A Fatal Case of Myasthenia Gravis Exacerbation in Covid-19 Leading to Acute Respiratory Failure
- 1. Department of Internal Medicine, Franciscan Healthcare, USA
- 2. Department of Internal Medicine, Gandhi medical college and hospital, India
- 3. Department of Health equity and Inclusion, Thomas Jefferson University, USA
- 4. Department of family medicine, Siddhartha hospital, India
Abstract
Background: The neurologic potential of COVID-19 in auto-immune disorders is yet to be uncovered. With chronic immunosuppression, patients with Myasthenia gravis are vulnerable in contracting the SARS-CoV-2 virus that may lead to further complications during the course of the disease along with progression towards pneumonia leading to increased mortality.
Case Report: We report a case of a 33-year-old male with a history of Myasthenia gravis who experienced COVID-19 infection leading to exacerbation of Myasthenia gravis symptoms and succumbed to death due to acute respiratory failure.
Conclusion: The implications of COVID-19 in auto-immune diseases like Myasthenia Gravis is very complex, with immunosuppressive therapy putting the patients at higher risk of contracting SARS-CoV-2 virus complicating to acute interstitial pneumonia and leading to Respiratory failure. About 15% of Myasthenia gravis (MG), patients are particularly susceptible to infections leading to Myasthenic crisis and evolution of respiratory muscle weakness leading to restrictive respiratory failure due to the combination of reduced neuromuscular safety factors adversely affected by pyrexia and the effect of acute inflammatory mediators compounded by immunosuppression. Viral infections are reported to stimulate autoimmunity through augmentation of T-cell signalling leading to cytokine dysregulation, causing Acute Respiratory Distress Syndrome.
Keywords
- Covid-19
- Immunocompromised state
- Myasthenia Gravis
- Thymectomy
- Acute Respiratory Distress Syndrome
- Respiratory failure
Citation
Adhikari R, Suram VK, Deepika K, Joseph T (2020) A Fatal Case of Myasthenia Gravis Exacerbation in Covid-19 Leading to Acute Respiratory Failure. J Neurol Transl Neurosci 6(1): 1087
INTRODUCTION
The rapid outbreak of coronavirus disease (COVID-19), caused by SARS-CoV-2 virus continues to be a global pandemic with increasing fatalities on a daily basis. The symptoms of COVID-19 are contingent on the age and the patient’s underlying medical illness and also the condition of the immune system [1]. Patients with auto-immune disorders have been more probable to have severe complications after contracting the SARS-CoV-2 virus than the general population [2]. Myasthenia Gravis (MG) is a postsynaptic auto-immune disease and is the most common disorder of the neuromuscular junction. About 15% of the patients can encounter Myasthenic crisis during the course of the disease and infections contribute towards one-third of the cases of the exacerbation of Myasthenic symptoms [3]. Immunocompromised states due to treatment can also put patients suffering from MG at a higher risk of contracting SARS-CoV-2 virus [4]. Here we present a case of a 33-year-old male patient with a history of MG who experienced infection with COVID-19, leading to exacerbation of symptoms and succumbed to death due to acute respiratory failure.
CASE REPORT
Myasthenia Gravis and COVID-19 Infection
The patient is a 33-year-old male with a history of Acetylcholine receptor antibody (AChR-Ab) positive MG. His exacerbations typically consisted of the weakness of lower extremities after activity and ptosis, and he occasionally experienced dysphagia. The patient was maintained on prednisone and underwent Thymectomy for the remission of symptoms. The patient presented to the emergency Department with a two day history of fever, cough, chills, and diffuse myalgia. He reported difficulty in breathing during the past day. The patient was given a surgical mask, and contact precautions were commenced. In the emergency Department the patient’s temperature was 38.3. Breath sounds were diminished in intensity bilaterally. The patient was transferred to the Intensive care unit (ICU) and symptomatic treatment was initiated. Initial chest X-ray revealed bilateral infiltrates with non-homogenous opacities consistent with Atypical consolidation suggestive of viral pneumonia. The COVID-19 test was reported positive on the second day of admission. Complete blood count revealed neutrophilia and lymphopenia, which is consistent with viral pneumonia. The respiratory status deteriorated on the third day of admission with severe hypoxemia and hypotension. The patient also developed Acute Respiratory Distress syndrome concomitantly developed metabolic acidosis with hyponatremia. Arterial blood gas levels disclosed partial pressure of oxygen as 40.1% and oxygen saturation at 72.8%, and the patient started to deteriorate. Rapid sequence intubation was initiated in the ICU for mechanical ventilation. The condition deteriorated rapidly despite emergency procedures, and the patient expired on the fourth day of admission due to hypoxemic respiratory failure secondary to SARS-CoV-2 infection.
