Motor Learning, a Key Feature of Physiotherapy, an Essential Component in (PNF-Based) Neuro-Rehabilitation after Stroke
- 1. Faculty member at the department for physiotherapy, Saxion university, the Netherlands
Abstract
Introduction: The amount of strokes is gradually increasing in the world, for instance in Europe the predictions are an increase of about 27 percent within the next 5 years. This will also increase the costs for society for therapy and rehabilitation. Hemiplegia is the main result of a stroke, hindering the people with a stroke to execute daily activities in a satisfying way. Guidelines for physiotherapy and rehabilitation point besides general therapy to motor learning as a main component of recommended therapy. The question arises what types of motor learning strategies should be considered. Therefore this informative paper is providing an overview and suggestions for possible clinical use. All based upon relevant literature.
Major findings: Motor learning is a process of acquiring the capacity for skilled action, practice and functional task training needs to be part of the provided interventions. Physiotherapist need to use a clinical reasoning approach in regard of ICF categories, activity limitations and underlying impairments. Secondly, biomechanical components need to be considered. These components are described and translated into physiotherapy and rehabilitation approaches with the use of over ten possible strategies. The various principles and strategies addressing motor learning are summarized and the possible effects on reorganization of the nervous system and alterations in neural drive are indicated. Specifically the motor learning approach within the PNF-concept is signalized. Finally two cases are described to illustrate the application of PNF-based motor learning interventions.
Conclusion: A variety of motor learning principles and strategies are based upon evidence in clinical situations. The evidence is a demonstrating neural drive alternations. A sound clinical reasoning is required for physiotherapists. There are indications for the PNF-concept to be within the guidelines for stroke rehabilitation.
Keywords
- Motor learning; Stroke; Hemiplegia; Clinical reasoning; Neuro-rehabilitation; PNF
Citation
Smedes F (2024) Motor Learning, a Key Feature of Physiotherapy, an Essential Component in (PNF-Based) Neuro-Rehabilitation after Stroke. J Neurol Disord Stroke 11(2): 1221.
INTRODUCTION
A stroke has been described by the World Health Organisation (WHO) as a “clinical syndrome characterized by a rapid development of clinical signs and symptoms of focal (sometimes global) disturbance of cerebral function, lasting more than 24 hours or leading to death” [1]. Each year about 12.2 million people suffer a stroke, with a loss of 143 million years of disability life years and 6.6 million deaths annually [2,3]. The prevalence of stroke was 521.000 cases and an incidence of 40.200 new cases per year in 2021 in the Netherlands [4]. Stroke is the primary cause of disablement in the Netherlands. The number of stroke incidence continues to rise due to the ageing population. It is predicted that the number of stroke patients in Europe will rise by 27% by 2027 [5]. The cost of stroke is estimated to be more than US$891billion globally and is expected to increase [3,6].
The results of a stroke are characterized by a hemiplegic disablement as a one sided paresis in the upper and lower extremity demonstrated by problems with activities of daily life (ADL), such as reaching, grabbing and holding objects as well as with ambulation [7-9]. The current view, expressed in guidelines for physiotherapeutic treatment, summarizing the possible interventions with supporting research and evidence are pointing towards the use of motor learning strategies. For example the Guidelines “Stroke” from the Dutch physiotherapy association (KNGF) and from the British National Institute for Health and Care Excellence (NICE) do so [10,11]. An eclectic approach consisting of several different treatment methods, - concepts and - forms seems to offer the best results [10]. There is no evidence that any specific intervention would be superior over other approaches in the rehabilitation of stroke survivors [10]. Task oriented training is strongly advocated in the current view of “neuro-rehabilitation” [9-12]. It is said that on the basis of brain plasticity, therapy-related gains are achieved [13,14]. It is suggested that the provided intervention has to aim for a “motor learning” effect for the tasks practised during therapy, possibly induced by motor cortex plasticity [14,15].
