Intercostal Neuralgia: A Review
- 1. Department of Pain Management, Delhi Pain Management Centre, India
Abstract
Intercostal neuralgia is pain in the thoracic region emanating from an intercostal nerve. It occurs commonly after thoracotomy. It can also be seen in elderly debilitated patients without a known precipitating event, other causes include rib trauma, very rarely benign periosteal lipoma and pregnancy. Intercostal neuralgia due to surgical injury of the intercostal nerve has traditionally been difficult to treat. No single treatment modality has been curative. There are several treatment options available, including systemic medications, topical or invasive nerve blocks, cryoablation, and radio ablation. Despite numerous treatment advances, many patients remain refractory to the current therapies and continue to have pain, physical and psychological distress. In this review, we will discuss the pathophysiology of intercostal neuralgia, its clinical manifestations, diagnosis and various pharmacological, non-pharmacological and interventional treatment modalities, as also the insight into the potential complications of the disease and treatment modalities.
Keywords
• Neuropathic pain
• Intercostal neuralgia
• Treatment
• Intercostal nerve block
Citation
Dureja GP (2017) Intercostal Neuralgia: A Review. J Neurol Transl Neurosci 5(1): 1076
INTRODUCTION
Intercostal neuralgia refers to a neuropathic condition involving the intercostal nerves, manifesting as intense dysesthetic pain, e.g., sharp, shooting, or burning in quality.
The pain is constant and burning in nature and May involve any of the intercostal nerves and the sub costal nerve of the12th rib. The pain usually begins at the posterior axillary line and radiates anteriorly into the distribution of the affected intercostal and sub costal nerves. Deep inspiration or movement of the chest wall may increase the pain of intercostal neuralgia slightly but much less compared with the pain
Associated with the musculoskeletal causes of chestwall pain (e.g., costosternal joint pain, Tietze’s syndrome, or broken ribs) [1,2].
Intercostal Neuralgia occurs due to a number of reasons such as nerve entrapment, a traumatic or iatrogenic neuroma, persistent nerve irritation, or herpes zoster [1]. The pain of intercostal neuralgia is the result of damage or inflammation of the intercostal nerves and can be localized one or more of the intercostal space. Although it is most commonly seen and recognized in patients with chronic chest wall pain after thoracotomy [3-5], intercostal neuralgia has been reported in patients after breast and abdominal surgery, trauma, and infection [6-8]. Intercostal neuralgia due to surgical injury of the intercostal nerve has traditionally been difficult to treat. No single treatment modality has been curative [5,6]. There are several treatment options available, including systemic medications [1,5], topical or invasive nerve blocks [5,9,10], cryoablation[11-13], and radiofrequency ablation [14].
PATHOPHYSIOLOGY OF INTERCOSTAL NEURALGIA
Anatomy of Intercostal Nerves
The twelve pairs of thoracic spinal nerves (T1-12) are divided into ventral and dorsal rami after they pass through the inter vertebral for amina. The ventral rami of T1- T11formtheintercostal nerves that enter the inter costal spaces. The ventral ramus of T12 forms the subcostalnerve that is located inferior to the 12th rib. The dorsal rami of T1-T12 pass posteriorly to supply sensation to skin, muscles, and bones of the back [15].
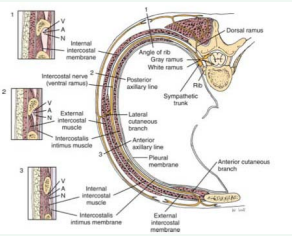
Intercostal nerves are composed of dorsal horn sensory afferent fibers, ventral horn motor efferent fibers, and postganglionic sympathetic nerves. The major branches of intercostal nerves are anterior and lateral cutaneous branches (Figure 1).
 \
\
Figure 1 Intercostal nerve location. The inter costal nerve (N) runs along the inferior rib with the artery (A) and vein (V)
These branches divide and innervate the skin and intercostal muscles of an individual segment along with variable collateralinnervation of the adjacent segments. Throughout its course, each inter costal nerve is associated with an artery and a vein. The intercostal nerve travels inferior to the vein and artery of the same segment [16].
The pathogenesis of acute intercostal neuralgia involves multiple etiologies, such as skin and muscle injury, costochondral dislocation, costovertebral ligament damage, post herpetic neuralgia, post thoracotomy pain, orintercostalneuritis. The pathophysiology of acute pain involves chemo sensitive ion channels in peripheral nociceptors that are activated by cytokines released from damaged tissue or inflammatory cells. Activation of these channels results in generation of action potentials that are conducted from the peripheral nociceptors in the chest area to the thoracic spinal cord via intercostal nerves.
