smoking cessation, stress management, and routine health monitoring is essential for reducing CVD risk and improving outcomes. CVD includes conditions like coronary heart disease (CHD), heart failure, arrhythmias, cerebrovascular disease, and congenital heart defects. CHD, the most common form, results from atherosclerosis- arterial narrowing caused by fatty deposits and cholesterol- leading to reduced blood flow to the heart [3]. Symptoms include chest pain, fatigue, and heaviness. Heart failure, a chronic condition, occurs when the heart cannot pump enough blood to meet the body’s oxygen demands, causing fatigue, weakness, and shortness of breath. Alcohol- induced cardiomyopathy, often affecting women more severely, alters heart shape and function due to prolonged alcohol consumption. Arrhythmias, characterized by irregular heart rhythms, result from electrical signal disruptions in the heart.
Addressing CVD through lifestyle modifications and integrated care offers a pathway to reduced mortality and enhanced quality of life.
Risk factors for cardiac pathogenesis
There is major risk factors associated with CV-related issues. Behavioral factors include poor diet, high sodium intake, smoking, tobacco, and alcohol consumption. Metabolic factors, including elevated blood glucose, low HDL cholesterol, high LDL cholesterol, and raised blood pressure, are more prevalent in males than females. Obesity is the only risk factor that is more prevalent in women than in men. Environmental factors include polluted air, soil, and contaminated water caused by urbanization. South Asian countries have some of the highest levels of ambient air pollution. Although these factors are modifiable, others, including gender, family history, and age, are non- modifiable.
The distribution of cardiovascular risk factors differs by sex. For instance, smoking rates are highest in South Asia, East Asia, and Oceania, while among women, and it is most prevalent in high-income countries. Obesity rates are highest among women in North Africa and the Middle East, while men in Southeast Asia, East Asia, and Oceania have the highest rates. According to the World Health Report 2023 [4], modifiable risk factors contributing to cardiovascular disease-related deaths in 2021 include:
- 3.8 million deaths due to raised LDL cholesterol
- 2.3 million deaths caused by high fasting plasma glucose levels
- 4.8 million deaths due to air pollution
- 2.0 million deaths due to high body mass index
- 3.0 million deaths due to high tobacco consumption
- 397,000 deaths due to low physical activity
Global Burden of Cardiovascular Diseases and Key Determinants
In 2021, cardiovascular diseases (CVDs) continued to be the leading cause of global deaths and disability- adjusted life years (DALYs). Key determinants contributing to this burden included elevated LDL cholesterol, high fasting glucose levels, obesity, air pollution, and tobacco consumption. LDL cholesterol alone accounted for approximately 3.8 million deaths globally, highlighting its critical role in increasing CVD risk [6]. High fasting plasma glucose levels and air pollution were linked to 2.3 million and 4.8 million deaths, respectively, while obesity, measured by body mass index (BMI), contributed to 2.0 million deaths. Tobacco consumption remained a significant risk factor, causing approximately 3.0 million deaths.
Ischemic heart disease (IHD), also known as coronary heart disease, emerged as the leading cause of cardiovascular mortality worldwide. It results from the narrowing of coronary arteries, impeding blood flow to the heart muscle and significantly elevating the risk to health. IHD was responsible for 9.1 million deaths in 2019 alone, accounting for about 33% of global cardiovascular-related deaths [7]. This condition’s burden is particularly high in low- and middle-income countries (LMICs), where access to healthcare and preventive measures is limited, and lifestyle-related factors play a major role in its prevalence.
The burden of CVD was disproportionately higher in LMICs, where 80% of all CVD-related deaths occurred [8]. This disparity is exacerbated by aging populations and increasing exposure to modifiable risk factors like poor diet, physical inactivity, smoking, and air pollution. Regions such as Central and Eastern Europe and Central Asia experienced some of the highest death rates from CVDs [9]. To combat CVD globally, public health efforts must focus on addressing these key risk factors through initiatives promoting healthier lifestyles, reducing tobacco use, mitigating air pollution, and improving healthcare access. Table 1 provides top Determinants of Cardiovascular Deaths and DALYs Worldwide in 2021.
