Neurogenic Stunned Myocardium - A Case Report
- 1. Division of Adult Cardiology, Sheikh Khalifa Medical City, Abu Dhabhi, United Arab Emirates
- 2. Division of Internal Medicine, Sheikh Khalifa Medical City, Abu Dhabhi, United Arab Emirates
- 3. Division of Pediatric Cardiac Surgery, Sheikh Khalifa Medical City, Abu Dhabhi, United Arab Emirates
Abstract
Neurogenic Stunned Myocardium (NSM) refers to transient cardiac abnormalities, including electrocardiographic changes, that occur following acute neurological events such as stroke or subarachnoid hemorrhage. These presentations can closely mimic acute myocardial infarction, often with normal coronary angiography findings. We report the case of a 51-year-old male who presented with a subarachnoid hemorrhage secondary to methamphetamine intoxication. The patient exhibited ECG changes suggestive of myocardial ischemia, but no evidence of obstructive coronary artery disease was found. His condition deteriorated rapidly. This case highlights the rare and under-recognized phenomenon of NSM, emphasizing the importance of distinguishing it from primary cardiac pathology. In settings where immediate coronary intervention is unavailable or when the diagnosis of myocardial infarction is uncertain, a comprehensive systemic evaluation including detailed history-taking, ECG, toxicology screening, and both coronary and neuroimaging is essential to identify alternative causes and guide appropriate management.
Keywords
• Sub arachnoid hemorrhage; Myocardium, Ischemia; Electrocardiogram; Stroke; Methamphetamine; Toxicity; Troponin.
Citation
Ahmed HA, Elmahi M, Jha NK (2025) Neurogenic Stunned Myocardium - A Case Report. J Cardiol Clin Res. 13(3): 1217.
INTRODUCTION
Neurogenic Stunned Myocardium (NSM) or neurogenic cardiac ECG (electrocardiogram) syndrome, refers to cardiac abnormalities, including ECG changes, that occur following a neurological event like a stroke or subarachnoid hemorrhage. These changes are caused by dysregulation of the autonomic nervous system and excess release of catecholamines, leading to myocardial injuries [1]. We are presenting herewith a 51-year-old male patient who presented with acute stroke (sub arachnoid hemorrhage) as a result of Methamphetamine (meth) intoxication leading to ECG changes without evidence of myocardial ischemia and deteriorated quickly. The case presentation, etiology, pathophysiology and relevant literature is being discussed due to rarity of this condition for educational and learning purposes.
CASE PRESENTATION
A 51-year-old, male patient was brought to the emergency by ambulance after he experienced a collapse while drinking alcohol in a party. History suggested that he was a chronic smoker. Upon arrival, he went to asystole for a brief period and successful cardiopulmonary resuscitation was done by ambulance crew on the spot. He could achieve return of spontaneous circulation (ROSC) after 2-cycles of CPRs (cardiopulmonary resuscitation). Endotracheal intubation, intravenous fluid administration was initiated along with inotropic support. Blood samples were taken for analysis.The initial ECG after ROSC in the emergency department showed ‘ST’elevation in leads I, AVR and AVL with ‘ST ‘depression in anterior and inferior leads (Figure 1). In view of these changes, he was taken directly to cardiac angiography suit and a coronary angiography was done. Surprisingly, the coronary angiogram showed no abnormalities.In the absence of significant coronary artery disease, it was decided to investigate other causes of abnormal ECG. It included sampling for electrolyte, sugar, metabolic, alcohol, infection and toxins including methamphetamine and benzodiazepine in the blood and urine. The patient family confirmed that there was no previous history of any medical illness or medications.After the ROSC, the patient was unconscious with blood pressure of 110 mm Hg. The heart rate was 83 per minute with regular rhythm. He was intubated and on ventilator. Minimal inotropic support was required.
Figure 1: Electrocardiogram on admission showing ST- elevation in the leads I, AVL, AVR and ST- depression in all other leads including anterior leads.
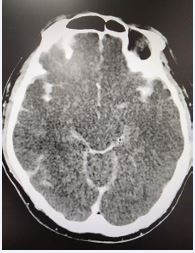
There was no evidence of external injuries. The blood tests showed Troponin T of 314 ng/dl and was significantly elevated. Creatinine, electrolyte, urea, hemoglobin, sugar and blood counts were normal. A toxicology screening was found to be positive for meth (cut-off level 500ng/ml) and benzodiazepine (cut-off level 200ng/ml) in the urine sample. The blood alcohol level was 2.2 mmol/L. The blood culture for bacteria, fugus and various virus panels was negative. The brain CT showed massive supra and infra tentorial subarachnoid hemorrhage (SAH) with extension into the ventricles without dilatation (Figure 2).
Figure 2: Computer Tomogram Head showing grade 4 sub arachnoid hemorrhage in the brain.
There was no evidence of head injury or cerebral ischemic stroke. Intensive care management was continued for his critical condition and despite efforts and supportive measures, he passed away on day 3.