A relative immobilization, “learned non-use” and “disuse” of the arm and hand, but also for the lower extremity may be a result from paresis and/or hypertonia [9,12,16]. Morphologic changes such as contractures and adhesions in muscle and joint tissue may occur as a result of “disuse” and relative immobilization [16- 19]. To overcome these impairments physiotherapy is addressing on all levels from the International Classification of Functioning (ICF) [20].
For relearning motor skills functional (repetitive) task oriented practice is based upon various techniques. These consist of a number of ideas; 1) repetitive practice may lead to beneficial neuroplastic changes within the brain; 2) repetitive practice has a strengthening effect on muscles; 3) a total task can be broken down into their components for practicing single elements before incorporating them into the total movement or task; 4) varying task complexity and training schedules (distributed practice, contextual interference) stimulates generalization to real life situations and retention of skills; 5) feedback is essential for learning the motor skills [11].
Proprioceptive neuromuscular facilitation (PNF) has been described as a comprehensive rehabilitation concept, promoting motor learning, motor control, strength and mobility within task oriented exercises [21-23]. This rehabilitation concept is defined by using specifically motor control and motor learning principles upon the specific utilisation of principles of facilitation of the proprioceptive systems to achieve a neuromuscular response [21,23,24].
Bringing the essentials of motor learning, the role of the physio/occupational therapist and the use of PNF-based physiotherapy intervention into the context of motor learning within neuro-rehabilitation after stroke is the aim of this informative paper.
In order to substantiate this narrative, a literature search has been executed in April 2024. The databases PubMed, CINAHL, Science Direct and Google Scholar have been used, as was the IPNFA website. The search terms included: Motor Learning, Stroke, Hemiplegia, Proprioceptive Neuromuscular Facilitation, PNF, exercise methods, exercise concepts, treatment methods, treatment concepts and rehabilitation approaches. Search terms were used isolated and combined. Literature was screened in order to secure supporting sources for this illuminating narrative. Secondly, the results have been discussed with fellow physiotherapy teaching staff from Saxion University of Applied Science, department of physiotherapy (although not opting for co-authoring) for eligibility.
Papers were included after screening the title and the abstract upon the following criteria: a) motor learning was a part of the publication. b) Techniques for motor learning were a part of the publication. c) motor learning techniques were a part of the treatments for a specific indication or patient population. d) Facilitation to improve motor learning effects was a part of the publication. This resulted in 21 sources supporting the presented view.
MAJOR FINDINGS
Motor Learning
Motor learning has been defined as a relatively permanent change in behavior resulting from practice [25,26]. To achieve a motor learning effect, the patient needs to go through a set of processes associated with practice leading to a (relative) permanent change in the capacity for skilled actions [26,27]. Learning is a process of acquiring the capacity for skilled action, it results from practice and cannot be observed directly but must be inferred from behavior (performance in time). Therefore it is only clearly apparent when the trained activity or skill is retained over time [25-28]. Basically the objective is to acquire motor control over the action and skill. Motor learning is concerned with the acquisition of novel action or movement, but when applied to patients, motor learning is the re-acquisition of previously learned actions in the presence of altered morphology which may be a sensory, motor or cognitive impairment [23].
Motor learning; considerations for physiotherapists
When we define that a patient is learning, one may ask who is teaching and what should be taught? In physical therapy and rehabilitation the “PT” is the Physiotherapist or Physical Therapist, or should we say he/she is the “Private Teacher” for the patient or client. Edwards et al., stated: “learning of movement and its therapeutic application with patients through teaching is arguably the most central role of physiotherapists” [29]. Every patient needs to gain control over his or her movements and activities within the context of the disorder or disease suffered. In musculoskeletal and orthopedic context, consider for example learning to walk and climbing stairs after a total hip replacement or lifting objects after a shoulder surgery. In neurological conditions reaching, walking and climbing stairs also need to be learned again. Prognosis in these various examples may be more or less favorable, depending on the type of disorder or disease.
