ANCA Positive Glomerulonephritis Due to Levamisole Therapy in Childhood Nephrotic Syndrome: A Case Series
- 1. Teaching Hospital Anuradhapura, Sri Lanka
- 2. Department of Pathology, University of Peradeniya, Sri Lanka
- 3. Teaching Hospital Kurunegala, Sri Lanka
- 4. Department of Paediatrics, University of Peradeniya, Sri Lanka
- #. Equally Contributing Author: Dinesh Rangana, Teaching Hospital Anuradhapura, Sri Lanka
Abstract
Background: Levamisole is a steroid sparing agent used in the treatment of steroid dependent and frequently relapsing nephrotic syndrome. It is used in combination with low dose prednisolone or as monotherapy. Though generally being a safe medication levamisole is known to cause rare systemic side effects like antineutrophil cytoplasmic antibody (ANCA) positive cutaneous vasculitis.
Methods: The clinical, biochemical and histopathological data of 3 cases of levamisole induced ANCA positive glomerulonephritis at our institution were reviewed.
Results: We report 3 patients with nephrotic syndrome treated with levamisole who developed ANCA positive glomerulonephritis. All of them had normal C3 and C4. None had severe forms with associated crescents or global glomerular involvement.
Conclusions: Levamisole induced glomerulonephritis is rare and a high index of clinical suspicion, early evaluation and aggressive management are important in the management of these patients.
Keywords
• Levamisole
• ANCA Positive Glomerulonephritis
• Nephrotic Syndrom
Citation
Rangana D, Wijetunge S, Weerasooriya L, Abeyagunawardena A, Thalgahagoda S (2025) ANCA Positive Glomerulonephritis Due to Levami sole Therapy in Childhood Nephrotic Syndrome: A Case Series. J Clin Nephrol Res 12(1): 1125.
ABBREVIATIONS
ANCA: Anti Neutrophil Cytoplasmic Antibody; Hb: Haemoglobin; ESR: Erythrocyte Sedimentation Rate.
INTRODUCTION
Levamisole, an anti-helminthic agent with immunomodulatory properties, has been used as a steroid sparing agent in patients with steroid dependent and frequently relapsing nephrotic syndrome [1,2]. It is prescribed at a dose of 2–2.5 mg/kg on alternate days for 12–24 months, though more prolonged use may be required [3,4]. It is usually used in combination with prednisolone, though success with monotherapy has also been reported [4]. Levamisole has also been used successfully in the treatment colonic and breast carcinoma as well as rheumatoid arthritis [5-10]. The side effect profile of levamisole includes agranulocytosis, hepatotoxicity, gastrointestinal disturbances and various types of rashes including a vasculitic purpura with a predilection for the ear lobe [1,11-16]. This latter side effect has come into prominence over the last two decades in cocaine abusers due to levamisole being used as a contaminant to enhance its euphoric properties [9, 10]. This cutaneous vasculitic syndrome is characterized by a retiform purpura with bullous formation, cutaneous necrosis, thrombosis of the small vessels and antineutrophil cytoplasmic antibody (ANCA) positivity. There may also be arthropathy and hepatosplenomegaly. End organ involvement in the form of renal and pulmonary involvement, though rare, has also been reported in cocaine abusers with levamisole induced vasculitis [17-21]. We previously reported a possible case of levamisole induced pauci-immune glomerulonephritis with crescents in a patient with nephrotic syndrome who presented with the typical necrotising cutaneous vasculitis with ear lobe involvement [15]. Here we report three further cases of ANCA positive glomerulonephritis due to levamisole therapy in childhood steroid dependent nephrotic syndrome as a case series.
CASE PRESENTATION
Case 01
An eight-year-old girl with steroid dependent, frequently relapsing nephrotic syndrome since the age of five years was commenced on levamisole (2.5 mg/kg on alternate days) as a steroid sparing agent, which was continued for three years. Her last relapse had occurred eleven months prior to presentation and she was on alternate day levamisole monotherapy when she presented with bilateral knee joint arthralgia and a skin rash over the lower limbs for one week duration. Examination revealed pallor and a purpuric rash on both lower limbs. Ear lobe lesions were not detected. There was no clinical evidence of arthritis or oedema detected. Blood pressure was 96/52 mmHg and the rest of the system examination was normal. Her haemoglobin (Hb) level was 9.8 g/dl with blood picture evidence of hypochromic microcytic anaemia. White blood count was 7.49x103/µL, platelets 775x106/µL. Erythrocyte sedimentation rate (ESR) was 98mm in the 1st hour. Serum creatinine remained normal during hospital stay (43 µmol/l). Urinalysis revealed albumin 1+ with moderately field full red cells. Normal complement C3 and C4 levels were noted with negative anti-nuclear antibodies (ANA) and anti-double stranded DNA antibodies (dsDNA). Perinuclear and cytoplasmic anti-neutrophil cytoplasm antibodies (pANCA and cANCA) were positive. Renal histopathology revealed focal segmental necrotizing glomerulonephritis in 3 out of 18 glomeruli present. Crescents were not present. Tubules contained red cell casts and there was patchy tubular interstitial inflammation with interstitial edema. Chronic changes such as glomerulosclerosis, tubular atrophy and interstitial fibrosis were not present. Immunofluorescence was negative for IgG, IgM, IgA and complement C3 (Figure A).