DISCUSSION-MYASTHENIA GRAVIS AND COVID-19 INFECTION
The neurologic complications of COVID-19 are still being uncovered as the disease pursues to spread with increasing rates of mortality. Table 1
|
Table 1: Case Summary. |
|
|
Gender |
Male |
|
Age |
33 |
|
Diagnosis Of Myasthenia Gravis |
Positive |
|
Antibody Status |
Achr+ |
|
History Of Thymectomy |
Positive |
|
Immunosuppressive Regimen |
Maintained On Prednisone |
|
Presenting Symptoms |
Fever, Cough, Chills, Diffuse Myalgia |
|
Covid-19 |
Positive |
|
Treatment Of Mg During Covid-19 |
Maintenance Doses |
|
Required Respiratory Support |
Yes-Intubated |
|
Myasthenic Exacerbation/Crisis |
Yes- Ards With Respiratory Failure |
|
Status |
Crisis Leading To Death |
describes the case summary of the patient along with the Medical history of MG and Thymectomy. MG is a chronic auto-immune disease of the neuromuscular junction (NMJ) caused by antibodies that attack components of the postsynaptic membrane, impair neuromuscular transmission that leads to weakness and fatigue of the skeletal muscle [5]. The pathogenesis of MG can be attributed to (Ig)G1 and (Ig) G3 antibodies to the acetylcholine receptor (AChR), producing complement-mediated damage leading to loss of AChR receptors [6]. Patients usually present with fluctuating and fatigable skeletal muscle weakness. The weakness of facial muscles, oro-pharyngeal muscles are the major factors contributing to morbidity in MG, which include slurred speech, drooping of eyelids, dysphagia and sometimes can lead to aspiration [7]. In MG, the involvement of respiratory muscles can be life-threatening [8]. Corticosteroids being the mainstay in the treatment of MG do have potential adverse effects during the course of treatment as observed in this particular patient who was maintained on prednisone [9]. In patients with moderate to severe symptoms, IV high-dose steroids are recommended for rapid remission and are gradually tapered to a minimal effective dose [10]. The immunosuppressive effect of corticosteroids is a known significant adverse effect that may pose a significant risk of infections with viral, bacterial and fungal pathogens in direct proportion to the dose and duration of therapy with corticosteroids [9]. In some cases of MG, elective Thymectomy is recommended for the control of myasthenic symptoms which also puts the patients at a higher risk of contracting infections [11]. Immunocompromised patients are at an increased risk of contracting respiratory viruses which may lead to further complications during the course of the disease along with progression towards pneumonia leading to increased mortality [12]. Increased duration of harbouring the pathogens is also associated with increased morbidity. This also explains the vulnerability of this patient in contracting the SARS-CoV-2 virus.
