Two Rare Variations; Persistent Trigeminal Artery and Hypoplasia of the A1 Segment of the Anterior Cerebral Artery
- 1. Clinic of Radiology, Nevsehir State Hospital, Nevsehir, Turkey
- 2. Department of Radiology, Duzce University, Turkey
Abstract
The trigeminal artery, which is one of the major carotid-basilar anastomoses in the fetal period, regresses with the development of the posterior circulation in the prenatal period. In rare cases, when this regression does not occur but persists, it is called persistent trigeminal artery (PTA). Because of the association of the persistent trigeminal artery with many other cerebral vascular pathologies, it is of vital importance to identify it and know its imaging characteristics, especially in cases where vascular surgery or interventional procedures are planned. We report a case with PTA and hypoplasia of the A1 segment of the anterior cerebral artery (ACA) as an associated vascular anomaly. Magnetic resonance angiography (MRA) is a non-invasive method for the detection of PTA and other vascular anomalies.
Keywords
• Persistent trigeminal artery
• Magnetic resonance imaging
• Magnetic resonance angiography
• Anterior cerebral artery hypoplasia
• Cerebral vascular variations
Citation
Has B, Naldemir IF, Guclu D, Onbas O (2024) Two Rare Variations; Persistent Trigeminal Artery and Hypoplasia of the A1 Segment of the Anterior Cerebral Artery. J Neurol Disord Stroke 11(1): 1213.
ABBREVIATIONS
ACA: Anterior Cerebral Artery; AComA: Anterior Communicating Artery; ICA: Internal Carotid Artery; MIP: Maximum Intensity Projection; MR: Magnetic Resonance; MRI: Magnetic Resonance Imaging; MRA: Magnetic Resonance Angiography; PComA: Posterior Communicating Artery; PTA: Persistent Trigeminal Artery; TSE: Turbo Spin Echo
INTRODUCTION
Anastomoses between the carotid and vertebrobasilar systems in the fetal period may persist into adulthood, although the cause is unknown. PTA is the most common type of these persistent anastomoses (~85%). Its prevalence has been reported as 0.06-0.6% [1,2]. The majority of cases are detected incidentally by imaging or post-mortem examination. PTA usually arises from the petrous or cavernous internal carotid artery (ICA), follows a posterolateral course and joins the basilar artery [1,3,4]
In this case report, we aim to show the MRA findings of PTA with ACA-A1 segment hypoplasia and address the significance of cerebral vascular anomalies.
CASE PRESENTATION
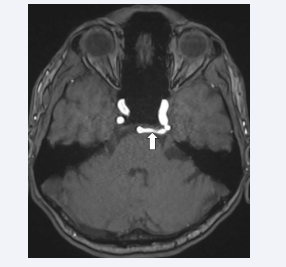
A 45-year-old man was admitted to our hospital with complaints of headache, dizziness and occasional nausea which started one month ago. There was no neurological deficit. A cranial MR scan was performed using a 3.0T magnetic resonance (MR) scanner (MAGNETOM Sykra, Siemens Healthineers, Erlangen, Germany, 2017) and no intra-axial pathology was found. However, an aberrant vascular structure originating from the basilar artery was observed in the left part of the prepontine cistern (Figure A) and cerebral MRA (3D TOF MRA) was planned.
Figure A: T2-weighted TSE sequence in the axial plane on the cranial MRI. A vascular structure between the ICA and basilar artery in the left part of the prepontine cistern (arrow)
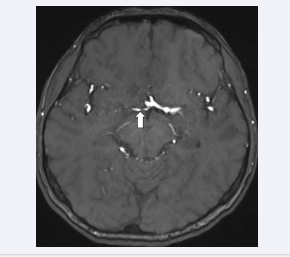
TOF MRA showed a persistent trigeminal artery that formed an anastomosis between the basilar artery and the left ICA (Figure B).