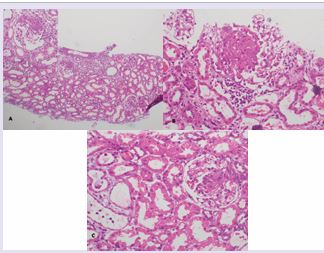
Figure A: Histopathological changes of case 1 to 3 represented by figures A to C (Haematoxylene and eosin stain). A) Low power view (X10) shows a focus of acute tubulo-interstitial inflammation and the inset shows (X40) segmental necrotizing glomerular lesion in
Case 1. B: Histopathological changes of case 1 to 3 represented by figures A to C (Haematoxylene and eosin stain). B) demonstrate (X40) segmental necrotizing glomerular lesions in cases 2 and 3 respectively. Histopathological changes of case 1 to 3 represented by figures A to C (Haematoxylene and eosin stain). A) Low power view (X10) shows a focus of acute tubulo-interstitial inflammation and the inset shows (X40) segmental necrotizing glomerular lesion in Case1. C) demonstrate (X40) segmental necrotizing glomerular lesions in cases 2 and 3 respectively.
Levamisole was omitted on admission. She was treated with immunosuppressive therapy consisting of intravenous methylprednisolone followed by oral prednisolone as well as monthly pulses of intravenous cyclophosphamide as per the unit policy for treatment of acute glomerulonephritis complicated with necrotising lesions. At one-month review urinalysis revealed trace albumin and red cells 20 25/HPF. Urinalysis was completely normal at the second month review.
Case 02
A 13 year old boy with steroid dependent nephrotic syndrome since the age of five years, who was on levamisole for six years, presented with arthralgia for a duration of one month. He was off steroids for six months with levamisole continued as a sole agent at a dose of 2.5 mg/kg on alternate days. Clinical examination revealed pallor without significant rashes or arthropathy. The rest of the system examination was normal. His Hb was 8.9 g/dl with blood picture evidence of hypochromic microcytic anaemia. White cell count was 10.62/µl and platelet count was 361/µl. ESR was 88 mm in the 1st hour. Serum creatinine was 93µmol/l on admission. Urinalysis revealed albumin 2+ with field full red cells. The urine protein: creatinine ratio was 192 mg/ mmol. Normal complement C3 and C4 levels were noted. ANA, pANCA and cANCA were positive. Renal biopsy revealed segmental necrotizing lesions characterized by endocapillary proliferation and karyorrhexis in 5 out of 8 glomeruli examined. Crescents were not present. Low grade acute tubulo interstitial inflammation was also observed involving a few foci; features of chronicity were not present. Immunofluorescence was negative for IgG, IgM, IgA and complement C3 (Figure B). Levamisole was omitted on admission. He also received a regime of intravenous methyl prednisolone and cyclophosphamide followed by oral prednisolone similar to the patient in Case 1. At one month review he was asymptomatic with urinalysis revealing albumin trace and red cells 10-12/HPF and serum creatinine was normal at 43 µmol/l. Urinalysis was completely normal at 2 months follow up.
Case 03
A nine years and six months old boy with steroid dependent nephrotic syndrome since the age of four years and eight months, was on levamisole since the age of 6 years. He was evaluated for pallor while he was on prednisolone 5mg on alternate days and levamisole 2.5 mg/kg on alternate days. Blood investigations revealed Hb 8.3 g/dl with WBC 4.04/µl (N-11%, L-71%) and ESR 60 mm in the 1st hour. One month later he presented with bilateral knee joint and wrist joint pain. Clinical examination revealed pallor and swollen, tender knee joints with normal wrist joints. Obvious rashes were not identified. The rest of the system examination was unremarkable. Investigations during this presentation revealed a Hb of 9.6.g/dl, white cell count of 9.9 /µl, platelet count 436/µl and blood picture revealed hypochromic microcytic anaemia. Serum creatinine was 54µmol/l and ESR was 55mm in the 1st hour. Urine full report revealed a trace of albumin with moderately field full red cells. Complement C3 and C4 levels were normal and ANA was negative. Both pANCA and cANCA were positive. Renal biopsy showed segmental necrotizing lesions in three out of 18 glomeruli, one was globally sclerosed; crescents were not present. Occasional red cell casts were present. Patchy acute tubular-interstitial inflammation of moderate degree was evident. Immunofluorescence revealed IgG+3 mesangial deposits with C3 trace mesangial deposits. IgA and IgM were negative (Figure C). Levamisole was omitted on admission. As in the previous 2 case reports, he was treated with a similar regimen to the first two patients with complete normalisation of ESR and urine within one month.
