Intracardiac Masses: Epidemiological, Clinical, Therapeutic and Evolutionary Aspects in a Cardiology Department in Sub-Saharan Africa
- 1. Department of Cardiology, Bogodogo University Hospital, Burkina Faso
- 2. Department of Cardiology, Yalgado OUEDRAOGO University Hospital, Burkina Faso
Abstract
Introduction/Objective: Intracardiac masses include thrombi, cardiac tumours and valvular vegetations. The aim of this study was to describe the epidemiological, clinical, therapeutic and evolutionary aspects of intra-intracardiac masses in a cardiology department in sub-Saharan Africa.
Patient and method: This was a three-month cohort study in the Yalgado Ouedraogo cardiology department. All patients diagnosed and hospitalised with intracardiac masses were included in the study. Sociodemographic, clinical, paraclinical, therapeutic and prognostic variables were collected. Qualitative and quantitative variables were assessed in terms of frequency and mean plus or minus standard deviation. Comparison of means and percentages was performed using Pearson’s Chi2 test with a significance level of p = 0.05.
Results: The hospital incidence of intracardiac masses was 7.5%. Diabetes was found in six patients (7.6%) and arterial hypertension in 57 patients (71.3%). The main aetiologies were dilated cardiomyopathy in 28.8% (n=23) of cases, ischaemic heart disease in 10% (n=8), and peripartum cardiomyopathy in 3.8% (n=3). Treatment consisted of anticoagulants in 65% of cases, antibiotics in 58.8% of cases and instrumental treatments in 1.3% of cases. The mortality rate was 18.5%. The causes of death during hospitalisation were thrombo-embolic complications (30%), uncontrolled heart failure (81.3%), cardiogenic shock (25%) and septic shock (20%).
Conclusion: Intracardiac masses are serious because of their high mortality rate. The most frequent were thromboses. They therefore require prolonged monitoring in order to preserve the patient’s survival.
Keywords
• Intracardiac masses
• Thrombus
• Vegetations
• Myxoma
• Ouagadougou
Citation
Thiombiano LP, Nacanabo WM, Zonou PNS, Kagembega LJ, Kontogom S, et al. (2025) Intracardiac Masses: Epidemiological, Clinical, Thera peutic and Evolutionary Aspects in a Cardiology Department in Sub-Saharan Africa. J Cardiol Clin Res. 13(1): 1211
INTRODUCTION
Intracardiac masses (ICMs) are frequent and serious complications of many heart diseases, including valvular, dilated, ischaemic and rhythmic heart disease. They may be discovered incidentally or during the investigation of a stroke or fever [1,2]. They include intracardiac thrombi (ICT), cardiac tumours and valvular vegetations [3]. The prognosis for intracardiac masses is generally guarded, and their appropriate management sometimes requires cardiac surgery, a technique that is still not widely available in Europe. However, diagnosis has been improved by the advent of transthoracic and transoesophageal Doppler echography (TTE), and cardiac Magnetic Resonance Imaging (MRI) [4,5]. The Asian general population prevalence of ICD was 1.5 ‰ in the 2014 study by Yaoet al [2]. We found no previous studies with a more global interest in IBD in Burkina Faso, including all subgroups (intracardiac thrombi, cardiac tumours, valvular vegetations). We therefore decided to look at the epidemiological, clinical, therapeutic and evolutionary aspects of IBD based on cases collected in the cardiology department of the Yalgado Ouedraogo University Hospital (CHU-YO) from 1 January 2011 to 31 March 2013.
PATIENTS AND METHOD
This was a retrospective descriptive study conducted in the cardiology department from 1 January 2011 to 31 March 2013. All patients of both sexes diagnosed and hospitalised with intracardiac masses were included in the study. Each patient included had a minimum follow-up of three months. Patients with ICMs other than tumours, thrombi and valvular vegetations such as pacemaker leads, catheters, anatomical remnants and valvular calcifications were excluded from our study. The variables studied were:
♣ Epidemiological data: sex, age, marital status, occupation, place of residence residence and socio economic level.
♣ Cardiovascular risk factors: age, hypertension, smoking, diabetes, oestroprogestogenic contraception, sedentary lifestyle, obesity, etc.
♣ Clinical data studied: dyspnoea, headaches, precordialgia, palpitations, temperature, heart rate, blood pressure and signs of heart failure and motor deficit.
♣ Therapeutic aspects: nature of treatment: medical (anticoagulant, antiplatelet agent, digitodiuretic, anti-arrhythmic); duration of treatment; whether or not the patient was receiving anticoagulant or antiplatelet agent treatment prior to hospitalisation in the cardiology department.
♣ Evolutionary aspects: length of hospitalisation, follow-up and survival.