Figure B: TOF MRA. PTA forming anastomosis between ICA and basilar artery (arrow)
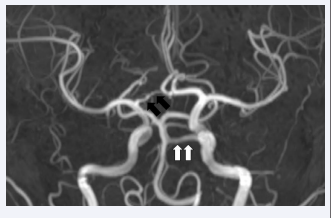
In addition, the A1 segment of the right ACA was hypoplastic (Figure C).
Figure C: TOF MRA. Right-sided hypoplastic A1 segment of the ACA (arrow)
Both vascular variations were visible on 3D MIP images (Figure D).
Figure D: TOF MRA with 3D MIP images. PTA (white arrows) and hypoplastic A1 segment of the ACA (black arrows).
DISCUSSION
The trigeminal artery is one of the arteries that forms a carotid-basilar anastomosis in the in-utero period and is one of the longest persistent arteries throughout the embryonic period. As the posterior fossa grows and the posterior communicating artery develops, it often regresses [1,5]. It is called PTA if it does not regress and persists into adulthood. The reason why primitive arteries such as the trigeminal artery persist and remain patent in adulthood is not clear [1].
Saltzman classified PTA into two main groups by showing the cerebral angiography findings of 8 patients with PTA. Later, type 3 was defined as a combination of types 1 and 2 [2,4,6]. In Saltzman type 1, PTA joins the basilar artery extending between the superior cerebellar artery (SCA) and antero-inferior cerebellar artery, and the posterior circulation distal to the anastomosis is supplied by the PTA. The proximal basilar or vertebral artery may be hypoplastic or aplastic and the posterior communicating artery (PComA) may be absent. In Saltzman type 2, PTA supplies mainly the SCAs, the proximal basilar artery is well developed and the PComA is present [1,2,4].
In an anatomical study performed on cadavers, Salas et al. classified the PTA into two classes as lateral (petrosal) and medial (sphenoidal) according to its relationship with the sella turcica. In the lateral type, which is more common, the PTA courses lateral to the dorsum sella. The medial type penetrates the dorsum sella, compresses the pituitary gland and is therefore important in transsphenoidal surgeries [1,4,5,7,8].
The classic appearance of PTA on the MR images is described as tau sign. This sign describes the appearance of the PTA in the form of the letter ‘t’ on the sagittal images of MRI or MRA [3].
In addition to many cerebrovascular anomalies associated with PTA, other vascular pathologies such as carotid-cavernous fistula, Moyamoya disease, cerebral aneurysm, arteriovenous malformation, and large vessel occlusion have been reported. In the management and treatment of these vascular pathologies, knowledge of the anatomical significance and imaging findings of PTA is important [1,4]. Demonstrating PTA is important to avoid potential complications before transsphenoidal surgery, neurovascular surgery or interventional procedures [1,3].
ACAs are located in the anterior circulation of the brain, are terminal branches of the ICA and are connected by the anterior communicating artery (AComA). Like other intracranial vessels, many variations can be seen in the course of ACA. These variations include fenestration, trifurcation, bihemispheric ACA, and azygos ACA. In the A1 segment of the ACA, also known as the horizontal or precommunicating segment, variations such as hypoplasia and aplasia can be observed [8,9]. It has been reported that unilateral A1 segment hypoplasia/aplasia may be associated with AComA aneurysm [9-11]. Recognition of these variations is important in patients undergoing vascular intervention. In addition, it should be kept in mind that collateral flow contribution may decrease and infarct risk may increase in case of ischaemia [8].
In our case, we detected Saltzman type 2 PTA and unilateral hypoplasia of the A1 segment of the ACA as another associated vascular anomaly. There was no evidence of AComA aneurysm in association with the hypoplastic A1 segment.
CONCLUSION
It is important to identify vascular anomalies such as PTA, especially in patients undergoing surgical or endovascular procedures, to prevent potential complications. Patients undergoing pituitary surgery in particular are at high risk of bleeding, which can be life-threatening due to vascular injury. Furthermore, the identification of ACA variations plays an important role in preventing complications during surgical or endovascular interventions in this region, where aneurysms are most commonly observed. MRA stands out as an applicable, safe and non-invasive diagnostic method for the diagnosis of cerebral vascular anomalies.