Considering more detailed the issues on ICF level for a patient, we need to analyze the task at hand and the required control over the various components to execute the task [23]. A lasting response of the neuromuscular mechanism is considered to be a motor learning effect [25-27], which is the key component of the (PNF) philosophy for neuro-rehabilitation [21-23]. To perform a task one needs to make a movement to come into the desired position. To make a movement or to be able to maintain a position, one needs muscle contractions, these contractions and movements in the required or desired position are the minimal requirements for the task at hand. The PT needs to teach the movement, the required type of contractions and the task or skill itself to the patient [23]. Hence, the patient needs to acquire control over external forces and resistances such as gravity and friction. Gravity acting on our own body and body parts and on the objects we handle. When people handle materials and move themselves within a mechanical environment, friction occurs [23]. Patients after stroke often develop a compensation strategy [30]. Therefore, learning to control these external forces with as less as possible compensation is arguably the main objective in neuro-rehabilitation, as in the re-acquisition of previously learned actions in the presence of altered morphology, be it sensory, motor or cognitive impairments [26,27,30].
Analyzing a reaching activity for a coffee cup in an overhead kitchen cupboard, a concentric contraction is needed to reach up and when lowering the arm the same agonists need to work eccentrically because of the weight of the arm and the lifted item [31]. When analyzing a reaching and pulling activity, like in reaching for a rope to pull for toilet flush, the agonists need a concentric contraction to lift the arm towards the rope and then when pulling the rope starts, the antagonists need a concentric contraction to pull against the weight and the friction of the system [31]. Therefore, we can conclude the stroke patient needs variation in coordination for similar but still different tasks. Secondly, neuromuscular control of reaching requires the synchronization of muscle activation at all the moving joints as well as all the muscles involved in postural stabilization [32]. In the described tasks of reaching, the wrist extension needs to be synchronized with gleno-humeral flexion, abduction and external rotation, while at the same time the scapula requires an elevation with lateral upward rotation and slight protraction. The elbow extension is relying on eccentric biceps activation because of gravity acting on the forearm and hand [Figure 1].
Figure 1: Synchronization of the muscle chain in reaching. [Muscles synchronizing in reaching against gravity. 1= wrist extensors and radial deviators; 2= biceps; 3= deltoid; 4= external rotators of glenohumeral joint; 5a= upper trapezius; 5b = lower trapezius (in between the middle trapezius); 6= serratus anterior; Fg= Force from gravity. Black dot in scapula= pivot point for lateral upwards rotation.]
For the two mentioned activities (cupboard and toilet flushing) there is clearly a different inter- and intramuscular coordination required, although it is a similar movement and a slightly different task, but a totally different skill. This can be addressed with specific motor learning techniques and strategies.
Motor Learning strategies
Several strategies [Table 1] to increase the motor learning effects have been described and studied [27,28,33].
