Acute Anterior Spinal Artery Syndrome in a Patient with Stented Coarctation of Aorta: A Case Report
- 1. Medical Unit, National Hospitals of Sri Lanka, Sri Lanka
Abstract
Background: Anterior spinal artery thrombosis leading to acute anterior cord syndrome is a rare clinical entity. It can occur in patients who underwent correction of coarctation of aorta even after many years of correction, which is scarcely reported in medical literature.
Case presentation: We present a case of a 39-year-old gentleman, who underwent dilatation and stenting of coarctation of aorta, presenting 14 years after the surgery with anterior spinal cord syndrome, with image proven anterior spinal artery thrombosis.
Conclusion: Our patient’s story illustrates a rare presentation of anterior cord syndrome with anterior spinal artery thrombosis. With the history of repair of aortic coarctation, in situ thrombosis in a residually dilated anterior spinal artery should be considered.
Keywords
• Anterior spinal artery
• Coarctation of aorta
Citation
Perera MNSK, Athukoralage KU (2022) Acute Anterior Spinal Artery Syndrome in a Patient with Stented Coarctation of Aorta: A Case Report. J Neurol Disord Stroke 9(2): 1194.
CASE PRESENTATION
A 39 year-old gentleman presented with acute onset back pain followed by bilateral lower limb weakness and numbness. There was no upper limb weakness or numbness. He was at his usual health on that day prior to the event, when he noted the above symptoms while he was working in the paddy field. Following admission, he developed acute urinary retention. He didn’t have alteration of consciousness, visual symptoms, swallowing difficulty or speech disturbances. There was no history of trauma to back. He didn’t have recent preceding fever, respiratory symptoms, alteration of bowel habits, night sweats or constitutional symptoms. There were no similar paralytic episodes in the past or any thrombotic manifestations. Current presentation was not associated with chest pain, palpitations, dizziness or shortness of breath.
He was a known hypertensive since the age of 24 years, when his evaluation for a secondary cause revealed the presence of coarctation of aorta. After 1 year from detection, in 2006, he underwent dilatation and stent implantation of coarctation at National hospital of Sri Lanka (NHSL). Post-operative period was uncomplicated. He has been on low dose aspirin until 3 months of post-operative period which was later withheld. One year following the surgery, his antihypertensives were also omitted, as he became normotensive. He was followed up thereafter, at local hospital with regular blood pressure monitoring. He was well in his health for last 14 years after surgery until current presentation. The monthly hospital review, few weeks prior to the current admission revealed a blood pressure measurement of 120/80mmHg.
He didn’t have diabetes mellitus, hypercholesterolaemia or other vascular risk factors. He was a non-smoker and his family history was unremarkable for vascular diseases. On admission, his neurological examination revealed a flaccid paraparesis with bilateral lower limb muscle power of 2/5 and 1/5 in right and left sides respectively. Deep tendon reflexes in lower limbs were absent and plantars were equivocal. Light touch and pin prick sensations were impaired with a sensory level at T2 level. Joint position sensation and vibration sensation were intact. Upper limbs were not weak, but upper limb reflexes were brisk. He had bladder and bowel incontinence. Cranial nerve examination was normal.
Patient was not pale and his pulse was of good volume and regular at a rate of 80 per minute. Peripheral pulses were all palpable symmetrically. Blood pressure in both arms were 120/70 mmHg without orthostatic changes. Cardiac auscultation had normal heart sounds without murmurs. Lung fields were clear to auscultation. Abdominal examination was unremarkable.
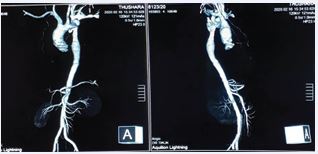
Computer tomography (CT) aortogram didn’t show aortic dissection or aneurysm; and the aortic stent was in normal position with normal blood flow proximal and distal to the stent (Figure 1).
Figure 1 Computed Tomography aortic angiogram.
