Percutaneous Management Post Robotic-Assisted Coronary Artery Bypass Graft Surgery
- 1. Department of Cardiology, King Faisal Specialist Hospital and Research Centre, Saudi Arabia
- 2. Department of Cardiac Surgery, King Faisal Specialist Hospital and Research Centre, Saudi Arabia
Abstract
Robotic-assisted coronary artery bypass graft surgery is an emerging approach since it has been associated with less post-operative complications, and shorter length of stay when compared to conventional surgery. Its utilization is growing up especially in some high-volume centers. Commonly, ischemic coronary artery disease was the main target of this new approach. We present a case of aberrant right coronary artery with a malignant course that was treated using this new approach. The procedure was complicated by acute occlusion of both native coronary artery and graft internal mammary artery. Percutaneous coronary intervention was successfully performed as a bail-out and restored the coronary flow
Keywords
• Aberrant coronary
• Myocardial infarction
• Percutaneous coronary intervention
• Robotic-assisted surgery
• Coronary artery bypass graft
CITATION
Dahdouh Z, Khaliel F. Percutaneous Management Post Robotic-Assisted Coronary Artery Bypass Graft Surgery. J Cardiol Clin Res. 2023; 11(2): 1193.
INTRODUCTION
Anomalous aortic origin of the coronary arteries is a rare condition and generally of incidental finding, however it could potentially carry serious risks. We present a case of aberrant right coronary artery (RCA) that was treated by robotic-assisted coronary artery bypass graft (RA-CABG). The procedure was complicated by arterial graft and native coronary occlusion that was successfully managed by percutaneous intervention.
CASE REPORT
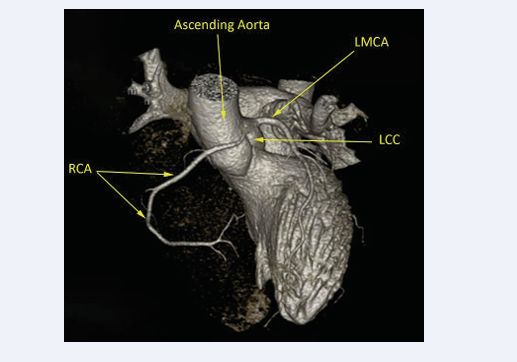
A 38-year-old male, previously healthy with no cardiac risk factors, presented to our institution with typical chest pain on exertion with recurrent episodes of syncope for the last six months. Electrocardiogram (ECG) at rest was normal. Trans-thoracic echocardiography (TTE), was normal. Coronary computed tomography angiography (CTA) showed patent left coronary system with abnormal origin of a dominant RCA arising from the left coronary cusp with an inter-arterial course between the aortic root and the pulmonary trunk (Figure 1).
Figure 1: Coronary computed tomography angiography (CTA) 3D reconstruction showing patent dominant right coronary artery (RCA) with abnormal origin arising from the left coronary cusp and an interarterial course between the aortic root and the pulmonary trunk.
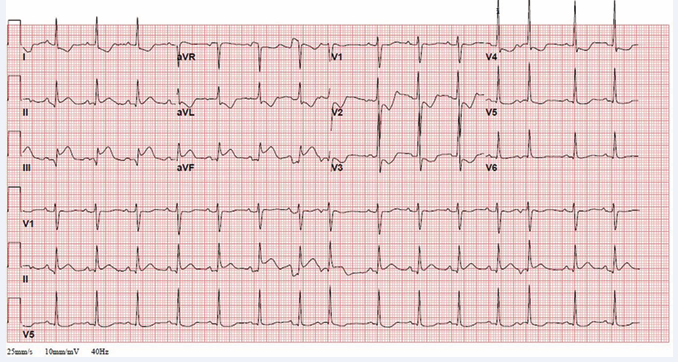
Additionally, the coronary CTA highlighted a sort of “elongation and deformation” at the origin and proximal segment of the RCA. 24-hour Holter monitoring was unremarkable. Stress echocardiography by bicycle was performed and was stopped after 6-minutes due to severe chest pain and dizziness, however with no ECG changes or regional wall motion abnormalities during exercise. Medical therapy based on beta-blockers was initiated; however, symptoms did not improve during follow up. Surgical treatment with unroofing and ostial translocation was offered to the patient as the preferred option. However, the patient totally refused this option since it includes sternotomy. After a multidisciplinary team meeting, it was decided to proceed with RA-CABG surgery using right internal mammary artery (RIMA) to RCA on beating heart off-pump. RIMA was harvested using the da Vinci robot surgical system (Intuitive Surgical, Sunnyvale, CA). RIMA was anastomosed to the mid RCA segment through right mini thoracotomy. ACT was above 300 sec during the procedure, and the anastomotic site was controlled with MediStim ASA Doppler flow meter (Oslo, Norway) showing a good transit-time flow and Pulsatility Index. The patient was transferred to the cardiac surgery intensive care unit in stable condition. Few hours later, ECG showed ST segment elevation in the inferior leads with reciprocal changes in the antero-lateral leads (Figure 2).