Data processing and analysis
The data were processed and analysed using the following software package EPI info version 3.5.1. Qualitative and quantitative variables were assessed in terms of frequency and mean plus or minus standard deviation. Comparison of means and percentages was carried out using Pearson’s Chi2 test with a significance level of p = 0.05.
Ethical aspects considerations included
- Confidentiality of study patient data;
- Explanation of the purpose of the study to patients and their informed consent verbal consent was obtained prior to inclusion.
RESULTS
General characteristics of the population
Among the 1,066 patients admitted during the study period, there were 80 patients with intracardiac masses, representing a hospital frequency of 7.5%. The mean age of the patients was 48.4 ± 17.4 years, with extremes of 17 and 84 years. Half the patients were male, giving a sex ratio of 1
Among the cardiovascular risk factors, diabetes was found in six patients (7.6%), and arterial hypertension in 57 patients (71.3%). A sedentary lifestyle was found in 59 patients (73.8%), and smoking in 19 (23.8%). IBD was discovered during a thromboembolic complication in 18 cases (22.5%), and during a cardiological work-up for heart disease in 62 cases (77.5%). These ICMs were complicated by stroke in 55.6% of cases, pulmonary embolism in 27.8%, syncope in 11.1% and acute ischaemia of the lower limb in 5.6%. The indications for echocardiography were exertional dyspnoea in 77.5% of cases, precordialgia in 45% of cases and palpitations in 7.5% of cases.
Characteristics of intracardiac masses
Among these intracardiac masses (ICMs), intracardiac thrombosis (ICT) was observed in 41 cases, i.e. 50.6% of ICMs and 3.84% of admissions. The other masses were intracardiac tumours and valvular vegetations. Table I
Table 1: Differents types of intracardiac masses
| Type of masse | Effectif (n=81) | Pourcente (%) |
| Thrombosis | 41 | 50,6 |
| Valvular vegetations | 32 | 39.5 |
| Intrcardiac tumor | 8 | 09,9 |
| Total | 81 | 100 |
shows the distribution of the different types of ICM.
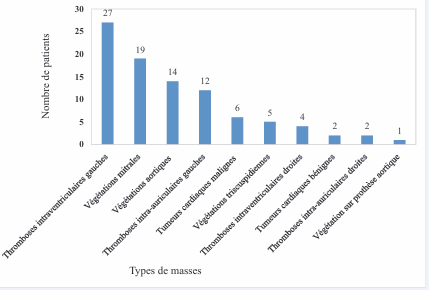
On echocardiography, we found multiple locations of thrombi in the same patient. Four patients had thrombi in two cavities. Six patients had vegetations on different valves. Figure 1
Figure 1:Topographical distribution of different types of mass
shows the topographical distribution of the different types of masses.
Aetiological factors
Heart failure was found in 65 patients (81.3% of cases). The main aetiologies were dilated cardiomyopathy in 23 patients (28.8% of cases), ischaemic heart disease in 8 patients (10%), and peripartum cardiomyopathy (PPMC) in 3 patients (3.8%). Infective endocarditis was found in 29 patients (36.3%), and decompensated rheumatic valve disease in nine patients (11.3%).
Treatment and outcome
Curative treatment of intracardiac masses consisted of anticoagulation in 65% of cases, antibiotics in 58.8% of cases and instrumental treatment in 1.3% of cases. Oral anticoagulation was with antivitamin K. Cardiac surgery was not used as a therapeutic option in our study. The mean length of hospitalisation was 17.4 ± 9.8 days, with extremes of 2 and 61 days, and the mean length of follow up was 12 ± 7.8 months, with extremes of 2 and 26 months. Death occurred early, after 14.3 ± 13.2 days, with extremes of one and 60 days. There was only one case of death during the second month of follow-up in our study. Seven patients died as outpatients (i.e. 8.8% of cases), with a mean time to post-hospital death of 4.6 ± 2.7 months, ranging from 2 to 10 months.
Mortality was therefore very high, with a total of 108 patients dying, including 20 during hospitalisation (25%). The specific mortality rate for intracardiac masses was 18.5%. The causes of these in-hospital deaths were thrombo-embolic complications (30%), uncontrolled heart failure (81.3%), cardiogenic shock (25%) and septic shock (20%).
DISCUSSION
Limitations and constraints of our study
Although this study was prospective, several difficulties were encountered. The monocentric nature of the study, the frequent absence of anatomopathological examination to confirm the nature of the mass, non-compliance with follow-up appointments, and the difficulty of recording deaths occurring at home were the main limitations of the study.