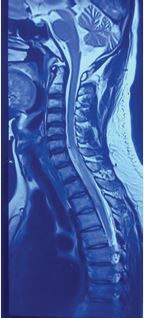
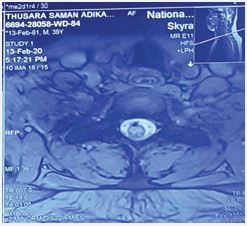
Magnetic resonance imaging (MRI) of whole spine revealed spinal cord ischaemia with anterior spinal artery thrombosis (Figure 2,3).
Figure 2 T2 high signal with cord expansion from lower border of C6 level upto the upper border of T4vertebral body levels. Anterior and central cord was involved with preservation of the posterior part of the spinal cord.
Figure 3 Anterior to the cord thrombosed vessel seen from C7 to T2 level (arrowed).
Coagulopathy screening and autoimmune panel were negative. Electrocardoigram showed sinus rhythm with voltage criteria for left ventricular hypertrophy. Transthoracic and transoesophageal echocardiogram didn’t reveal cardiac sources of thromboembolism. Therefore, anticoagulation was not suggested by the consultant cardiologist. Patient was started on aspirin.
Patient was referred for spinal rehabilitation under the care of specialized rehabilitation team including consultant rheumatologist, physiotherapist and occupational therapist. Muscle strengthening, ambulation, self-intermittent catheterization, and neuropathic pain management were carried out.
Neurological examination after 3 months from the event revealed spastic lower limb weakness with lower limb muscle power of 4/5 bilaterally. Lower limb deep tendon reflexes were brisk and plantars were upgoing. There was no clonus. T2 sensory level persisted. He was able to walk independently. Bladder control was partially achieved and clean self-intermittent catherterization too was continued. Total bowel control was achieved. Repeat MRI of spine showed calcified thrombus in the anterior spinal artery further confirming the primary diagnosis of anterior spinal artery thrombosis.
DISCUSSION
Bold supply to spinal cord is through a single anterior spinal artery and two posterior spinal arteries. All of them are branches of the vertebral artery [1]. Anterior cord syndrome can occur when ischemia occurs to anterior 2/3 of spinal cord. Anterior spinal artery occlusion occurs due to thrombotic or embolic causes. It results in infarction of the corticospinal and spinothalamic tracts leading to initial acute flaccid paralysis, which later progresses to spastic weakness. Pain and temperature sensation loss occurs below the level of the lesion. Tactile sensation, joint position sensation and vibration sensation would be intact because the posterior spinal artery territories are preserved [2].
This young patient presented with acute onset paraplegia, without a history of trauma or symptoms and signs of infection. Full detailed neurological examination of him concluded as anterior cord syndrome. Identification of the site of the lesion as anterior spinal cord syndrome was helpful at this stage to build on the causes for the lesion.
In this patient, MRI imaging concluded evidence of anterior spinal cord ischaemia with anterior spinal artery thrombosis. Negative serology and normal CSF analysis further helped in exclusion of other causes for acute spinal cord syndrome.
Common causes for ischaemia and infarction in anterior spinal artery territory include, atherosclerotic aortic vessel and its branches, mitral valve disease and multiple emboli, surgery for aortic occlusive disease, vasculitis, polycythemia, sickle cell anemia and hypotension due to cardiac arrest, traumatic rupture of aorta or aortic dissection. [1-3]
His past history led us to narrow down the differentials to a pathology related to the underlying coarctation. Coarctation of aorta accounts for 6.8% of all congenital heart diseases [4]. It can be treated successfully with surgical or catheterization techniques such as balloon angioplasty and stenting. When the coarctation is detected in older children or adults, stenting is preferred over surgical correction especially in the presence of arch hypoplasia and tortuous vessels [5].
This patient was diagnosed as having coarctation when he was evaluated for young hypertension. It was corrected by dilatation followed by expandable stent insertion at his age of 26 years. He made a good clinical recovery following the surgery and post-operative 14 years were uncomplicated until the current presentation. Persistent hypertension is a usual finding when correction is done after 20 years of age compared to childhood correction [6]. But this patient showed a good response with normalisation of blood pressure within about 1 year following surgery. He didn’t have any other thrombotic manifestations, neither there were laboratory or serology evidence to suggest acquired or inherited thrombophilia status. His echocardiography didn’t reveal bicuspid aortic valve or any other cardiac sources of thromboembolism.