Figure 2: Electrocardiogram few hours post robotic-assisted coronary artery bypass graft surgery showing ST segment elevation in the inferior leads with reciprocal changes in the antero-lateral leads.
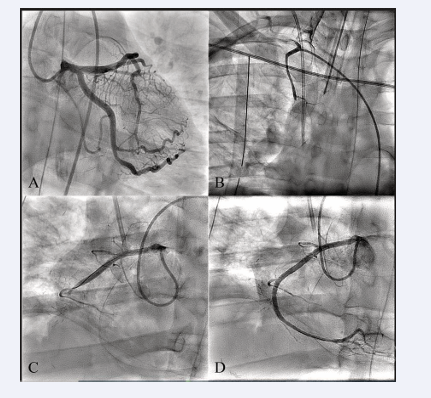
TTE showed akinesia of the basal to mid inferior wall with preserved left ventricular function. Urgent coronary angiogram showed patent left coronary system, total occlusion of the RIMA, and total thrombotic occlusion (TIMI 0 flow) of the mid RCA at the level of the anastomosis with the RIMA (Figure 3, Panel A, B & C; Videos 1 & 2).
Video 1
Video 2
After careful and quick discussion held between the cardiac surgeon and the interventional cardiologist, percutaneous coronary intervention (PCI) was carried on. Stenting to the RCA using two drug eluting stents was successfully performed and TIMI 3 flow was restored (Figure 3, Panel D; Video 3).
Figure 3: Coronary angiogram showing patent left coronary system (Panel A), total occlusion of the RIMA (Panel B; Video 1), and total thrombotic occlusion (TIMI 0 flow) of the mid RCA at the level of the anastomosis with the RIMA (Panel C; Video 2). RCA post stenting with a TIMI 3 flow (Panel D; Video 3).
Video 3
ECG immediately normalized, and TTE showed normal contraction of the inferior wall. The patient was mechanism is the compression of the aberrant RCA caused by pressure and volume expansion of the pulmonary artery against the aorta during exertion leading to myocardial ischemia. Several risk factors for myocardial ischemia were reported in AAORCA, such as high orifice, ostial stenosis, slit-like/fish-mouth-shaped orifice, acute angle take-off, intramural course and its length, inter-arterial path, and hypoplasia of the proximal coronary artery [2].
Correlating the clinical presentation to the AAORCA finding is usually challenging since physiologic investigations to detect myocardial ischemia are generally non-conclusive in such conditions. Fractional flow reserve computed tomography (FFRCT) has been used to identify myocardial ischemia associated with AAORCA [3], however not on a large scale due to its elevated cost and limited availability. Coronary angiogram could detect the abnormal origin of the RCA from the left coronary sinus, however it is of limited diagnostic utility to understand the course of the aberrant RCA as well as its dynamic relation to the adjacent structures [4]. Coronary CTA has emerged as a robust diagnostic tool with three-dimensional view delivering information of the origin, course, and anatomic relationship of the anomalous vessel, allowing differentiation between benign and malignant variants, and subsequently playing a decisive role in the management strategies [5]. AAORCA treatment varies from conservative approach to percutaneous stenting, and surgical intervention depending on the clinical scenario and the center experience in each modality [6,7].
