Effect of Constraint, Induced Movement Therapy and Mirror Therapy for Patients with Subacute Stroke in Bangladesh
- 1. Department of Physical Medicine and Rehabilitation, Kumudini Women’s Medical College, Bangladesh
- 2. Department of Physical Medicine and Rehabilitation, Kurmitola General Hospital, Bangladesh
- 3. Department of Physical Medicine and Rehabilitation, BSMMU, Bangladesh
- 4. Department of Internal Medicine, BSMMU, Bangladesh
Abstract
Subacute stroke is a health, related problem that spans a period from two days to two weeks. This randomized controlled trial investigates the effectiveness of constraint, induced movement therapy (CIMT) and combined mirror therapy for inpatient rehabilitation of patients with subacute stroke admitted to Bangabandhu Sheikh Mujib Medical University (BSMMU). Eighteen patients with subacute stroke were enrolled and randomly divided into three groups: CIMT combined with mirror therapy group, CIMT only group, and control group. Two weeks of CIMT for 6 hours a day with or without mirror therapy for 30 minutes a day were performed under supervision. All groups received conventional occupational therapy for 40 minutes a day for the same period. The CIMT only group and control group also received additional self, exercise to substitute for mirror therapy. We performed the Fugl, Meyer assessment, which was 32.67±21.70 pre,treatment and 37.00±21.06 post,treatment with a p,value of 0.011, MRC muscle grading pre,treatment 3.01±2.78 and 3.21±1.35 post,treatment with a p,value of 0.107, and Modified Barthel Index pre,treatment 29.56±27.43 and 28.33±26.71 post,treatment with a p,value of 0.104. After two weeks of treatment, we had found that CIMT along with mirror therapy, had more impact on subacute stroke patients. More early initiation of rehabilitation program showed better results.
Keywords
• Induced Movement Therapy
• Mirror Therapy
• Subacute stroke
• Rehabilitation
CITATION
Newaz F, Hasan I, Ahmed SM, Imam H (2023) Effect of Constraint, Induced Movement Therapy and Mirror Therapy for Patients with Subacute Stroke in Bangladesh. J Neurol Disord Stroke 10(3): 1207.
INTRODUCTION
Stroke is one of the common and disabling health, care problems worldwide. It is the third most common cause of death in the developed world after cancer and ischaemic heart disease and is the most common cause of severe physical disability [1,2]. Every year, a significant number of stroke survivors are left with residual disabilities, varying from mild to severe form [3]. These disabilities can be reduced by proper rehabilitation [4,5]. Stroke is frequently accompanied by loss of motor function, where more than half of stroke survivors losing functional abilities in their affected upper limb [6-9]. The consequences of upper limb disability in post,stroke adults influence their activities of daily living (ADL) such as feeding, grooming, bathing, dressing, toileting etc [10,11]. After the stroke, when the function of one side is superior to the contralateral limb, a patient may prefer to use the active limb to perform self, care. With time they use their non, involved limb to perform ADL [12,13]. Tarb et al., described this phenomenon as “learned non, use” [14,15]. As upper limbs play a valuable role in performing ADL, retraining motor controls and skills to improve ADL should be an important aim of rehabilitation programs [12]. The upper limb dysfunction due to stroke is usually treated by using various rehabilitation approaches; CIMT is one of these approaches which may minimize the consequences of upper limb dysfunction and enhance stroke patients’ daily functional activities [6,14-16]. CIMT was developed by Dr. Edward Taub, is a therapeutic package based on two principles: (1) restraint of the less,affected limb for prolonged periods to force the use of the more,affected limb and (2) supervised repetitive task practice of upper limb by shaping [17-20]. Types of restraints include a sling or triangular bandage, a splint, a sling combined with a resting hand splint, a half glove, and a mitt [21]. Determination of the type of restraint used for therapy depends on the required level of safety [22]. While restraining the unaffected upper limb 90% of waking hours, training the affected limb six hours a day, for two weeks in a hospital setting [19,23-25]. Shaping is a training method in which a task is gradually made more difficult with respect to a patient’s motor capabilities. It is systematic, specifiable, and quantified. About 120 tasks have been developed by the Constraint, Induced Therapy Research Group. Among these, 10 to 15 tasks are selected primarily for each patient. Each task is usually performed in a set of 10, 30 seconds trials. At the end of each set of 10 trials, the task is changed. A reward should be provided visually and verbally to encourage good performance. Performance regressions are usually ignored. Rest should be given between trials as needed [15]. As a patient is engaged in repetitive exercises with the affected limb, the brain grows new neural pathways referred to as cortical reorganization or neuroplasticity. Thus possible benefits are achieved [21,22,26]. Reliable and valid measurements of motor functions are required to assess physical recovery following stroke. The Fugl, Meyer assessment was developed for these purposes. Fugl, Meyer motor assessment includes items dealing with the shoulder, elbow, forearm, wrist, and hand in the upper extremity [27,30].