The pathophysiology of chronic intercostal neuralgia pain is complex and involves a combination of peripheral, central, and psychological mechanisms. In some patients, a structural or inflammatory source can be identified; however, most patients encountered in clinical practice have primary pain disorders in which the etiologies are uncertain [16].
Epidemiology
According to University Pain Centre Maastricht thoracic pain is relatively rare, and is only seen in an estimated3-22% of patients referred to pain clinics. The prevalence of thoracic pain in the general population is about 15%. Chronic post-thoracotomy and post-thoracoscopy pain has a prevalenceof40%, and half of these cases are neuropathic in character. Intercostal neuralgia is the most frequent form.
The exact prevalence of abdominal wall pain is unknown. Abdominal wall pain has been diagnosed in 10 to 90 percent of patients with abdominal pain of unknown cause in various series based upon the patient cohort [17]. In one study, 5 to 10 percent of patients referred to specialist practices in gastroenterology had a diagnosis of chronic abdominal wall pain. In another study, 20 percent of patients admitted to a surgical department for abdominal pain had abdominal wall pain [18].
Women appear to be four times more likely to have chronic abdominal wall pain than men. The peak incidence is between the ages of 30 to 50 years, although cases have been reported in children and the elderly.
Clinical Manifestations
The first symptom of intercostal neuralgia may be considered pain in the ribs, which is due to irritation or compression of the intercostal nerves. According to the nature of the pain it can be different in feeling: burning, sharp, aching, or dull. According to the periodicity the pain can be both episodic and constant. The pain can be dramatically intensified if any, even minor physical activity, or simply an unexpected movement, for example, a sharp body movement, jump, cough or sneeze.
The symptoms of intercostal neuralgia can be recognized with a simple probing. During the palpation of the certain parts of the body (in the area between ribs along the spinal discs and thorax), the patient can feel a sharp pain. Also, patients often complain about the pain during the active inhalation and exhalation, there is a feeling of “intercepting” breathing. There is also a “reflection” of pain, which is usually localized in other parts of the body and can occur under the shoulder blade, in the back and loins. Also the “belting” pain is a characteristic. Intercostal neuralgia may be accompanied by not only the pain and tightness of the intercostal space, but also involuntary contraction and twitching of individual muscle groups. In the area of peripheral nerve injury the skin can change colour (turn red or pale), as well in these places the sensitivity can be lost due to numbness.
In intercostal neuralgia, there are no constitutional signs, such as fever, dyspnea, diaphoresis, or shortness of breath [19]. Physical examination generally reveals minimal findings unless the patient has a history of previous thoracic or sub costal surgery or cutaneous evidence of herpes zoster involving the thoracic dermatomes. Patient with intercostal neuralgia do not attempt to splint or protect the affected area, unlike patients with musculoskeletal causes of chest wall and sub costal pain. Careful sensory examination of the affected dermatomes may reveal decreased sensation or all odynia. When motor involvement of the sub costal nerve is significant, the patient may complain that his or her abdomen bulges outward [20].
Diagnosis
Physical Examination: Extensive general physical and neurological examinations are always indicated in thoracic pain, particularly when dorsal column disorders are present. The sensitivity of the thorax and stomach should also be examined. Loss of sensitivity indicates whether or not the pain is neuropathic pain. Examination of the thoracic spine is preferably performed with the patient in a sitting position and comprises inspection at rest and palpation of the vertebra and para vertebral structures, such as the costovertebral joints.
Provocation of pain by performing passive rotations, forward flexion, backward flexion and lateral flexions in particular, can indicate that the pain has as pinalaetiology. In upper thoracic and median and paramedian unilateral pain, shoulder function on the same side should also be examined. Pressure pain in the sternum, sternocostal and cost overtebral junctions is usually accompanied by a local pain pattern(e.g., Tietzesyndrome), but is sometimes associated with segmental pain. Pressure pain of the rib(s) can indicate which thoracic level(s) is involved. Segmental translation of the thoracic vertebra (Federung test) in the prone position can indicate the level of the affected segment.
Additional Somatic Diagnostics: Since thoracic pain is not a clinical entity and the cause cannot always be determined by anamnesis and physical examination, additional diagnostics are always necessary.