Table 1: motor learning principles and strategies in short described
|
Trial and error |
Learning by doing and learning from your own mistakes. |
|
Self controlled practice and guided practice |
Trial and error learning from feeling (the guided) movement and use of the perceived and received feedback. |
|
Observational practice |
First see, than imitate either a novice (see mistakes to be avoided) or an expert. |
|
Massed and distributed practice |
massed practice is longer sessions of the same while distributed practice is more often but shorter. |
|
Variability of practice |
Practicing the same task with different settings and small differences. |
|
Contextual interference |
Mixing various multiple tasks during a practice session (non repetitive). |
|
Focus of attention |
Internal focus on body and (bio)mechanics) versus external focus on the result of activity or task. |
|
Implicit and explicit learning |
Implicit is automatic learning connected to the result (external focus), explicit connected to details that need improvement (internal focus). |
|
Feedback |
Inherent feedback is movement produced and perceived with all senses, intrinsic(e.g. extero- and proprioceptive) and extrinsic (e.g. sounds/auditive, vison, smell). Augmented feedback is artificial, informative and delayed information and cues for corrections and is often verbalized. |
|
Shaping |
Gradually making the task more difficult and towards more real life reality |
|
Forced use |
Where the use of the affected side is demanded and enforced, often by constraining the un-affected side. |
|
Movement imagery |
Mental practice or rehearsal of an activity in the absence of motor execution. |
All publications agree that a functional task context is essential, to ensure task specific training and learning. Observational practice is often in life the first strategy, we people and patients observe others and try to imitate [33]. This can be applied in functional task training, also as repetitive task training. The risk is that only that specific task will be learned and retained. Bernstein (1967) already pointed out learning needs repetition, but without repeating [34]. This means that the same task should be practiced often, but without exact imitation, hence repetition and variability both are necessary [27,28]. Distributed practice and massed practice refer to the time used in the sessions for a task, distributed is more often but shorter while massed means longer sessions of the same [25,35]. Contextual interference refers to mixing multiple task while practicing (non-repetitive) this leads to inferior practice performance but superior retention as compared to practicing a single task repetitive [36]. Focus of attention can be internal, having the focus on the mechanics from the body to perform the task, while external focus of attention has the focus on the result from the task [27,28,33]. This is close to explicit learning versus implicit learning. When the focus of attention is on the result, implicitly, one needs to make more or less correct movements, but when the focus is just on a body part, the result will be less of importance and more incorrect [25,33,35]. A learning curve requires feedback, this can be inherent feedback and augmented feedback. Inherent means “movement produced feedback” while augmented is artificial, delayed, informative, correcting cues (basically that what the PT is providing during a session) [30,36]. Based upon the received feedback the patient will develop knowledge of result (successful or not) or knowledge of performance (how the task or skill was executed) [27,30,33]. Shaping is a strategy where step by step the task difficulty is increasing to achieve the same skill until a real life situation is learned [36,37]. In hemiplegic patient the use of the affected side can be “forced upon” the client, for example by constraining the unaffected side as in constrained induced movement therapy (CIMT) [7,9,12]. But when considering tasks such as closing a zipper or opening a bottle, bilateral hand function is required [23]. Hence, constraining has also its limitations. Guiding and stimulating the affected limb can also be a type of “forced use” during physiotherapy intervention [38]. Finally a patient can practice mentally as in motor imagery, defined as the mental rehearsal of a movement in the absence of motor execution [39] [Table 1].
Clinical implications and incorporated into PNF based neuro-rehabilitation
Voss et al. [24] ,defined PNF as “methods of promoting or hastening the response of the neuromuscular mechanism through stimulation of the proprioceptors”. A conscious and deliberate use of motor learning principles can be the start for clinical decision making, once objectives for the treatment have been defined.
For the use of the PNF-concept there is support from several studies [22,23]. Three-dimensional patterns of movement as defined in the PNF-concept [21,22,24], enhance the initiation of voluntary movements and result in a shorter reaction time for the muscle to be activated and a more efficient movement of the joints compared to neutral positions [40]. According to Moreira et al., a greater cortical activity, measured by the absolute power levels in the beta band in the parietal cortex can be generated wit the use of PNF-pattern movements and this is essential for the integration of motor information [41]. Secondly, an electrophysiological increase of alpha absolute power in the dorsolateral prefrontal cortex and superior parietal cortex results from PNF-pattern movements [42]. Although these cortical effects are of interest for motor learning objectives, motor learning effects are depending on real life tasks in real life environment [15]. Therefore, coping with learned non-use, tightness and weakness, neuro-rehabilitation after stroke needs to address these issues while optimizing neural reorganization in a functional recovery setting. That means achieving motor learning effects depends on providing meaningful task training in a challenging and engaging environment [13,43,44]. Functional task oriented environment situations have been integrated in modern PNF [21,23]. The patient is guided to shift the focus of attention from internal (body oriented) to an external focus (effect oriented) when (PNF) muscle pattern activation is offered in a task oriented way. When an increase of strength, motor control and skill is occurring, the learner’s focus of attention can shift more and more to an external focus [28,33].