National Program for the Prevention and Management of Non-Communicable Diseases (2023–2030): Focus on Cardiovascular Disease
Non-Communicable Diseases (NCDs) encompass long- term illnesses that are not transmissible from person to person. This category includes conditions such as diabetes, cancer, hypertension, cardiovascular diseases, chronic kidney diseases, chronic obstructive pulmonary disease (COPD), asthma, fatty liver disease, and other related disorders. Among these, cardiovascular diseases (CVDs) remain a significant and urgent concern.
NCDs are a leading cause of out-of-pocket medical expenses in India, with their financial burden projected to reach $3.55 trillion between 2012 and 2030, excluding mental health issues. Addressing this, the Sustainable Development Goals (SDGs) aim to reduce premature deaths from NCDs by one-third globally by 2030. In alignment with these goals, emphasis is placed on preventing and managing alcohol and tobacco use, two critical risk factors for CVDs.
Cardiovascular diseases are the leading cause of death in India, accounting for 27% of all fatalities, as highlighted in the WHO NCD India Profile (2018). Percentage Share of Various Non-Communicable Diseases provides a visual representation of the distribution of NCD-related fatalities in India (Figure 1).
Figure 1: Percentage Share of Various Non-Communicable Diseases [10]
Additionally, NCDs are projected to account for 63% of total deaths nationwide. Data from the India State-Level Disease Burden Initiative CVD Companions (2016), reveals approximately 55 million cases of cardiovascular disorders, including 23.8 million ischemic heart disease cases and about 6 million stroke cases. Cardiovascular illnesses contributed to 28.1% of total deaths in 2016 [10].
This emphasizes the critical need for a comprehensive approach under the 2023–2030 national program to reduce the burden of NCDs, particularly cardiovascular diseases, through prevention, management, and addressing lifestyle-related risk factors.
Hypertension: Hypertension, or elevated blood pressure, arises from excessive force exerted by blood against arterial walls. It is classified as Primary (Essential) or Secondary. A diagnosis is confirmed when diastolic blood pressure is ≥90 mmHg and systolic blood pressure is ≥140 mmHg across two separate readings. Hypertension affects approximately 33% of the global population, with 1.28 billion individuals aged 30 to 79 impacted.
Although often asymptomatic, severe hypertension may cause fatigue, nausea, headaches, nosebleeds, irregular heartbeats, and vision disturbances. Management includes medication, lifestyle adjustments, and salt reduction. If left uncontrolled, hypertension can lead to severe conditions such as kidney failure, heart attacks, and strokes [10].
Stroke: India reports 700,000 stroke-related deaths and 1.17 million cases annually. Most strokes are preventable through lifestyle modifications, telemedicine, early diagnosis, and community awareness. Educating the public about the BE FAST approach-Balance loss, Eyesight changes, facial drooping, arm weakness, and dysphasia— can reduce stroke incidence and severity. Timely emergency intervention is crucial. Treatment options include antiplatelet medications, thrombolytics, surgery, and physical therapy [10].
ST-Elevation Myocardial Infarction (STEMI): Stroke and ischemic heart disease account for 80% of cardiovascular disease cases in India, contributing to 28.1% of all deaths. Ischemic heart disorders also represent 8.7% of Disability Adjusted Life Years (DALYs) and 14.1% of cardiovascular diseases. Approximately 40% of myocardial infarctions are STEMIs, identifiable via ECG changes. Risk factors include hypertension, diabetes, smoking, obesity, hyperlipidemia, poor diet, and excessive alcohol intake. Men are twice as likely as women to experience STEMIs. Early treatment, such as thrombolysis and Percutaneous Coronary Intervention (PCI), is vital for restoring blood flow and saving lives [10].
Effect of Diet on Cardiovascular Wellness
A healthy dietary pattern significantly reduces risk factors associated with cardiovascular disorders. Conversely, an improper diet is strongly linked to poor cardiovascular health. Common dietary mistakes include irregular eating habits, excessive intake of unhealthy fats and sweets, and inadequate consumption of dietary fiber, unsaturated fatty acids, and legumes. Studies emphasize the importance of dietitians and nutritional education to curb the rising prevalence of CVDs. A balanced, diverse diet ensures adequate intake of heart-healthy nutrients [11].
Carbohydrates: Excessive intake of simple carbohydrates, such as sugar, sweets, and high-glycemic index foods, elevates CVD risk. The WHO recommends limiting simple carbohydrates to no more than 10% of total caloric intake and prioritizing complex carbohydrates, low-glycemic index foods, and dietary fibers instead.