The implications of COVID-19 in auto-immune diseases like MG is very complex, with immunosuppressive therapy putting the patients at higher risk of contracting SARS-CoV-2 virus and complicating towards acute interstitial pneumonia and leading to Acute Respiratory distress syndrome. About 15% of MG patients are particularly susceptible to infections leading to Myasthenic crisis and evolution of respiratory muscle weakness leading to restrictive respiratory failure due to the combination of reduced neuromuscular safety factors adversely affected by pyrexia and the effect of acute inflammatory mediators compounded by immunosuppression in many patients [13]. The distinctive observation, in this case, is MG exacerbation. It is very well known that infections can cause Myasthenic crisis by unmasking the existing MG symptoms. Viral infections are reported to stimulate autoimmunity through augmentation of T-cell signalling leading to a pro-inflammatory environment due to a hyper-active antiviral immune response with effects of temperature at the neuromuscular junction [14]. The magnitude of increase in neutrophil counts suggests the intensity of inflammatory response in this patient with COVID-19 whereas the decrease in Lymphocyte count indicates the extent of impairment of immune system in response to COVID-19 infection [19]. The immunopathogenesis of COVID-19 and Myasthenic crisis can also be due to cytokine dysregulation, which causes an increase in pro-inflammatory cytokines and chemokines leading to ARDS [15]. The arterial blood gas values and oximetry values reveal significant lung injury in this patient due to an overaggressive and dysregulated pro-inflammatory cytokine response in SARS-CoV-2 virus infection termed as ‘cytokine storm’ [16]. It is also possible that dysregulated inflammatory response causing cytokine storm can lead to metabolic acidosis, which explains the increased concentration of clac in this patient [17]. This phenomenon of a dysregulated immune response in metabolic acidosis has also been described in patients with severe sepsis [18]. In this specific case, the Cytokine storm resulting in myasthenic crisis resulted in deleterious inflammation and poor clinical outcome. This patient, combined with several risk factors, was potentially associated with a worse outcome in COVID-19 with MG. Though the disease course was aggressively managed, the patient succumbed to Acute Respiratory distress syndrome leading to respiratory failure and death (Table 2 and Figure 1).
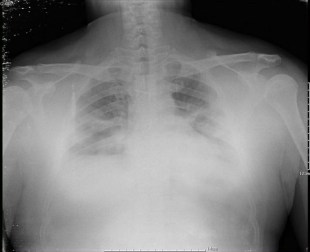
Figure 1 Bilateral interstitial patchy infiltrates suggestive of viral pneumonia.
|
Table 2: Laboratory Values. |
|
|
? |
7.420 ( 7.350 - 7.450 ) |
|
pCO2 |
41.5mmHg ( 32 - 45 ) |
|
pO2 |
40.1mmHg ( 83.0 - 108 ) |
|
ctHb |
15.6 g/dL ( 12.0 - 16.0 ) |
|
Hctc |
47.9% ( 36.0 - 52.0 ) |
|
sO2 |
72.8% ( 95.0 - 99.0 ) |
|
cLac |
71mg/dL ( 5 -10) |
|
cGlu |
292mg/dL ( 65 - 95) |
|
WBC |
20.96 |
|
Neutrophils |
19.50 |
|
Lymphocytes |
0.44 |
|
cNa+ |
134mmol/L ( 136 - 146 ) |
CONCLUSION
Evaluating patients with neuromuscular disorders for potential neuromuscular complications of COVID-19 poses a greater challenge ahead. Risk of treatments is to be considered while treating COVID-19 with MG. Patients with neuromuscular disorders may need stress doses of steroids which may also lead to further complications. Abrupt cessation of medications can flare up the underlying condition. As infection has always been the leading cause of exacerbation of MG symptoms, attention should always be given to baseline respiratory dysfunction.
In this pandemic of novel coronavirus - COVID-19, MG patients should be considered as high risk due to immunosuppression and respiratory muscle weakness. Also understanding how to identify patients presenting with COVID-19 with underlying auto-immune comorbidities like MG going on to develop severe crises is of paramount importance [20]. Monitoring underlying disorder and risks associated with it is the most important predictor of clinical outcome during this pandemic. Alteration in corticosteroid and catecholamine response to acute stressors like the severe viral infection is speculated in the development of exacerbation of MG. Treatments should be tailored based on individual patients and the severity of COVID-19, which helps in preventing fatal complications from the disease [20]. The MG expert panel suggests that therapy decisions should be individualized and made collaboratively between the person with MG and his/her healthcare provider [4]. Therefore, it is vital to recognize MG as a potential risk factor for COVID-19 complications and patients need to take extra precautions as advised by the Centers for Disease Control and prevention to protect themselves from contracting COVID-19.








































































































