DISCUSSION
Childhood nephrotic syndrome is the commonest glomerular disease in children which follows a relapsing and remitting course. Levamisole has been used to reduce relapse frequency in patients with frequent relapses and mild steroid dependence. It was initially thought to have a low side effect profile but with numerous cases of cutaneous vasculitis being reported, levamisole fell out of favour in North America and FDA approval was withdrawn. It is still used in some units in the United Kingdom and is widely used in Asia. The exact mechanism by which levamisole produces an ANCA associated vasculitis is not entirely clear. The role of neutrophil extracellular traps (NETS) in the pathogenesis of ANCA associated vasculitis has come to light over the last decade [16]. NETS are thought to extrude both myeloperoxidase (MPO) and serine proteinase 3(PR3), which are usually contained in cytoplasmic granules within neutrophils, to the cellular surface in activated neutrophils. This in turn is thought to lead to ANCA formation. Levamisole is known to promote neutrophil mobility and chemotaxis, enhance dendritic cell maturation and promote T cell proliferation. Through activation of neutrophils, levamisole may thus induce circulating ANCAs by cell surface exposure of MPO and PR3 [16]. Lood et al showed that cocaine alone can induce ANCA formation and the levamisole-cocaine association probably escalates this effect [18]. McGrath et al, in their series of 30 patients with ANCA positive vasculitis due to levamisole contaminated cocaine found arthralgia in 83%, cutaneous manifestations in 61% and ear/nose/throat involvement in 44%. Renal involvement was noted in 8 patients, of which only 2 had severe involvement [17]. Neel et al reviewed 17 patients over a period of eight years with pauci-immune glomerulonephritis due to similar levamisole exposure [19]. Of the three patients described in our series two were on alternate day levamisole monotherapy while one was on alternate day levamisole in combination with a small dose (5mg) of prednisolone on alternate days. Our group previously described a similar case of ANCA associated cutaneous vasculitis and necrotizing glomerulonephritis in a patient who was also on levamisole and a minor dose of prednisolone. It is interesting that all the patients with nephrotic syndrome thus described were either on levamisole monotherapy or coupled with only a minor dose of steroids. This is opposed to the majority of patients on levamisole who are also on significantly high doses of prednisolone. It could be postulated that steroids have a protective effect, preventing the development of ANCAs and thus vasculitis and glomerulonephritis. All three patients in this series and the previously reported case [15], did not have severe forms of necrotizing lesions: none had global glomerular involvement or crescents. All three patients in this series were managed with discontinuation of levamisole and aggressive immunosuppressive therapy as they had evidence of necrotizing glomerulonephritis. All made a complete recovery with normalization of renal function as well as clearing of urinary sediment during follow up. In the series reported by McGrath et al. the two patients with significant renal impairment developed chronic kidney disease, though renal function improved. It would thus seem that early withdrawal of levamisole along with aggressive immunosuppression helps to preserve renal function and avoid chronicity [17]. It would also seem that the dose of levamisole may not have a bearing on the development of necrotising glomerulonephritis. We have shown increased efficacy with the use of daily levamisole, as opposed to alternate day therapy, in the management of nephrotic syndrome [22]. Therefore a significant number of patients with nephrotic syndrome in our unit are on daily levamisole therapy. This complication has, as yet, not been observed in any of these patients. However, as levamisole levels were not monitored, firm conclusions cannot be drawn in this regard. The presence of mesangial IgG and C3 on immunofluorescence in Case 3 is also interesting as ANCA associated vasculitis is usually pauci-immune with minimal immune deposits. However this picture has been noted in previous case series. One of them was an immune complex glomerulonephritis and the other was a membranous nephropathy associated with Levamisole [23,24]. It is possible that all three patients in this series were due to secondary ANCA glomerulonephritis, especially as case 2 and case 3 did not have evidence of cutaneous vasculitis. However, we feel that the association with levamisole is too strong especially as ANCA formation is known to occur with levamisole and necrotising glomerulonephritis has previously been shown to occur with this drug. A high index of clinical suspicion, early evaluation and aggressive management may have contributed to the improved outcome in these patients. Children on long term levamisole are usually monitored only with full blood counts and urinalysis in our unit. In accordance with the findings of this case series, follow up with periodic assessment with ANCA may be beneficial as early detection of these antibodies, may help to prevent the development of this rare but serious complication.
ACKNOWLEDGEMENTS
The parents who consented for the publication of this case series.