MATERIALS AND METHODS
The Physical Medicine and Rehabilitation (PM&R) department of BSMMU was the place of study for this RCT. All the patients attending the PM&R department having the first stroke attack with uncomplicated patients were the sample. Patients who fulfilled the inclusion criteria were the study subjects. We used a specifically developed assessment questionnaire for data collection. Before the intervention, One Internist and two Rehabilitation physicians evaluated the chosen patients by history, physical examination, and relevant investigations. Then subjects were enrolled after providing informed written consent. The sample size was 18. In the combined CIMT, mirror therapy group and CIMT only group, patients wore a specially designed orthosis to suppress the unaffected upper extremity’s motion for a total of two weeks. The patients received intensive training for five days a week except for the weekend, for a total of six hours (2 hours in the therapy room and 4 hours in the inpatient room) a day except for sleeping hours. During the time, an occupational therapist performed the intensive fine motor exercise of the hemiplegic upper extremity. The mirror therapy was performed for 30 minutes a day for five days a week, for two weeks. According to the verbal commands, patients completed the mirror therapy components like flexion and extension of the shoulder, elbow, wrist, finger, and pronation and supination of the forearm. They also performed the objective task training with the unaffected hands. The control group patients executed the self, exercise program and the palliative rehabilitation therapy as routinely recommended for the hospitalized patients. The combined CIMT, mirror therapy group did not receive the palliative rehabilitation therapy, and they performed mirror therapy during the CIMT break period. The patients of the CIMT only group committed CIMT, palliative rehabilitation therapy, and an additional self, exercise program to minimize the difference in the total amount of treatment time between the three groups. Moreover, we also maximized full, time guardians’ participation to improve treatment compliance and lower the drop, out rate. Furthermore, we made it easier to monitor the length of time the patients wear the orthosis by enrolling hospitalized patients for the first two weeks in this study rather than the outpatients.
RESULTS
During the study period, 27 stroke patients according to inclusion and exclusion criteria were selected for CIMT on upper limb. But four subjects did not complete their treatment, and five subjects did not come for a second follow-up for unknown reasons. Finally, 18 (n= 18) patients were evaluated for data presentation and analysis. Data are presented and analyzed according to objectives. The findings are presented through tables, graphs and organized.
The Table 1 shows that the mean age of the patients was 52.77±10.30 years. Among the studied patients regarding the age distribution, most of the patients (66.7%) were found in the 46 60 years age group followed by 16.67% in ≤ 45 years and >60 years of age group. The patient’s lowest and highest age in this study was 30 years and 70 years, respectively.
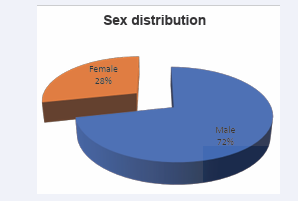
Among the studied patients regarding the sex distribution, most of the patients (72%) were male, and 28% were female. The ratio of male-female was 2.57:1 (Figure 1).
