Failure of Direct Oral Anticoagulant Therapy Detected by Pharmacodynamic Assay: A Case Report Highlighting the Spectrum of DOAC Response
- 1. Neuroradiologische Klinik, Klinikum Stuttgart, Germany
- 2. Perosphere Technologies, Inc., USA
- 3. Neurologische Klinik, Klinikum Stuttgart, Germany
Abstract
In several neurovascular interventions, direct oral anticoagulants (DOACs) are required in addition to antiplatelet therapy. Antiplatelet therapy can be reliably assessed by platelet function tests. However, anticoagulant monitoring is not part of clinical routine, and DOAC efficacy is often assumed. In selected pharmacodynamic assay. clinical situations, it may be essential to measure the anticoagulant effect of DOACs to make more informed treatment decisions. We present two cases involving f low diverter treatment of basilar artery aneurysms, highlighting the clinical importance of detecting poor or absent DOAC response using a point-of-care pharmacodynamic assay.
Keywords
• Pharmacodynamic
• Basilar Artery Aneurysm
• DOAC Measure
• Flow Diverter
• Ischemic Stroke
• Anticoagulation Effect; Clotchek
• Point-Of-Care Testing
• DOAC Poor Responder
• DOAC Failure
Citation
Hajiyev K, Bakhru S, Khanafer A, von Gottberg P, Wolf M, et al. (2025) Failure of Direct Oral Anticoagulant Therapy Detected by Pharmaco dynamic Assay: A Case Report Highlighting the Spectrum of DOAC Response. J Neurol Disord Stroke 12(3): 1242.
INTRODUCTION
Direct oral anticoagulants (DOACs) have revolutionized anticoagulation management by eliminating the need for routine laboratory monitoring and offering predictable pharmacokinetics [1]. Despite their convenience and widespread adoption, emerging clinical data suggest significant variability in patient response [2-4]. This is particularly relevant in high-risk populations, such as those undergoing complex neurovascular procedures, where thromboembolic complications can result in devastating neurological outcomes. A growing body of evidence indicates that a subset of patients-so-called ‘DOAC poor responders’ or ‘non responders’—may exhibit subtherapeutic anticoagulant effects despite standard dosing [5-8]. This variability may be attributable to differences in absorption, renal clearance, drug interactions, or pharmacogenetics [9]. Importantly, current clinical practice often assumes therapeutic anticoagulation based solely on adherence to prescribed dosing regimens. However, therapeutic plasma concentrations may not necessarily correlate with pharmacodynamic effects. This discordance is particularly concerning in acute care settings where precise assessment of anticoagulant effect can significantly influence therapeutic decisions. Perosphere Technologies Inc. has recently developed and launched in the EU the ClotChek™ coagulometer, a point of care (POC) assay that replicates a whole blood clotting time (WBCT). Clot detection methodology employs an infrared spectrophotometer and disposable glass/silicon test cuvettes that measures clotting time in whole blood (14 ul in 3-8 minutes). The coagulometer serves as a global measure of coagulation status and has demonstrated precision and accuracy, especially at the lower thresholds of DOAC concentrations which is key to critical patient care decisions. This assay provides an individual measure of a patient’s anticoagulant effect and can be pivotal in identifying DOAC poor responders in real time.In this report, we present two illustrative cases that underscore the clinical relevance of pharmacodynamic measurement in patients undergoing endovascular treatment of fusiform basilar artery aneurysms.
Patient 1
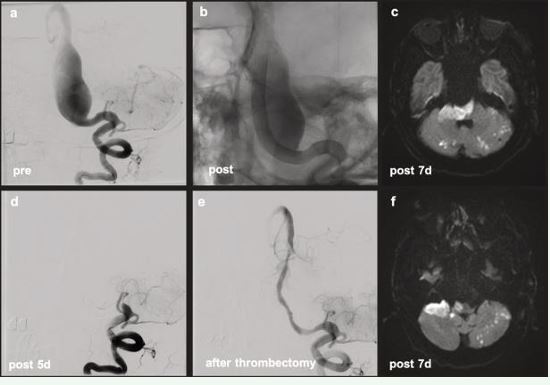
An 81-year-old man referred with a diagnosis of a usiform aneurysm of the basilar artery (BA) had recurrent headaches and visual disturbances. MRI showed a 2.5 cm fusiform aneurysm with significant wall enhancement and brainstem compression. He received loading doses of prasugrel, aspirin, and dabigatran. Platelet function tests measured by Multiplate and VerifyNow assays confirmed adequate inhibition. The patient underwent implantation of five overlapping flow-diverters (FD). Post-operatively, triple antithrombotic therapy was continued. One day post-discharge, the patient developed diplopia and dizziness. MRI revealed new ischemic lesions. Despite continued antiplatelet efficacy, neurological deterioration followed. CT angiography showed FD occlusion. The anticoagulant response to dabigatran was assessed using the ClotChek™ POC device. Clotting Time was 194 seconds, which was below the normal clotting time range (200–290 seconds), thus indicating insufficient dabigatran anticoagulation effect. Emergency thrombectomy restored flow, but ischemic injury progressed. A second thrombectomy was performed, but the patient developed locked-in syndrome and died four days later (Figure 1).