The limited number of studies or scientific works dealing with thrombi, tumours and valve masses at the same time, and looking at epidemiological, clinical, therapeutic and evolutionary aspects, makes it inappropriate to compare some of our results. In fact, most studies of TIMs focus on a specific type of mass, its diagnostic strategies and treatment methods. In our study, we found a prevalence of intracardiac masses of 7.5%, with thrombi representing the most frequent group, in line with the data in the literature [5,6]. During our study, intracardiac tumours accounted for 9.9% of ICMs recorded, i.e. 0.75% of admissions to the cardiology department. Our results are better than those of Damourou et al., in Togo, who reported a rate of 0.2% for cardiac tumours in their ICD series [7]. This difference can be explained by the size of the samples (10 cases versus 80 cases). We observed 32 cases of valvular vegetations, representing 39.5% of ICDs studied and 3% of admissions to the cardiology department during our study period. Elbey et al. in Turkey noted 89% vegetations in their series, but their study only concerned patients followed up for infective endocarditis, which would explain their higher prevalence [8]. In 2010 Ralamboson et al., found a sex ratio of 1.5 in their series of cardiac intracavitary thrombi [9]. Previously described as rare in women, the increase in the prevalence in women could be explained by the increasingly frequent occurrence in women of cardiovascular diseases, particularly those that cause intracardiac thrombi (acute myocardial infarction, dilated cardiomyopathy, valvular diseases). The increased use of contraceptives and the higher prevalence of breast and cervical tumours in women could also explain the sex ratio of 1 in our series.
In our study, MIC was diagnosed in 18 cases (22.5%), when a thromboembolic complication occurred, including stroke in 55.6% of cases, pulmonary embolism in 27.8% of cases, syncope in 11.1% of cases and acute ischaemia of the lower limb in 5.6% of cases. Thomas C et al., noted in their study that 5.2% of strokes occurred during a 31-month follow-up in patients with left intraventricular thrombi [10]. The other study was carried out in a national referral hospital which mainly receives complicated TIC cases transferred from peripheral health facilities. In addition, the low socio-economic level of our populations often makes it difficult to monitor anticoagulant treatment and INR controls. This can lead to treatment breaks or ineffective anticoagulation, which could explain the higher number of strokes.
A left intraventricular location of the thrombus was found in was found in 65.8% of TIC cases. This result is in line with those of Stefano and Davinder, who reported that intraventricular thrombosis in the left cavities was the most frequent and occurred most often in heart disease with LV dilatation and in cases of impaired LV systolic function (dilated cardiomyopathy, acute myocardial infarction) [11,12]. In the literature, left atrial thrombosis is favoured by atrial fibrillation and mitral valve disease [3,13]. They accounted for 29.3% of TIC cases, of which 66.7% of patients had valve disease and 41.7% had atrial fibrillation in our series.
The location of the vegetations was predominantly mitral (23.8% of cases), but also aortic in 17.5% of cases. A predominance of mitral location was reported by Elbey et al., in Turkey (mitral in 43.1% of cases, aortic in 39.1% of cases and tricuspid in 8.9% of cases). This is consistent with the physiological and haemodynamic characteristics of the left ventricle.
Treatment of intracardiac thrombosis in our study was based in the majority of cases on the use of anticoagulants. In the literature, the choice of treatment is sometimes debated, ranging from thrombolysis to thrombectomy. It should be noted that cardiac surgery was not accessible in Burkina at that time. In our study, anticoagulant treatment with low molecular weight heparin (LMWH), was instituted in 100% of patients, 97.6% of whom were followed up with VKA. For some authors, the benefit of thrombectomy is comparable to anticoagulation in the case of TIC [14]. Intracardiac thrombosis accounted for 19.5% of the 18.5% mortality rate for ITC. In-hospital and out-of-hospital mortality in intracardiac tumours was 37.5% and 40% respectively, reflecting their seriousness. Most authors agree that surgical removal remains the only treatment modality for benign cardiac tumours (myxoma and fibroelastoma) [15-17]. However, only symptomatic treatment was used in our patients, which would justify this very high mortality rate.
CONCLUSION
The intracardiac masses visualised on ultrasound in this study were most often thrombi, vegetations or myxomas. The most frequent intracardiac masses were thrombi. Thromboses are serious because of their high mortality rate (in and out of hospital). Their late diagnosis is a potential source of poor prognosis. They therefore require prolonged monitoring in order to preserve the patient’s survival. A prospective study on a larger sample deserves to be carried out in order to collect significant data that could help establish a management protocol adapted to our context.
REFERENCES
1. Perrine Vande Berg, Olivier Marcovitch, Auriane Ceulemans, Marc Alkhori, Ron Cytryn, et al. Incidental cardiac mass ... what should we think?. J Cardiologie.
2. Yao H, N’Guetta R, Ekou A, Anzouan-Kacou JB, Souaga A, Adoh M. Cardiac masses: clinical, epidemiological and evolutionary characteristics of 50 cases. 2014; 4: 273-311.
13. Amad H., Leong-poi H. Les Tumeurs cardiaques primaires. Cardiol Confe Sci. 2006; 6.