REFERENCES
- Levamisole for corticosteroid-dependent nephrotic syndrome in childhood. British Association for Paediatric Nephrology. The Lancet. 1991; 337: 1555-1557.
- Mühlig AK, Lee JY, Kemper MJ, Kronbichler A, Yang JW, Lee JM, et al. Levamisole in children with idiopathic nephrotic syndrome: clinical efficacy and pathophysiological aspects. J Clin Med. 2019; 8: 860.
- Bagga A. Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatrics. 2008; 45.
- Kudagammana ST, Thalgahagoda S, Abeyagunawardena S, Karunadasa UI, Abeyagunawardena AS. Efficacy of Levamisole as a single agent in maintaining remission in steroid dependant nephrotic syndrome. Sri Lanka J Med. 2017; 26: 13-19.
- Mutch RS, Hutson PR. Levamisole in the adjuvant treatment of colon cancer. Clin Pharm. 1991; 10: 95-109.
- Klefström P, Nuortio L. Levamisole in the treatment of advanced breast cancer: A ten-year follow-up of a randomized study. Acta Oncologica. 1991; 30: 347-352.
- Fostiropoulos GA, Zissis NP, Marketos G. Once weekly administration of levamisole in rheumatoid arthritis. Clin and invest med. 1982; 5: 255-258.
- Runge LA, Pinals RS, Tomar RH. Treatment of rheumatoid arthritis with levamisole: long-term results and immune changes. Ann Rheum Dis. 1979; 38: 122-127.
- Walsh NM, Green PJ, Burlingame RW, Pasternak S, Hanly JG. Cocaine- related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol. 2010; 37: 1212-1219.
- Chang A, Osterloh J, Thomas J. Levamisole: a dangerous new cocaine adulterant. Clin Pharmacol Ther. 2010; 88: 408-411.
- Smith JD, BC-ADM CD. Drug-Induced Skin Disorders. US Pharm. 2012; 4: 23.
- Carter MR, Amirhaeri S. p-ANCA-associated vasculitis caused by levamisole-adulterated cocaine: a case report. Case Rep Emerg Med. 2013; 2013: 878903.
- Chung C, Tumeh PC, Birnbaum R, Tan BH, Sharp L, McCoy E, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole- adulterated cocaine. J Am Acad Dermatol. 2011; 65: 722-725.
- Roberts JA, Chévez-Barrios P. Levamisole-induced vasculitis: a characteristic cutaneous vasculitis associated with levamisole- adulterated cocaine. Arch Pathol lab Med. 2015; 139: 1058-1061.
- Thalgahagoda RS, Ranawaka R, Abeyagunawardena S, Karunadasa UI, Abeyagunawardena A. A possible case of levamisole-induced pauci-immune focal necrotising and crescentic glomerulonephritis. Sri Lanka J Child Health. 2019; 48: 84-87.
- Söderberg D, Segelmark M. Neutrophil extracellular traps in ANCA- associated vasculitis. Front Immunol. 2016; 7: 256.
- McGrath MM, Isakova T, Rennke HG, Mottola AM, Laliberte KA, Niles JL. Contaminated cocaine and antineutrophil cytoplasmic antibody- associated disease. Clin J Am Soc Nephrol. 2011; 6: 2799-2805.
- Lood C, Hughes GC. Neutrophil extracellular traps as a potential source of autoantigen in cocaine-associated autoimmunity. Rheumatology. 2017; 56: 638-643.
- Neel A, Agard C, Hamidou M. Vasculitides induced by cocaine and/or levamisole. Joint Bone Spine. 2018; 85: 9-14.
- Karch SB, Busardò FP, Vaiano F, Portelli F, Zaami S, Bertol E. Levamisole adulterated cocaine and pulmonary vasculitis: Presentation of two lethal cases and brief literature review. Forensic Sci Int. 2016; 265: 96-102.
- Quintos A, Vanaik S, Niroula A, Rives-Sanchez M, Sandhu K, SamudralaG. Necrotizing Pneumonia in the Setting of Levamisole Vasculitis. Chest. 2017; 152: A934.
- Abeyagunawardena AS, Karunadasa U, Jayaweera H, Thalgahagoda S, Tennakoon S, Abeyagunawardena S. Efficacy of higher-dose levamisole in maintaining remission in steroid-dependant nephrotic syndrome. Pediatr Nephrol. 2017; 32: 1363-1367.
- Collister D, Sathianathan C, Ryz K, Karpinski M, Bernstein K, Gibson IW. ANCA associated vasculitis secondary to levamisole-adultered cocaine with associated membranous nephropathy: a case series. Am J Nephrol. 2017; 45: 209-216.
- Garg L, Gupta S, Swami A, Zhang P. Levamisole/cocaine induced systemic vasculitis and immune complex glomerulonephritis. Case Reports Nephrol. 2015; 2015: 372413.