Dietary Fiber: Dietary fiber includes soluble and insoluble plant-based substances digestible by probiotic bacteria in the gastrointestinal tract. WHO recommends consuming 27–40 grams of fiber daily for substantial cardiovascular benefits. Adequate fiber intake helps prevent hypertension, reduces visceral fat, improves insulin sensitivity, and promotes healthier LDL cholesterol levels by limiting cholesterol absorption in the gastrointestinal tract.
Fats: High consumption of trans fats and insufficient intake of polyunsaturated fatty acids (PUFAs) are linked to increased CVD risk. Trans fats, mainly from highly processed foods, contribute to elevated cholesterol levels and higher diastolic blood pressure, increasing CVD- related mortality. Conversely, essential PUFAs restore metabolic balance, reduce oxidative stress, and offer anti- inflammatory benefits that protect vascular health.
Ultra-Processed Foods (UPFs): UPFs, designed for enhanced shelf life and palatability, contain additives like colorants, stabilizers, emulsifiers, and sweeteners. They account for 57% of energy intake among U.S. adults. UPFs contribute to CVD risk through harmful fats, added sugars, excess sodium, and caloric overload. Moreover, UPFs are associated with glucometabolic disruptions, gut microbiota alterations, inflammatory processes, diabetes, endothelial dysfunction, and cardiac tissue damage. These effects are linked to compounds such as acrylamide, monosodium glutamate, bisphenol-A, and advanced glycation end products. Cohort studies from the U.S. and Europe consistently demonstrate a positive correlation between UPF consumption and CVD risk [12].
Cardio protective food ingredients
Certain foods have specific cardioprotective effects. Including them in the diet can help prevent the onset of CVDs and improve health in those already affected. Several cardioprotective food components are listed in the Figure 2, with their roles and sources [11].
Figure 2: Specific cardiovascular-protective ingredients [11]
Recommended nutritional strategies in the prevention and treatment of cardiovascular disease
Extensive research has demonstrated that the Mediterranean and DASH diets are highly beneficial for heart health. Here is an overview of the research validating these diets, along with additional dietary approaches [13].
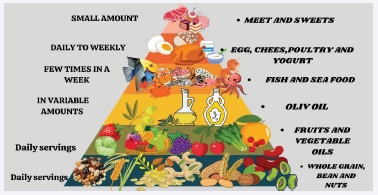
Mediterranean diet: It is a traditional dietary pattern of Mediterranean countries like Greece, Italy, and France. This diet is characterized by a variety of plant-derived foods like fruits, vegetables, whole grains, legumes, nuts, and seeds, with olive oil as the main fatty food source. It recommends fish and poultry are consumed in moderation, while red meat is kept to a minimum (Figure 3).
Figure 3: Mediterranean Diet Pyramid - A Visual Guide to Balanced, Healthy Eating
According to the PREDIMED study, a Mediterranean diet that is focused on the abundant consumption of extra-virgin olive oil or a variety of mixed nuts reduced cardiovascular risk by 30% compared to low-fat diets [12].
The omega-6 and omega-3 fatty acids, along with plant sterols found in nuts, including almonds, walnuts, hazelnuts, and pine nuts, help lower LDL cholesterol and reduce the risk of heart disease, making them a heart- healthy addition to the diet. Research suggests that weekly consumption of nuts leads to a 40% to 60% reduction in CVD risk. Additionally, foods with a low glycemic index and rich in fiber can lower insulin production and boost short- chain fatty acid levels, which inhibit cholesterol production. Research shows five key benefits of the Mediterranean diet: it lowers lipid levels, Defends against oxidative stress, inflammation, and platelet clumping. Due to its richness in cardioprotective components, this diet significantly reduces cardiovascular disease risk [11].
Dash diet: The dietary approach to preventing hypertension is rich in nutrients such as calcium, magnesium, and fiber, and devoid of saturated fats, with a balanced amount of protein. Several studies indicate its effectiveness in managing multiple CVD risk factors, including hypertension, dyslipidemia, and glucose intolerance. The DASH diet is abundant in fruits, green leafy vegetables, poultry, fish, nuts, and legumes, while it restricts red meat and promotes low-fat dairy products and whole grains over refined grains, minimizing sweet food consumption. Research shows that the DASH diet also improves lipid level and reduces the likelihood of CVDs and type 2 diabetes. Higher consumption of whole grains, green vegetables, and beans helps reduce cardiovascular disease risk by 60%, 45%, and 65%, respectively [14].