CLINICAL ILLUSTRATIONS
- Smedes and da Silva (2019) illustrated in a case study the specified use of PNF muscle activation pattern for arm and hand function problems in tasks where dexterity is of importance [38]. The described patient suffered from a stroke and has an hemiplegic condition. The original intervention offered was CIMT based forced use therapy, but the patient was unhappy with this approach since he felt bilateral handicapped. Thereupon, a PNF based strategy was designed to enforce the use of the affected side, and was successfully applied [38]. Reaching activities for coffee and thee pots and cups has been trained with the specific use of PNF muscle activation pattern of Flexion/Abduction/external rotation with elbow extension [21,23,38]. The specific technique needed to address the earlier described biomechanic demand on the agonistic muscles. Hence, the technique “combination of Isotonics”, which is defined as combining concentric, static and eccentric contractions in the agonistic muscles, has been applied [21,23]. To address more specific first the scapula positioning and later the wrist, hand and fingers, facilitation needed to emphasis this aspect during the practical training, based upon the PNF principle “Timing for Emphasis” [21,23,24].
Figure 2: Synchronization of the muscle chain in reaching. a: Timing for emphasis for scapula lateral upward rotation in reaching. b: Timing for emphasis in finger positioning.
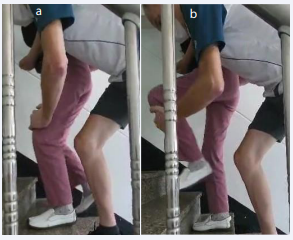
[Figure 2a and b] Also the use of a razor has been trained, requiring alternating lifting against gravity and pulling over the friction from skin and beard. The technique “dynamic reversals” (see case 2) addressed the specific coordination of the involved muscles. - A young man of 28 suffered from an hemiplegic condition on the left side since two years. His difficulty was climbing stairs with alternating steps. To be able to do so, one needs concentric contractions directly after each other from the agonists. To swing the leg up on the next tread, concentric contraction in hip and knee flexors and ankle dorsi flexion is required. To bring the total body weight up on that tread a concentric hip and knee extension together with plantar flexion of the ankle is needed. This alternating and directly activation of agonists and antagonists is mimicked in the PNF technique “dynamic reversals” [21,23,24]. “Forcing the use” of this specific coordination from the involved agonistic and antagonistic muscles can be enhanced by stimulating the correct sensations from propriocepsis (inherent feedback emphasized with augmented feedback). The PNF- concept describes approximation in a closed chain and tactile guidance in the open chain as principles for facilitation of the proprioceptors while learning the specific task at hand [21,23,24] [Figure 3].
Figure 3: Sstair climbing. a: Approximation in closed chain. b: Tactile guidance in open chain.
CONCLUSION
In conclusion one can state that a variety of motor learning principles and strategies have shown to be based upon evidence in clinical situations, and that the evidence is also demonstrating neural drive alternations. Secondly, a sound clinical reasoning integrating activity limitations, underlying impairments (ICF) and biomechanics for task oriented exercises seems to be the basic requirements for physiotherapists. Finally, in neuro- rehabilitation there seems to be indications that the PNF-concept enhances patients abilities from facilitation to participation, and is within the guidelines for stroke rehabilitation.
CONFLICT OF INTEREST
The author is involved in post graduate education (courses) for physiotherapists as a representative of the International PNF Association (IPNFA).
REFERENCES
- World Health Organization. Cerebrovascular Disorders: a clinical and research classification. 1978.
- The rising global burden of stroke.EClinicalMedicine. 2023; 59: 102028.
- Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022; 17: 18-29.
- RIVM. Stroke publications and care. RIVM National Review on stroke. 2022.
- Wafa HA, Wolfe CDA, Emmett E, Roth GA, Johnson CO, Wang Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke. 2020; 51: 2418-2427.