Figure 1 PT 1 Diagnostic: fusiform BA aneurysm (a). Post-treatment without subtraction (b): perfectly adapted FDs from distal left V4 segment to mid BA. Day 5: FD occlusion (d). Successfully recanalized (e). Day 7 MRI: progressive ischemic changes in the brainstem and cerebellum (c, f).
Patient 2
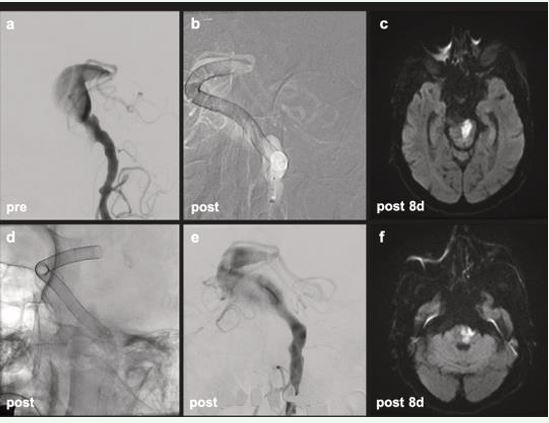
An 88-year-old man with a fusiform BA aneurysm underwent MRI showing a 3.5 cm lesion with mass effect. He received ticagrelor, aspirin, and dabigatran. Antiplatelet measurement confirmed adequate dual platelet receptor inhibition. The patient underwent implantation of ten overlapping FDs. Initially stable, he experienced hypotension post-procedure but recovered without focal deficits. ClotChek™ confirmed that the patient was therapeutically anticoagulated with dabigatran (382s). On postoperative day 5, the patient developed right hemiparesis, dysphagia, and dysarthria. MRI showed pontine ischemia likely due to perforator branch coverage. Dabigatran was discontinued due to nasogastric tube use and replaced with LMWH. Despite progression of local ischemia, no new infarcts were seen and flow diverter was patent. The patient was discharged to rehabilitation (Figure 2).
Figure 2 PT 2 Diagnostic (a): fusiform BA aneurysm. Road map (b), fluoroscopy (d) and post-treatment (e): perfectly adapted FDs from distal left V4 segment to mid BA, telescoping technique, covering entire fusiform segment. MRI after 8 days following treatment demonstrated pontine ischemic infarct (c, f).
DISCUSSION
Non-saccular fusiform basilar artery aneurysms represent a particularly high-risk neurovascular pathology with limited therapeutic options and poor natural history [10,11]. Endovascular reconstruction using overlapping flow diverters (FDs) has emerged as a technically feasible strategy, yet carries substantial procedural risk, including thromboembolic and ischemic complications [12,13]. Antiplatelet and anticoagulant therapy is central to reducing this risk, with recent data supporting triple therapy regimens involving two antiplatelet agents and one DOAC. Despite standardized DOAC dosing, clinical outcomes remain heterogeneous. This variability could reflect a clinically relevant spectrum of anticoagulant response among patients. Real-world evidence shows that approximately 20% of patients treated with DOACs for atrial fibrillation experience breakthrough ischemic strokes, raising concern for suboptimal pharmacodynamic effect [8]. Such patients may not achieve sufficient thrombin or factor Xa inhibition despite appropriate plasma levels. Pharmacodynamic failure may be especially consequential in the neurointerventional setting, where clot formation on stent constructs or within aneurysm sacs can result in brainstem infarction or death. The cases presented here exemplify both ends of the DOAC response spectrum. ClotChek™ testing in Patient 1 demonstrated insufficient dabigatran effect, which likely contributed to the development of catastrophic FD thrombosis. This case highlights the inadequacy of relying solely on standard dosing protocols and the need for real-time, point-of-care coagulation testing. Patient 2, in contrast, exhibited a therapeutic response by ClotChek™ and maintained patency of the stent construct, with ischemia likely attributable to hemodynamic and anatomical factors rather than pharmacologic failure. These findings reinforce the concept that pharmacodynamic variability in DOAC response can have significant clinical consequences. Incorporating bedside coagulation testing into neurointerventional practice could guide therapeutic adjustments and ultimately enhance patient outcomes. Further studies are needed to validate these findings and establish standardized protocols for measuring DOAC effect in high-risk populations.