- In uncomplicated intercostal neuralgia, additional diagnostics are not necessary
- In trauma with or without osteoporosis, X-ray is indicated in order to exclude an impression fracture.
- When there is suspicion of a malignancy, MRIs can and/ or referral to a specialist is mandatory. Particularly in patients with a history of malignancy with acute thoracic pain, additional diagnostics are important. The same is true in the case of neurological deficits.
- When there is suspicion of pathology in the chestwall and/or there are pulmonary
- Complaints, X-ray can be useful, together with possible referral to a pulmonary specialist.
- When there is any doubt, or if visceral pathology is suspected, ultrasound, CT scan or
- Referral to a specialist should be considered.
Differential diagnosis [19]:
Thoracic radiculopathy
Malignant neoplasm (primary or metastatic)
Rib fracture
Vertebral compression fracture
Chest wall contusion
Acute Herpes Zoster and Postherpetic neuralgia
Referred pain from cardiac, pulmonary, vascular, or GI systems
Angina, Myocardial infarction
Aortic dissection
- Esophageal disorders
- Cholecystitis
- Peptic ulcer disease
- Pancreatitis
- Pleurisy
- Pulmonary embolism
- Pneumothorax
- Costochondritis
- Tietze syndrome
- Nephrolithiasis
- Pyelonephritis
- Costovertebral or costochondral arthritis
- Spondylitis
Multidisciplinary Treatment
A definite treatment protocol is yet to be suggested for patients of intercostal neuralgia, as the efficacy of the proposed treatments is difficult to evaluate. Small sample sizes, difficulty in assigning control groups, and ambiguous outcome parameters are the main factors that affect the outcome. The initial choice of therapy should be guided by the patient’s comorbidities, adverse effects of drugs, and patient preference. Whether or not somatic treatment is indicated is based on the pain diagnosis. Based on the findings of the pain questionnaires, additional diagnostics and/or multidisciplinary treatment comprising various non-somatic treatments may be necessary (Figure 2).

Figure 2 Treatment plan for Intercostal neuralgia.
Somatic Treatment
Pharmacological Treatment: Tricyclic anti depressants: Amitriptyline, Nortryptyline, Desipramine
Anticonvulsants: carbamazepine, oxcarbazepine, gabapentin, pregabalin
Non-somatic Treatment:
Psychological Treatment
Cognitive-Behavioural Treatment
Rehabilitation Treatment
Interventional Pain Treatment
Intercostal Nerve block
Dorsal root ganglion test block
Dorsal root ganglion PRF treatment
Pharmacological Treatment (Table 1)
Table 1: Treatment of options for Intercostal Neuralgia/
|
Table 1: Treatment of options for Intercostal Neuralgia/ |
||
|
Medications |
Dosage |
Adverse effects |
|
Antiepileptics |
||
|
Gabapentin |
100 to 300 mg orally at bedside; increase dosage by 100 to 300 mg every 2 days until dosage is 300 to 800 mg three times daily or response is adequate |
Mild peripheral edema, cognitive impairment, somnolence, fatigue, dizziness, ataxia, rash |
|
Pregabalin |
50mg at bedtime daily, increase to 150 mg bd daily within one week |
Sleep disturbance, dizziness |
|
Tricylic antidepressants
Amitriptyline
Nortriptyline
Imipramine
Desipramine
|
10 to 25mg orally at bedtime; increase dosage by 25mg every two or four weeks until response is adequate, or to a maximal dosage of 150mg per day |
Sedation, dry mouth, consipation, sweating xerostomia, confusion, dysrhythmias, weight, gain, dizziness |
|
Topical agents
Capsaicin cream 0.025%
Capsaicin cream 0.075%
Capsaicin cream 8%
|
Applied to affected area three to five times daily
single- application placed on the skin for 60 minutes after pretreatment with lidocaine cream;
Up to four patches may be applied at one time, and repeated as often as every three months
|
Localized erythema and comfortable burning, stinning or itching |
|
5% Lidocaine gel |
Apply to affected area every four to twelve hours, as needed |
Localized skin irritation |
|
Transdermal 5% lidociane |
One -to – three patches worn for 12 hour interval |
|
|
Eutectic mixture of local anesthetics ( 2.5% of lignocaine 2.5% prilociane) |
Apply to affected area every six to twelve hours as needed |
|