Our patient, who was found to have an AAORCA with an inter-arterial course, poses a real management dilemma since the stress echocardiography was not conclusive and has failed to document any electrical changes or regional wall motion abnormalities. However, our patient presented typical angina and dizziness early during cycling reason for which, along with the recurrent syncope episodes, surgical intervention was decided. Several surgical approaches for AAORCA are possible including “unroofing”, pulmonary artery translocation, reimplantation (ostial translocation), ostioplasty, and bypass grafting [8,9]. The use of saphenous vein grafts is preferred by some surgeons to avoid early occlusion that can occur in arterial grafts that are used to bypass vessels with competitive flow. Other surgeons advocate the use of internal mammary arteries due to their long term patency advantage over vein [10,11]. Ligation of the patent aberrant artery to eliminate competitive flow during the surgery is controversial.
In our case, coronary CTA showed inter-arterial course of the RCA and a sort of “elongation and deformation” at the origin and proximal segment of the RCA as well. This is a common finding among AAORCA taking an inter-arterial course and has been postulated to be the source of ischemia in these patients that can trigger sudden death rather than the external compression caused by the great vessels [2]. Unroofing and ostial translocation was suggested, however, sternotomy or “chest cracking” as described by the patient was completely rejected. Thereafter, RA CABG using RIMA to RCA on beating heart off-pump was offered as an alternative strategy to our young patient with aberrant RCA and, at the same time, it could treat the rheological problem at the proximal RCA by bypassing the “elongation and deformation” at this point. RA-CABG approach has been associated with less post-operative complications, and shorter length of stay when compared to conventional surgery in ischemic coronary artery disease patients [12]. In addition, early clinical and angiographic outcome of RA-CABG was comparable to conventional surgery [13]. Moreover, the decision was supported by the patient preference due to sternotomy and cardiopulmonary bypass avoidance.
Our case was complicated by early graft failure and native RCA occlusion few hours post procedure causing an inferior myocardial infarction. Several mechanisms could be suggested including thrombus formation at the level of the anastomosis causing concomitant total occlusion of the RIMA graft and the native RCA, or direct trauma effect related to the suture going around the anastomosis causing severe narrowing of the native RCA, and subsequently causing competitive flow between the two conduits leading to their mutual occlusion.
In our case, the RCA was ultimately treated with PCI in the mid segment and, unfortunately, the patient still has an anomalous RCA taking a malignant course that remains uncorrected. Since this has not yet been corrected, why did the patient’s symptoms resolve? One hypothesis but difficult to prove could be because the symptoms were attributable to another condition associated to the malignant course such as coronary spasm at the mid RCA that was treated by stenting. Coronary spasm has been reported in aberrant coronary artery [14]. An alternative approach would have been to stent the RCA via the RIMA, though it could be more challenging. If this was performed, the flow to the distal RCA would not depend on the proximal RCA via its inter-arterial course.
In our patient, PCI with stenting post RA-CABG has served as a salvage approach for the suffering myocardium, and possibly as a treatment of an eventual coronary spasm associated to the aberrant RCA with inter-arterial course since the radial force of the stent established a solid conduit to maintain RCA patency at the mid segment.
CONCLUSION
AAORCA accompanied with an inter-arterial course may cause sudden death with exercise. The choice of treatment for this congenital anomaly is controversial. Because of its association with sudden death, most of the literature advocates surgical revascularization. However, surgical revascularization has some drawbacks like early graft failure. Our case illustrates a hyperacute graft failure that can be seen post RA-CABG. In such cases, PCI remains the strategy of choice as a salvage approach for grafts failure. Heart team collaboration between cardiac surgeons and interventional cardiologists is a key factor in such high-risk situations, leading to the optimal decision for the best patient outcome.
REFERENCES
11. Kitamura S, Kawachi K, Nishii T, Taniguchi S, Inoue K, Mizuguchi K, Fukutomi M. Internal thoracic artery grafting for congenital coronary malformations. Ann Thorac Surg 1992; 53: 513-516.