- Owolabi MO, Thrift AG, Mahal A, Ishida M, Martins S, Johnson WD, et al. Primary stroke prevention worldwide: translating evidence into action. Lancet Public Health. 2022; 7: e74-e85.
- Lee van der JH, Wagenaar RC, Lankhorst GJ, Vogelaar TW, Devillé WL, Bouter LM. Forced use of the upper extremity in chronic stroke patients: results from a single-blind randomized clinical trial. Stroke. 1999; 30: 2369-2375.
- Kwakkel G, Meskers CGM, van Wegen EE, Lankhorst GJ, Geurts ACH, van Kuijk AA, et al. Impact of early applied upper limb stimulation: The EXPLICIT-stroke programme design. BMC Neurol. 2008; 8: 49.
- Kwakkel G, Winters C, van Wegen EEH, Nijland RHM, van Kuijk AAA, Visser-Meily A, et al. Effects of Unilateral Upper Limb Training in Two Distinct Prognostic Groups Early after Stroke: The EXPLICIT-Stroke Randomized Clinical Trial. Neurorehabil Neural Repair. 2016; 30: 804-816.
- Royal Dutch Physiotherapy Association. KNGF Guideline. Stroke. 2014.
- Stroke rehabilitation in adults. Nice Guideline. 2023.
- Wolf SL, Winstein CJ, Miller JP,Taub E, Uswatte G, Morris D, et al. Effect of Constraint-Induced Movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA. 2006; 296: 2095-2104.
- Liepert J, Bauder H, Miltner WHR, Taub, Wolfgang HR, Weiller C. Treatment-Induced Cortical Reorganization After Stroke in Humans. Stroke. 2000; 31: 1210-1216.
- Hodics T, Cohen LG, Cramer SC. Functional Imaging of Intervention effects in Stroke Motor Rehabilitation. Arch Phys Med Rehabil. 2006; 87: s36-42.
- Carr JH, Rb Shepheard RB. The Changing Face of Neurological Rehabilitation. Rev Bras Fisioter. 2006; 10: 147-156.
- Gracies JM. Pathophysiology of spastic paresis. I: Paresis and soft tissue changes. Muscle Nerve. 2005; 31: 535-551.
- Pandyan AD, Cameron M, Powell J, Stott DJ, Granat MH. Contractures in the post-stroke wrist: a pilot study of its time course of development and its association with upper limb recovery. Clin Rehabil. 2003; 17: 88-95.
- Lieber RL, Steinman S, Barash IA, Chambers H. Structural and functional changes in spastic skeletal muscle. Muscle Nerve. 2004; 29: 615-627.
- Malhotra S, Pandyan AD, Rosewilliam S, Roffe C, Hermens H. Spasticity and contractures at the wrist after stroke: time course of development and their association with functional recovery of the upper limb. Clin Rehabil. 2011; 25: 184-191.
- World Health Organization. How to use the ICF-A practical manual for using the International Classification of Functioning, Disability and Health.2013.
- Beckers D, Buck M. PNF in practice. 5th ed. Berlin: Springer. 2021.
- Smedes F, Heidmann M, Schäfer C, Fischer N, St?pie? A. The proprioceptive neuromuscular facilitation-concept; the state of the evidence, a narrative review. Physical Therapy Reviews. 2016; 21: 1–15.
- Smedes F. The Essential Elements of the PNF-concept, an Educational Narrative. J Phys Med Rehabil. 2022; 4: 37-48.
- Voss DE, Jonta MK, Meyers BJ. Proprioceptive neuromuscular facilitation – patterns and techniques. 3rd ed. New York (NY): Harper & Row publishers; 1985.
- Schmidt RA, Lee TD. Motor Control and Learning: A Behavioral Emphasis. 5th ed. 2011.
- Shumway-Cook A, Woollacott MH. Motor Control Translating research into clinical practice. 5th ed. Philadelphia (PA): Wolters Kluwer; 2017.