Plant-based diet: Research indicates that vegetarian and vegan diets, as examples of plant-based eating, help minimize cardiovascular health risks. Studies show that individuals following this diet have reduced blood pressure, enhanced lipid profiles, weight loss, and a decreased chances of ischemic heart disease contrasted to those on animal-based diets. The EPIC-Oxford studies suggest that plant-based eaters have 13% reduced likelihood of ischemic heart disease than non-vegetarians [13].
Dietary Factors Associated with Cardiovascular Disease
Certain dietary components have been linked to an elevated risk of cardiovascular disease (CVD). While these elements can be part of a balanced diet when consumed in moderation, excessive intake may contribute to CVD. Key factors associated with increased CVD risk include:
Saturated fat: Found in animal products like red meat, butter, and cheese, saturated fat is linked to increased total cholesterol and LDL cholesterol, which raise CVD risk. Consuming high amounts of saturated fat can negatively impact heart health by increasing LDL cholesterol in the blood, leading to atherosclerosis, which is the accumulation of plaque in the arteries. According to the American Heart Association saturated fats should contribute no more than 6% of total daily calories, or 11–13 grams per day, is typical for a 2,000-calorie diet.
Sodium: A diet high in salt increases CVD risk. Sodium is commonly found in table salt, processed foods, and restaurant meals. While sodium is essential for maintaining blood pressure, excessive intake may lead to cardiovascular issues, including heart attacks and strokes. The AHA advises limiting sodium to 1,500 mg per day for those with high blood pressure.
Trans fats: Processed foods and fried meals are high in trans fats, which increase CVD risk. Trans fats adversely affect total and LDL cholesterol and are even more harmful than saturated fats. Trans fats are formed through the process of partially hydrogenating vegetable oils to increase shelf longevity. The AHA recommends avoiding trans fats whenever possible by minimizing processed food consumption and choosing a diet abundant in fruits, vegetables, whole grains, lean proteins, and healthy fats.
Added sugars: Added sugars in many sugary foods and drinks can cause insulin resistance, rise in weight, and high blood pressure. Common sources such as granulated sugar, brown sugar, and high-fructose corn syrup, present in soft drinks, candies, and baked goods, contribute to a higher risk of cardiovascular diseases. The AHA advises a daily limit of 36 grams of added sugar for men and 25 grams for women.
Lifestyle, Biological, and Environmental Factors Impacting Cardiovascular Health
Cardiovascular health is shaped by a combination of lifestyle choices, biological factors, and environmental exposures. Factors like diet, physical activity, smoking, and alcohol intake affect cardiovascular risk by influencing lipid profiles, blood pressure, and inflammation. Genetic predispositions, age, and hormonal variations also impact susceptibility to cardiovascular diseases (CVDs). Additionally, environmental factors such as pollution, heavy metals, and second hand smoke contribute to oxidative stress and inflammation, accelerating vascular damage. These interconnected factors highlight the importance of a comprehensive approach to CVD prevention and management [15].
The Impact of Gut Microbiota on Heart Disease: The human intestine hosts a large number of bacteria collectively known as the gut microbiota. Its composition is influenced by host factors, dietary choices, genetic variations, and antibiotic use. In healthy individuals, the gut microbiota includes a balance of beneficial and limited harmful bacteria, supporting overall health. Disease conditions can disrupt this balance, reducing beneficial bacteria and increasing harmful ones. Increased dietary fiber intake has been linked to greater microbiota diversity, which correlates with reduced hypertension and cardiovascular disease (CVD) risk [16].
The impact of Smoking on Heart Health and Blood Pressure: According to the WHO, smoking contributes to approximately 10% of cardiovascular diseases (CVDs), causing around 6 million deaths annually worldwide, including 500,000 in the United States. Of these deaths, 10% result from second hand smoke exposure. Smokers, as well as those exposed to second hand smoke, are at risk. Women who smoke face a 25% higher risk of coronary heart disease compared to men with similar tobacco exposure [18]. Smoking elevates blood pressure, a key risk factor for heart disease. The nicotine in cigarettes activates the renin-angiotensin-aldosterone system (RAAS), leading to temporary increases in blood pressure. This sympathetic response can raise blood pressure for up to 15 minutes post-smoking [16].