FUNDING
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
REFERENCES
- Heestermans M, Poenou G, Hamzeh-Cognasse H, Cognasse F, Bertoletti L. Anticoagulants: A Short History, Their Mechanism of Action, Pharmacology, and Indications. Cells. 2022; 11: 3214.
- Mekaj YH, Mekaj AY, Duci SB, Miftari EI. New oral anticoagulants: their advantages and disadvantages compared with vitamin K antagonists in the prevention and treatment of patients with thromboembolic events. Ther Clin Risk Manag. 2015; 11: 967-977.
- Foulon-Pinto G, Lafuente-Lafuente C, Jourdi G, Guen JL, Tall F, Puymirat E, et al. Assessment of DOAC in GEriatrics (Adage Study): Rivaroxaban/Apixaban Concentrations and Thrombin Generation Profiles in NVAF Very Elderly Patients. Thromb Haemost. 2023; 123: 402-414.
- Kim PY, Yeh CH, Dale BJ, Leslie BA, Stafford AR, Fredenburgh JC, et al. Mechanistic Basis for the Differential Effects of Rivaroxaban and Apixaban on Global Tests of Coagulation. TH Open. 2018; 2: e190-e201.
- Seiffge DJ, De Marchis GM, Koga M, Paciaroni M, Wilson D, CappellariM, et al. Ischemic Stroke despite Oral Anticoagulant Therapy in Patients with Atrial Fibrillation. Ann Neurol. 2020; 87: 677-687.
- Meinel TR, Branca M, De Marchis GM, Nedeltchev K, Kahles T, Bonati L, et al. Prior Anticoagulation in Patients with Ischemic Stroke and Atrial Fibrillation. Ann Neurol. 2021; 89: 42-53.
- Ali O, Elnaeem A, Kaur M, Thatikonda N, Aigbogun J, Muktadir AKM. Possible Factor Xa Resistance in a Patient Who Failed Apixaban and Rivaroxaban. Clin Case Rep. 2024; 12: e9623.
- McCabe JJ, Cheung Y, Foley M, Brennan SO, Buckley J, Renom PC, et al. Residual Risk of Recurrent Stroke Despite Anticoagulation in Patients With Atrial Fibrillation: A Systematic Review and Meta-Analysis. JAMA Neurol. 2025; 8: 696-705.
- Thompson LE, Davis BH, Narayan R, Goff B, Brown TM, Limdi NA. Personalizing Direct Oral Anticoagulant Therapy for a Diverse Population: Role of Race, Kidney Function, Drug Interactions, and Pharmacogenetics. Clin Pharmacol Ther. 2023; 113: 585-599.
- Shapiro M, Becske T, Riina HA, Raz E, Zumofen D, Nelson PK. Non- saccular vertebrobasilar aneurysms and dolichoectasia: a systematic literature review. J Neurointerv Surg. 2014; 6: 389-393.
- Rezai Jahromi B, Dashti R, Ota N, Dabbagh Ohadi MA, Srinivasan V, Fiorella D, et al. Natural history of dolichoectatic vertebrobasilar aneurysms: a multinational study. J Neurosurg. 2024; 142: 1376-1386.
- Bhogal P, Pérez MA, Ganslandt O, Bäzner H, Henkes H, Fischer S. Treatment of posterior circulation non-saccular aneurysms with flow diverters: a single-center experience and review of 56 patients. J Neurointerv Surg. 2017; 9: 471-481.
- Kiyofuji S, Graffeo CS, Perry A, Murad MH, Flemming KD, Lanzino G, et al. Meta-analysis of treatment outcomes of posterior circulation non- saccular aneurysms by flow diverters. J Neurointerv Surg. 2018; 10: 493-499.