DISCUSSION
Although the ECG is an essential diagnostic test for patients with possible or established myocardial ischemia, it may be normal or associated with non-specific changes in such condition. Surprisingly, sometimes, ECG abnormalities that appear to represent myocardial ischemia or infarction may be related to other etiologies [2]. One such condition is stroke. It is likely mediated by the autonomic nervous system response, particularly secondary to subarachnoid hemorrhage. These changes include QT prolongation, T wave abnormalities, ST segment elevation, and aberrant Q waves An episode of cardiac arrest can further initiates ECG or enzymatic changes [3]. Other ECG changes in stroke may be present in the form of tachy or bradyarrhythmia including various types of heart blocks. Myocardial injury in these cases is most likely the result of a centrally mediated release of catecholamines caused by stroke-related brain injury. This type of cardiac injury is similar to stress cardiomyopathy characterized by transient regional systolic dysfunction of the left ventricle, mimicking myocardial infarction, but in the absence of angiographic evidence of obstructive coronary artery disease or acute plaque rupture [4].Cardiac myofibrillar degeneration has been described in patients who die from acute stroke, and is histologically identical to the cardiac lesions of catecholamine infusion. Myofibrillar degeneration occurs in the vicinity of the cardiac nerves, and not in the macrovascular distribution seen in patients with coronary disease The lesion also differs from the necrosis seen in coronary disease because it is visible within minutes of onset, and the cells die in a hypercontracted state with contraction bands, associated mononuclear infiltration, and early calcification [4].Similarly, an abnormal cardiac troponin level can also be seen in a variety of other diseases including acute stroke. An elevation of troponin and other cardiac enzymes after acute stroke may be related to stroke-induced autonomic dysfunction or other types of nonischemic myocardial injuries (5). Patients with acute ischemic stroke and elevated cardiac troponin have worse functional and mortality-related outcome. While elevated troponin is also frequently observed in patients with intracerebral hemorrhage (ICH), routine invasive coronary angiography should not be performed on these patients [5].Methamphetamine, is a potent and addictive central nervous system stimulant. In clinical practice, it is used to treat attention deficit hyperactivity disorder and obesity. However, it is a controlled medication and known as recreational drug due to the fact that it creates sense of excitement and stimulation and many people get addicted to it. It is also known to cause severe cardiovascular and neurological complications which may have been a significant contributing factor in our patient. The subarachnoid or intracranial hemorrhage may occur due to prolonged use or overdose of meth. The mechanism of hemorrhage is related to hypertensive surge, vasoconstriction, breakdown of blood brain barrier, vasculitis, aneurysm formation and rupture [6]. A synergistic toxicity of alcohol, benzodiazepine and methamphetamine could be lethal. Of the many adverse effects of meth use, hemorrhagic stroke is one of the best described and most devastating entity. A recent review has found that over 80% of case reports and series on meth-related strokes were hemorrhagic. The meth also increases the likelihood of ICH by as much as 2–5 times.The incidence of SAH among meth users is likely less than ICH [6].ossibly, a combination of drug abuse; particularly meth, benzodiazepine and alcohol, resulting in the SAH leading to cardiac dysfunction and arrest, led to a poor prognosis and untimely death of our patient. In this case, administering dual antiplatelet therapy and thrombolytic therapy could have exacerbated bleeding and catastrophic. The learning from our case presentation is that a thorough history, physical examination and evaluation of non- cardiac etiologies are mandatory in cases where coronary angiogram is normal but ECG changes are present in association with myocardial dysfunction.
CONCLUSION
Sub arachnoid hemorrhage can sometimes present with symptoms that mimic acute myocardial infarction, particularly when there are concurrent risk factors like drug use (methamphetamine), or sub arachnoid hemorrhage and both can cause cardiac and neurological manifestations.This presents a diagnostic challenge, as the clinical presentation might resemble a cardiac event, but underlaying cause could be different and uncommon. In a situation where primary coronary intervention is not available or the diagnosis of myocardial infarction is uncertain, it is crucial to perform a thorough systemic examination, including a detailed history, ECG, evaluation of drug toxicity, coronary and neuro imaging to rule out other potential causes of the symptoms.
REFERENCES
- Biso S, Wongrakpanich S, Agrawal A, Yadlapati S, Kishlyansky M, Figueredo V. A Review of Neurogenic Stunned Myocardium. Cardiovasc Psychiatry Neurol. 2017; 2017: 5842182.
- Ceasovschih A, ?orodoc V, Covantsev S, Balta A, Uzokov J, Kaiser SE, et al. Electrocardiogram Features in Non-Cardiac Diseases: From Mechanisms to Practical Aspects. J Multidiscip Healthc. 2024; 17: 1695-1719.
- Lin M, Zhu H. ECG changes and notable markers in ischemic stroke: a systematic review. Heliyon. 2025; 11: e43061
- Chen Z, Venkat P, Seyfried D, Chopp M, Yan T, Chen J. Brain-Heart Interaction: Cardiac Complications After Stroke. Circ Res. 2017; 121: 451-468.
- Fastner C, Lesch H, Kruska M, Haucke ML, Duerschmied D, Platten DM, et al. Cardiac troponin elevation in intracerebral hemorrhage patients may rather reflect acute myocardial damage than acute myocardial infarction. Eur Heart J. 2024; 45: ehae666.3019
- Kafi H, Shannon T, David T, Arielle PD. A review of methamphetamineuse and stroke in the young. Front Neurol. 2024; 15.