Perimesencephalic Hemorrhage: Conventional Angiogram or Not
- 1. Department of Neurosciences and Comprehensive Stroke Center, Corewell Health West, USA
- 2. College of Human Medicine, Michigan State University, USA
Abstract
Parimesencephalic hemorrhage is a rare type of non-aneurysmal subarachnoid hemorrhage (SAH). It is characterized by bleeding around the midbrain region of the brainstem, but often confound with SAH and intraparenchymal hemorrhage (IPH). Unlike other types of SAH, parimesencephalic hemorrhage has a more favorable prognosis. It remains unclear if conventional angiogram is surely necessary in patients with suspected parimesencephalic hemorrhage. We presented an unusual case of a 45-year-old man with initial presentation of severe headache, who received conventional angiogram that unfortunately resulted in multifocal embolic ischemic infarcts. Another 48-year-old woman was admitted to hospital with similar presentation, a diagnosis of parimesencephalic hemorrhage was given based on computed tomography (CT) angiogram (CTA), who made a fully recovery. Our real-world practice experience demonstrated that conventional angiography is not necessary in patients with suspected parimesencephalic hemorrhage to avoid potential periprocedural embolic events.
Keywords
- Parimesencephalic hemorrhage
- Computed tomography angiogram
- Conventional angiogram
CITATION
Javaid B, Ahrar A, Min J (2024) Perimesencephalic Hemorrhage: Conventional Angiogram or Not. J Neurol Disord Stroke 11(3): 1225
INTRODUCTION
Parimesencephalic hemorrhage is a distinctive nonaneurysmal cerebral hemorrhage, representing hemorrhage centered in parimesencephalic cisterns [1,2]. The incidence of parimesencephalic hemorrhage has increased recently; however, the management of parimesencephalic hemorrhage is still unstandardized [3], particularly where or not a conventional angiogram is necessary to make a diagnosis. The present case report demonstrated that high-resolution CTA is an acceptable diagnostic tool for patients with suspected parimesencephalic hemorrhage.
CASE PRESENTATION
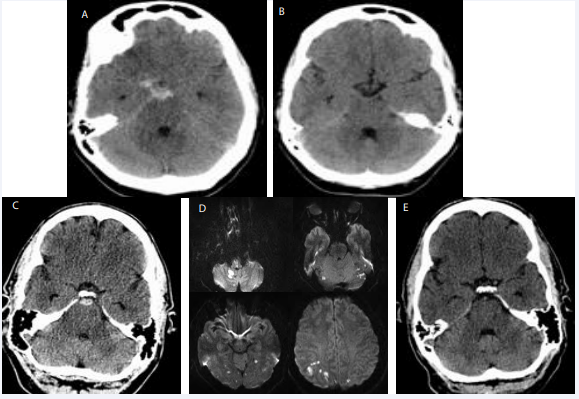
A 48-year-old female presented to the emergency department with sudden onset of “the worst headache of her life”. Headache was aggravated by head movement. She has no other relevant past medical history. Neurological examination was normal. A non-contrast head computed tomography (CT) revealed hemorrhagia within components of the foramen magnum to the suprasellar cistern with suspicion of a parimesencephalic hemorrhage (Panel A). CT angiography of the head showed no evidence of intracranial aneurysm. A repeated head CT two weeks later revealed that the previous prepontine cistern hemorrhage had resolved and was no longer visualized (Panel B). Another patient, a 45-year-old male with controlled type-II diabetes and hypertension, presented to the hospital with a sudden onset severe headache. Neurological examination was normal without focal deficits upon hospital admission. A non-contrast head CT revealed a small hemorrhage within the cisterns anterior to the pons and midbrain (Panel C). CT angiography (image not shown) showed normal flow in the anterior and posterior circulation without evidence of cerebral aneurysm. Subsequently, a conventional angiography was obtained to rule out possible occult posterior aneurysm, which further demonstrated no evidence of cerebral aneurysm or hemodynamic stenosis. Unfortunately, he developed sudden onset symptoms of mild left hemiparesis, left hemiparesthesia, ataxia, vertigo, and an unsteady gait. Brain magnetic resonance imaging (MRI, Panel D) was then pursued, which revealed multiple foci of restricted diffusion signals involving the brainstem, cerebellar, frontal, parietal, occipital, and temporal regions bilaterally. A repeated head CT two weeks later (Panel E) showed that the previous perimesencephalic hemorrhage had resolved. These embolic ischemic infarcts are iatrogenic secondary to conventional angiography.
DISCUSSION
Perimesencephalic hemorrhage rarely results from a ruptured cerebral aneurysm [4], which carries a benign course that distinguishes these patients from ruptured aneurysmal or traumatic subarachnoid hemorrhage (SAH). Detection of cerebral aneurysm with CT angiography is highly accurate, with a sensitivity and specificity of 100% [5]. Conventional angiography can be withheld, which could avoid potential periprocedural embolic events, especially in patients with underlying vascular risk factors, such as our second case.
STATEMENT OF ETHICS
Written informed consents were obtained from patients for publication of the details of their medical cases and any accompanying imaging. Ethical approval is not required for this study in accordance with local guideline.
Figure 1 A, Initial noncontrast head CT revealed perimesencephalic hemorrhage in a patient who is a 48-year-old female. B, Noncontrast head CT demonstrated resolved hemorrhage on day 14 in the same patient. C, Head CT showed small hemorrhage within prepontine cistern in a different patient who is a 45-year-old male. D, Brain MRI diffused weighted imaging showed multiple embolic infarcts after conventional angiogram. E, A repeated head CT after 2 weeks demonstrated resolved prior prepontine cistern hemorrhage as displayed in Panel C.
AUTHOR CONTRIBUTIONS
Dr. Beenish Javaid conceptualized and designed the work including data acquisition and drafting oof the manuscript. Dr. Asad Ahrar took part in the drafting of the manuscript. Dr. Jiangyong Min helped designing the work and took part in manuscript reversion. All authors reviewed and edited the manuscript, approved the final version, and took full responsibility for the data, the analyses, and the interpretation.
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
REFERENCES
- van Gijn J. Subarachnoid hemorrhage. Lancet.1992; 339: 653–5.
- van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: Diagnosis, causes, and management. Brain. 2001; 124: 249–78.
- Wolfert C, Maurer CJ, Sommer B, Steininger K, Bonk MN, Krauss P, et al. Management of perimesencephalic nonaneurysmal subarachnoid hemorrhage: a national survey. Sci Rep. 2023; 13: 12805.
- Mensing LA, Vergouwen MDI, Laban KG, Ruigrok YM, Velthuis BK, Algra A, et al. Perimesencephalic Hemorrhage: A Review of Epidemiology, Risk Factors, Presumed cause, clinical course, and outcome. Stroke. 2018; 49: 1363-1370.
- Velthuis BK, Rinkel JE, Ramos LM, Witkamp TD, Van Leeuwen MS. perimesencephalic hemorrhage exclusion of vertebrobasilar aneurysms with CT angiography. Stroke. 1999; 30: 1103-9.