Figure 1: Sex distribution (n= 18):
The Table 2 shows the distribution of occupation among the studied patients, 44.44% were retired, 16.67% housewife, 11.11% service holder, 5.56% were a farmer and businessman and 11.11% were teacher and unemployment each
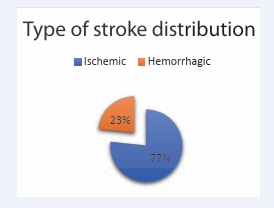
Among the study subjects regarding the type of stroke, most of the patients were found ischemic (77%) and rests (23%) were hemorrhagic (Figure 2).
Figure 2: Distribution of type of stroke (n= 18)
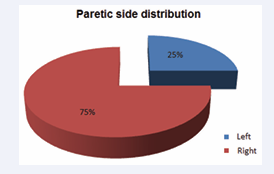
Among the study subjects’ paretic side distribution, most patients’ (75%) paretic sides were right, and (25%) rest of them are left (Figure 3).
Among the studied patients regarding the distribution of comorbidities, only Hypertension (HTN) and only Diabetes mellitus (DM) were found in 50.0% and 16.7% of patients, respectively. Both DM and HTN were found in 22.2% of patients, and no HTN or DM was found in 11.1% of patients (Table 3).
Figure 2: Distribution of paretic side (n= 18)
The mean FIM score at baseline among the studied patients was 106.28±12.61. The lowest and highest FIM score at baseline in this study was 88 and 126 respectively (Table 4).
Table 5 showing evaluation of FM score at different follow up. We found a significant difference between mild and moderate impairment groups at initial assessment, week two, and week four follow-up (P<0.05) regarding FM score. The table also shows an increasing percentage of mild impairment group and a decreasing moderate impairment group at week two and week four follow-up. There was no severe impairment group (Table 6,7).
DISCUSSION
Stroke is third important cause of disability. Impaired muscle strength throw challenge to patient, care, giver and rehabilitation specialists. As described, if hemiplegic patients use the unaffected upper extremity, they would lose the functional independence. In this present study, the mean age of the patients was 52.77±10.30 years. Most of the patients were in the 46,60 years age group (60%), followed by 20% in the 30,45 and 61,70 years of age group. Our investigation found similar mean age in many studies [6,12,31], including studies of Bangladesh [38-40], where most stroke patients were between 51,70 years of age.
Most of the patients in this study were male (72%). The ratio of male, female was 2.57:1. On the other hand, the male, female proportion in the survey of Tariah HA et al. [6], was 4:1, Gharib M et al. [12], was 1.67:1, and Steven L et al. [33], and was 2.86:1. Male predominance in stroke was the findings in various studies in Bangladesh [38,41].
In this study, most of the patients were retired (33.3%) followed by 28.3% housewife, 18.3% service holder, 6.7% were farmer and businessman, and 3.3% were teacher and unemployment each respectively, which coincided with the study of Hossain AM et al., [39].
The patients’ mean duration of onset of stroke was 34.62±48.66 days, and most of the patients were 78.3% in the 1,30 days group. Among the rest, 10.0% were in more than 90 days, 8.3% in 61, 90 days, and 3.3% in the 31,60 days group, respectively. Those reflect stroke patients seek rehabilitation in an early phase and the chronic phase of the stroke.
The highest 77% patient’s type of stroke was Ischemic stroke. Most of the patient’s paretic side was right (75%), which was nearly similar to Tariah HA et al. (70%) [6], Sanford J et al. (60%) [27], and Mohammad QD et al. (72%) studies [38].
Among the patients, most of the comorbidities were HTN 50.0%, followed by DM and HTN 22.2%, unknown 11.1%, and DM 16.7%. Hayee et al. [42], found 52.11%, and Alamgir et al. 43 found 58% Hypertensive. Similar studies in some Asian countries also correlated with the present study [43].