The Role of Gender in Smoking-Related Chronic Diseases: Women who smoke are at a greater risk of cardiovascular complications at an earlier age than male smokers. Smoking increases the risk of ischemic stroke, peripheral arterial disease, and carotid atherosclerosis in women. Quitting smoking reduces these risks within 1–2 years [18].
Smoking Cessation and Its Impact on Cardiovascular Health: Quitting smoking helps reverse many cardiovascular risks by improving blood vessel function, lipid profiles, and reducing inflammation and oxidative stress [12].
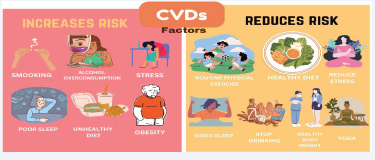
Alcohol Consumption and Cardiovascular Health: Alcohol intake, particularly in regions like Southeast Asia, East Asia, and Oceania, can affect cardiovascular health. Low-to-moderate consumption has been linked to improved HDL cholesterol and reduced platelet aggregation, offering cardioprotective benefits. However, excessive drinking exacerbates oxidative stress, inflammation, and hypertension, contributing to conditions like atherosclerosis [19,20] (Figure 4).
Figure 4: Risk and protective factors for cardiovascular health
The role of physical exercise in cardiovascular health
Physical activity includes any bodily movement involving muscle contraction that elevates energy expenditure beyond resting levels. Exercise is one aspect of a person’s complete physical activity, which should be carefully planned and organized [19].
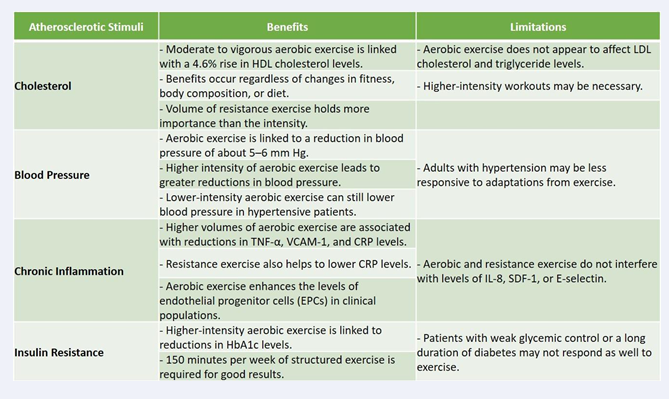
Impact of exercise on atherosclerosis: Atherosclerosis is characterized by the buildup of lipids and fibrous components in the endothelial layer, particularly in larger coronary arteries. The process begins when LDL particles leak through a damaged endothelial layer into the subendothelial region, where they oxidize and acquire proatherogenic properties. This triggers the upregulation of adhesion molecules, such as VCAM-1, E-selectin, and P-selectin, promoting the recruitment of monocytes and T cells. Monocytes adhere to endothelial cells, migrate into the subendothelial area, and engulf oxidized LDL particles, transforming into foam cells-an early asymptomatic stage of atherosclerosis [5] (Table 2).
Table 2 Impact of Exercise on Atherosclerotic Risk Factors – Benefits and Limitations [20].
As the disease advances, an immune-inflammatory response leads to fibroproliferation driven by smooth muscle cells, which generate a collagen-rich matrix to protect against plaque rupture and thrombosis. However, ongoing atherogenic stimuli may cause vessel stiffening, narrowing of the lumen, and ischemia [20]. Physical exercise has been shown to positively influence the blood lipid profile, improving lipid metabolism and reducing inflammation, thus mitigating atherosclerosis. However, overtraining and oxidative stress may exacerbate vascular damage [21] (Figure 5).