Following successful surgical repair of coarctation, complications such as re-coarctation, aneurysm formation at the site of repair, aortic rupture, myocardial infarction and subarachnoid hemorrhage are recognised [5,7,8]. Spinal artery ischaemia can occur due to diminished blood flow to spinal cord during surgical repair or at immediate post-operative period [9]. In long standing coarctation of aorta, vasculature can change with sclerosis or dilatation. This can involve the anterior spinal artery and it is thought to be the contributing factor for delayed thrombosis of anterior spinal artery in patients with coarctation, when other causes are excluded [8,9].
This patient was haemodynamically stable with normal cardiovascular examination findings on admission, which was immediately after the onset of symptoms. His CT aortogram excluded dissection, aortic rupture, aneurysm formation or re coarctation. Embolic manifestations were too excluded, so insitu thrombosis due to residual dilatation of the anterior spinal artery was considered as the pathology.
Management of anterior spinal artery thrombosis remains debatable. Studies have shown no proven benefits in usage of corticosteroids or anticoagulation [10]. Secondary prophylaxis using aspirin is of proven benefit, which was initiated in our patient [10]. Rehabilitation is the most crucial management step in these patients, which gives successful outcomes as in our patient. Spinal cord infarction itself being a rare condition [11], we illustrated a young gentleman presenting with anterior spinal artery thrombosis, 14 years following successful aortic coarctation stenting.
His story teaches us on the need of proper neurological assessment of suspected spinal cord lesions with syndromic approach. Even though delayed anterior spinal artery thrombosis is a rare entity in patients who had coarctation of aorta, consideration of the underlying vascular pathology with regard to the clinical presentation, helped us to make the diagnosis. Early imaging with MRI helped to confirm it as well as to rule out other differentials. This patient’s story further emphasizes the benefit of early initiation of rehabilitation which gave a favourable outcome to this patient.
REFERENCES
- Bican O, Minagar A. Pruitt AA. The spinal cord: a review of functional neuroanatomy. Neurol Clini. 2013; 31: 1-18.
- Satran R. Spinal cord infarction. Stroke. 1988; 19: 529-532.
- Foo D, Rossier AB. Anterior spinal artery syndrome and its natural history. Paraplegia. 1983; 21: 1-10
- Swan L, Wilson N, Houston AB, Doig W, Pollock JC, Hillis WS. The long- term management of the patient with an aortic coarctation repair. Eur Heart J. 1998; 19: 382– 386.
- Suradi H, Hijazi ZM. Current management of coarctation of the aorta. Glob Cardiol Sci Pract. 2015: 2015; 44.
- Fawzy ME, Fathala A, Osman A, Badr A, Mostafa MA, Mohomed G, et al. Twenty- two years of follow up results of balloon angioplasty for discrete native coarctation of aorta in adolescents and adults. Am Heart J. 2008; 156: 910-917.
- Campbell M. Natural history of coarctation of the aorta. Br Heart J. 1970; 32: 633-640.
- Jenkins NP, Ward. Coarctation of the aorta: natural history and outcome after surgical treatment. QMJ Int J Med.1999; 92; 365-371
- Servais LJ, Rivelli SK, Dachy BA, Christophe CD, Dan B. Anterior spinal artery syndrome after aortic surgery in a child. Pediat Neurol. 2001; 24: 310-2.
- de Seze J, Stojkovic T, Breteau G, Lucas C, Michon-Pasturel U, Gauvrit JY, et al. Acute myelopathies: Clinical, laboratory and outcome profiles in 79 cases. Brain. 2001; 124: 1509-1521.
- Masson CP, Meder JF, Cordonnier C, Touze E, De La SV, M Giroud, et al. Spinal cord infarction: clinical and magnetic resonance imaging findings and short-term outcome. J Neurol Neurosurg Psychiatry. 2004; 75: 1431-1435.