The mean FM baseline score was 45.57±7.56, where the moderate impairment group was 86.7%, and the mild impairment group was 13.3% (p=0.000). After a two, week follow up, the mean FM score was 52.25±6.58; among them, 68.3% were in moderate impairment, and 31.7% were in the mild impairment group (p=0.000). After a four, week follow up, the mean FM score was 54.42±5.66, among them the moderate impairment group 60% and mild impairment group 40% (p=0.000). There was no severe impairment group in this study.
A study done by Tariah HA et al. [6], found the mean FM baseline score was 46.7±12.64, after two months follow up 55.8±6.46 (p=0.061) and four months follow up 54.5±9.53 (p=0.336) respectively. The Fugl, Meyer Upper Extremity Motor Performance Section Test scores showed significant improvements (P=0.004) in a study by Whitall J et al., [10].
At our medical institution, we performed the conventional CIMT concomitantly with the mirror therapy to improve the hand functions by focusing on the fine motor exercise. This was decided concerning of a possibility that we would achieve the fine motor functions to lesser extents, if we only perform CIMT. In the present study, we compared the difference in the improvements between prior to and following the treatment among the three groups. This finding showed that the degree of the improvement in the box and block test and 9, hole Pegboard test, and the indicators for the fine motor functions as well as the grip strength were all significantly higher in the CIMT combined with mirror therapy group compared to the CIMT only group. These results indicate that the mirror therapy combined with the CIMT would be effective in improving the indicators for the fine motor functions in the clinical setting.
In conclusion, after two weeks of treatment, the CIMT combined with or without mirror therapy groups showed more improvement than the control group in most of functional assessments on hemiplegic upper extremity. The CIMT combined with mirror therapy group achieved more significant improvement than the CIMT only group in Fugl Meyer, MRC and grip strength which represent fine motor functions of the upper extremity.
CONCLUSION
It may be suggested that constraint, induced movement therapy (CIMT), along with mirror therapy and conventional therapy, has a beneficial impact on post, stroke hemiparetic upper limb survivors who were eligible for CIMT. However, further larger sample size powered studies are required to see the effect of CIMT on upper limb motor functions in post, stroke rehabilitation.
ETHICAL ISSUE
A well informed, voluntary, signed written consent was taken in Bangla from the study subjects before enrollment after convincing them that privacy, anonymity, and confidentiality of data information identifying any patient would be maintained strictly. Each patient enjoyed every right to participate or refuse or even withdraw from the study at any point in time. The protocol was approved by the Institutional Review Board of Bangabandhu Sheikh Mujib Medical University.
LIMITATION
1) We evaluated the treatment outcomes at baseline and two weeks after the treatment. Therefore, we did not examine whether our methods were also effective in maintaining the functions of the hemiplegic upper extremity over a long, term period.
2) Our results cannot be completely generalized, because we enrolled a small number of patients and the mean age of the three participating groups showed significant difference. As a pilot study, however, our results contain a clinical significance for combining two intensive rehabilitation treatments for the upper extremity, and this approach deserves further large, scale studies.
3) We used the Mini, Mental Status Examination, MAS scale, and manual muscle test to initially screen the patients. Therefore, we did not examine whether the degree of functional recovery is correlated with the cognitive functions, muscle rigidity, muscle strength, and functional status.
4) There were no consistent criteria for the location or size of lesions prior to the current study. It is probable that the treatment outcomes might be subjected to the degree of the functional defects of the upper extremity, due to the arrangement of the cerebral cortex according to the lesions such as the proximal or distal dominance or the potential visuospatial functions affecting the motor functions.
ACKNOWLEDGEMENT
We are grateful to physiotherapist Mr. Abul Kalam Azad for his kind cooperation. We are thankful for financial support from the Ministry of Science and Technology, Government of Bangladesh (Ref. No. 464/2019).
REFERENCES
3. O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Melacini PR et al.Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010; 376: 112–123.
37. https://www.physio-pedia.com/Fugl-Meyer_Assessment_of_Motor_ Recovery_after_Stroke
43. Wasay M, Khatri IA, Kaul S .Stroke in South Asian countries. Nat Rev Neurol. 2014; 10: 135-143.