Figure 5: Benefits of physical exercise in older adults [21]
Resistance Training: Resistance training, which uses weights to enhance muscular strength and endurance, also benefits cardiovascular health by reducing resting blood pressure, increasing HDL cholesterol, and improving insulin sensitivity [22]. It improves body composition by boosting muscle mass and reducing body fat. Combining resistance training with aerobic exercise further enhances heart health, with both exercises recommended at least twice a week [13]. Though the exact mechanisms are not fully understood, evidence suggests that exercise helps muscles utilize lipids as a primary energy source, reducing plasma lipid levels [23]. Increases in HDL cholesterol from exercise can counterbalance high LDL cholesterol and triglyceride levels, though higher-intensity aerobic exercise may be required for significant changes in LDL and triglycerides [24]. Regular physical activity offers multiple benefits for older adults, improving cardiovascular health, muscle strength, and mobility, which contributes to a better quality of life [20].
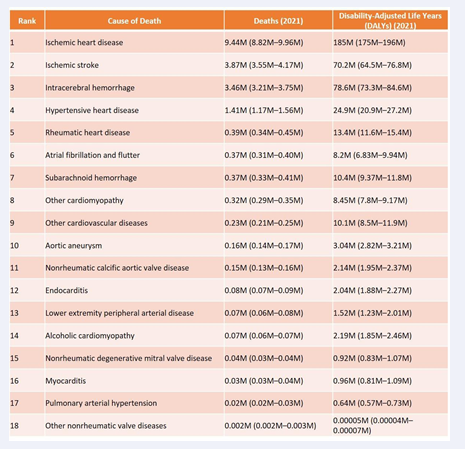
Current recommendations and guidelines for lifestyle modification aimed to improve heart health adapted from AHA, ESC, WHO Guidelines on Cardiovascular Health, is presented in Table 3 [24,25].
Table 3: Guidelines on Diet, Exercise, and Lifestyle for Cardiovascular Health
CONCLUSION AND FUTURE PROSPECTIVE
In conclusion, transforming cardiovascular health through lifestyle changes is both essential and achievable. The reviewed literature reveals strong links between diet, physical activity, smoking cessation, and stress management with reduced cardiovascular disease (CVD) risk. Diets rich in fruits, vegetables, whole grains, and healthy fats are consistently associated with improved heart health, while regular exercise enhances heart function and reduces hypertension. Quitting smoking significantly lowers the risk of CVD, and effective stress management minimizes its harmful effects. Public health campaigns should raise awareness and support these lifestyle changes. Future research should explore strategies to promote and sustain these behaviors across diverse communities. In the future, cardiovascular disease prevention will benefit from personalized medicine, advanced technologies, and addressing broader social factors. Genomics, biomarkers, and wearable technologies will allow for tailored interventions, enabling more effective, data-driven approaches to CVD prevention and improved outcomes for high-risk populations.
Author Contributions
- Veena Sharma: Conceptualization, primary writing, formatting, literature search, methodology development, preparation of the initial draft, and supervision.
- Anjali Dubey: Writing, critical editing, refinement of drafts, reference management, and manuscript review.
- Anjali Rajpoot: Writing, editing, visualization, and overall manuscript refinement.
REFERENCES
- Venugopal V, Richa R, Singh D, Gautam A, Jahnavi G. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke: A Scoping Review in the Context of Hypertension Prevention and Control in India. Indian J Public Health. 2023; 67: S50-S57.
- Sharifi-Rad J, Rodrigues CF, Sharopov F, Docea AO, Can Karaca A, Sharifi-Rad M, et al. Diet, lifestyle and cardiovascular diseases: linking pathophysiology to cardioprotective effects of natural bioactive compounds. Int J Env Res Public Health. 2020; 17: 2326.
- Kaiser J, van Daalen KR, Thayyil A, Reis MTDAR, Caputo D, Oliver- Williams C. A systematic review of the association between vegan diets and risk of cardiovascular disease. J Nutr. 2021; 151: 1539- 1552.
- World Heart Report 2023: Confronting the World’s Number One Killer. Geneva, Switzerland. World Heart Federation. 2023. Bohara SS, Thapa K, Bhatt LD, Dhami SS and Wagle S (2021) Determinants of Junk Food Consumption Among Adolescents in Pokhara Valley, Nepal. Front Nutr. 2021; 8: 644650.
- Rajpoot A, Aggarwal T, Sharma V. Unraveling the Enigma of Cardiac Damage Caused by Lead: Understanding the Intricate Relationship between Oxidative Stress and Other Multifactorial Mechanisms. Toxicology. 2024.