- Kleynen M, Beurskens A, Olijve H, Kamphuis J, Braun S. Application of motor learning in neurorehabilitation: a framework for health-care professionals. Physiother Theory Pract. 2020; 36: 1-20.
- Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychon Bull Rev. 2016; 23: 1382-1414.
- Edwards I, Jones M, Hillier S. The interpretation of experience and its relationship to body movement: a clinical reasoning perspective. Man Ther. 2006; 11: 2-10.
- Fujii S, Lulic T, Chen JL. More feedback is better than less: Learning a novel upper limb joint coordination pattern with augmented auditory feedback. Frontiers in Neuroscience. 2016; 10: 251.
- Knudson D. Fundamentals of Biomechanics. 2nd ed. Springer Science. New York. 2007.
- McCrea PH, Eng JJ, Hodgson AJ. Biomechanics of reaching: Clinical implications for individuals with acquired brain injury. Disabil Rehabil. 2002; 24: 534-541.
- Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med educ. 2010; 44: 75-84.
- Bernstein N. The Co-ordination and Regulation of Movements. 1967.
- Maier M, Ballester BR, Verschure PFMJ. Principles of Neurorehabilitation After Stroke Based on Motor Learning and Brain Plasticity Mechanisms. Front Syst Neurosci. 2019; 13: 74.
- Lin CH (Janice), Yang HC, Knowlton BJ, Wu AD, Iacoboni M, Ye YL, et al. Contextual interference enhances motor learning through increased resting brain connectivity during memory consolidation. Neuroimage. 2018; 181: 1-15.
- Abdullahi A. Effects of Number of Repetitions and Number of Hours of Shaping Practice during Constraint-Induced Movement Therapy: A Randomized Controlled Trial. Neurol Res Int. 2018; 2018: 5496408.
- Smedes F, Giacometti da Silva L. Motor learning with the PNF-concept, an alternative to constrained induced movement therapy in a patient after a stroke; a case report. J Bodyw Mov Ther. 2019; 23: 622-627.
- Kraeutner SN, Cui AX, Boyd LA, Boe SG. Modality of practice modulates resting state connectivity during motor learning. Neurosci Lett. 2022; 11: 781.
- Shimura K, Kasai T. Effects of proprioceptive neuromuscular facilitation on the initiation of voluntary movement and motor evoked potentials in upper limb muscles. Hum Mov Sci. 2002; 21: 101-113.
- Moreira R, Lial L, Teles Monteiro MG, Aragão A, Santos David L, Coertjens M, et al. Diagonal movement of the upper limb produces greater adaptive plasticity than sagittal plane flexion in the shoulder. Neurosci Lett. 2017; 643: 8-15.
- Lial L, Moreira R, Correia L, Andrade A, Pereira CA, Lira R, et al. Proprioceptive neuromuscular facilitation increases alpha absolute power in the dorsolateral prefrontal cortex and superior parietal cortex. Somatosens Mot Res. 2017; 34: 204-212.
- Brach JS, VanSwearingen JM, Gil A, Nadkarni NK, Kriska A, Cham R, et al. Program to improve mobility in aging (PRIMA) study: Methods and rationale of a task-oriented motor learning exercise program. Contemp Clin Trials. 2020; 89: 105912.
- Rozevink SG, Hijmans JM, Horstink KA, van der Sluis CK. Effectiveness of task-specific training using assistive devices and task-specific usual care on upper limb performance after stroke: a systematic review and meta-analysis. Disabil Rehabil Assist Technol. 2023; 18: 1245-1258.
![Synchronization of the muscle chain in reaching. [Muscles synchronizing in reaching against gravity. 1= wrist extensors and radial deviators; 2= biceps; 3= deltoid; 4= external rotators of glenohumeral joint; 5a= upper trapezius; 5b = lower trapezius (in between the middle trapezius); 6= serratus anterior; Fg= Force from gravity. Black dot in scapula= pivot point for lateral upwards rotation.]](https://www.jscimedcentral.com/public/assets/images/uploads/image-1724837131-1.PNG)