- Huimin Chen, Lu Liu, Yi Wang, Liqiong Hong, Wen Zhong, Thorsten Lehr, et al. Burden of cardiovascular disease attributable to metabolic risks in 204 countries and territories from 1990 to 2021. Eur Heart J. Quality of Care and Clinical Outcomes. 2024, qcae090.
- Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi SKBM, AlKatheeri R, et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus. 2020; 12: e9349.
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020; 76: 2982-3021.
- Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low-and middle-income countries: a systematic review. BMC Public Health. 2018; 18: 975.
- NATIONAL PROGRAMME FOR PREVENTION AND CONTROL OF NON-COMMUNICABLE DISEASES (2023-2030) Ministry of Health & Family Welfare Government of India. 2023
- Szczepa?ska E, Bia?ek-Dratwa A, Janota B, Kowalski O. Dietary Therapy in Prevention of Cardiovascular Disease (CVD)—Tradition or Modernity? A Review of the Latest Approaches to Nutrition in CVD. Nutrients. 2022; 14: 2649.
- Mendoza K, Smith-Warner SA, Rossato SL, Khandpur N, Manson JE, Qi L, et al. Ultra-processed foods and cardiovascular disease: analysis of three large US prospective cohorts and a systematic review and meta-analysis of prospective cohort studies. The Lancet Regional Health–Americas. 2024; 37.
- Ghodeshwar GK, Dube A, Khobragade D, Dube AH. Impact of lifestyle modifications on cardiovascular health: a narrative review. Cureus. 2023; 15.
- Said MA, Verweij N, van der Harst P. Associations of Combined Genetic and Lifestyle Risks with Incident Cardiovascular Disease and Diabetes in the UK Biobank Study. JAMA Cardiol. 2018; 3: 693-702.
- Diab A, Dastmalchi LN, Gulati M, Michos ED. A Heart-Healthy Diet for Cardiovascular Disease Prevention: Where Are We Now? Vascular Health and Risk Management. 2023; 19: 237-253.
- Liu H, Zhuang J, Tang P. The Role of the Gut Microbiota in Coronary Heart Disease. Curr Atheroscler Rep. 2020; 22: 77.
- Luehrs RE, Zhang D, Pierce GL, Jacobs Jr, DR, Kalhan R, Whitaker KM. Cigarette smoking and longitudinal associations with blood pressure: the CARDIA study. J Am Heart Association. 2021; 10: e019566.
- Gallucci G, Tartarone A, Lerose R, Lalinga AV, Capobianco AM. Cardiovascular risk of smoking and benefits of smoking cessation. J Thorac Dis. 2020; 12: 3866-3876.
- Metsios GS, Moe RH, van der Esch M. The effects of exercise on cardiovascular disease risk factors and cardiovascular physiology in rheumatoid arthritis. Rheumatol Int. 2020; 40: 347-357.
- Dobrosielski DA. How can exercise reduce cardiovascular disease risk? A primer for the clinician. Pol Arch Intern Med. 2021; 131: 10- 20452.
- Cium ?arnean L, Milaciu MV, Negrean V. Cardiovascular Risk Factors and Physical Activity forthe Prevention of CardiovascularDiseases in the Elderly. Int J Environ Res Public Health 2022; 19: 207.
- Sharma KNS, Pailoor S, Choudhary NR, Bhat P, Shrestha S. Integrated Yoga Practice in Cardiac Rehabilitation Program: A Randomized Control Trial. J Altern Complement Med. 2020; 26: 918-927.
- Guddeti RR, Dang G, Williams MA, Alla VM. Role of yoga in cardiac disease and rehabilitation. J Cardiopulm Rehabil Prev. 2019; 39: 146- 152.
- Noubiap JJ, Nyaga UF. Cardiovascular disease prevention should start in early life. BMC Glob Public Health. 2023; 1: 14.
- Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021; 143: e984-e1010.
![Figure 1 Percentage Share of Various Non-Communicable Diseases [10]](https://www.jscimedcentral.com/public/assets/images/uploads/image-1749534642-1.PNG)
![Figure 2 Specific cardiovascular-protective ingredients [11]](https://www.jscimedcentral.com/public/assets/images/uploads/image-1749534679-1.PNG)
![Figure 5 Benefits of physical exercise in older adults [21]](https://www.jscimedcentral.com/public/assets/images/uploads/image-1749534762-1.PNG)