Typically, drugs have not been specifically tested on populations of patients with intercostal neuralgia. Instead, physicians are left to extrapolate the data from treatment of other sources of neuropathic pain and to apply those principles in choosing medication to be used for this population. Often, neuropathic pain responds poorly to acetaminophen, non-steroidal anti-inflammatory drugs, and low-dose narcotics, in contrast to nociceptive pain [21, 22]. However, if the pain is mild to moderate, these agents are often tried first. Topical agents may be effective when there is significant allodynia or dysesthesia. Capsaicin creams are available over-the-counter, and a newer capsaicin patch (Qutenza) is available by prescription (the actual indication is for postherpetic neuralgia). Capsaicin is derived from hot chilli peppers from the genus Capsicum and has a long history of use in medical practice. It interacts with sensory afferents via vanilloid receptors VR1, which are cation channels from transient receptor potential family. Chronic exposure to capsaicin stimulates and desensitizes these channels. Besides, capsaicin depletes substance P at nervous afferent endings and transiently decreases the density of nervous fibers on the skin. Capsaicin is available as 0.025% cream used 3-4 times/day or 8% patch for single dose [23]. Topical lidocaine applied as a gel, eutectic mixture of local anesthetics (EMLA), or patch (Lidoderm) is another alternative [9]. It was recognized that a lidocaine patch acted only on abnormal, intact hyperalgesic afferent receptors. Recently, patches proved to be effective also in skin devoid of nociceptors [24]. Topical lidocaine slows peripheral nociceptor sensitization and central hyper excitability.
Tricyclicantide pressants (e.g., amitriptyline, nortryptyline, desipramine) have been used for neuropathic pain for decades [25]. Unfortunately, this class of drugs is associated with significant anticholinergic side effects, including dry mouth, constipation, sedation, and urinary retention.
These drugs should be used with caution in patients suffering from glaucoma, cardiac arrhythmia, and prostatism. To minimize side effects and encouragecompliance, the physician should startamitriptylineornortryptylineata10-mg dose at bedtime; the dose can then be titrated upward to 25 mg at bedtime, as side effects allow. Subsequently, upward titration in 25- mg increments can be carried out each week, as side effects allow. Even at lower doses, patients generally report a rapid improvement in sleep disturbance and begin to experience some pain reliefin10to14days. The selectiveserotoninre up take inhibitors such as fluoxetine have also been used to treat the pain of intercostal neuralgia, although these drugs are better tolerated but appear to be less efficacious than the tricyclic antidepressants [2]. If the anti depressant compounds are in effective or contraindicated, gabapentin is a reasonable alternative. Gabapentin is started at a 300-mg dose at bedtime for 2 nights. The patient should be cautioned about potential side effects, including dizziness, sedation, confusion, and rash. The drugisthenincreasedin300-mgincrementsgiven in equally divided doses over 2 days, as side effects allow, until
Painrelief is obtained or a total dose of2400mg/day is reached. At this point, if the patient has experienced partial pain relief, blood values are measured, and the drug is carefully titrated upward using 100-mg tablets. Rarely is a dose greater than 3600 mg/day required [2]. Pregabalin can also be started at a low 50 mg bedtime dose and titrated to 300 mg twice daily, although it is uncommon to exceed 150 mg twice daily. Gabapentin and other anti convulsants should be tapered before discontinuance [19]. Like gabapentin and pregabalin, to piramate has also been used off - label for intercostal neuralgia [1].
Narcotics are often required for intercostalneuralgia. Adequate analgesia is needed to promote continued activity levels and to prevent deconditioning from disuse. Initial treatment should be with short-acting agents such as hydrocodone 5 mg with acetaminophen 325 mg every 4 hours as needed.
Treatment of inter costal neuralgia can be protracted, and patients are often switched to long-acting agents for maintenance. If the pain is progressive, one should reevaluate the diagnosis and reconsider the possibility of occult tumor. In refractory cases of neuropathic pain, clonidine, an adrenergic agonist, and ketamine, an N - methyl- d -aspartate (NMDA) receptor antagonist, may be prescribed by pain specialists [26].
REHABILITATION
Physical and occupational therapy can be instrumental in combating disusede conditioning.Also, desensitization techniques may be employed. Psychological consultation, relaxation therapy and acupuncture have also been employed with anecdotal success [4].
If pain is severe, intercostal neuralgia may lead to avoidance of activity and deconditioning. It is important to keep patients physically active early in the habilitation process. The muscles of persons on strict bed rest lose 1.0%to1.5% of their strength per day during a 2-weekperiod. The loss is greatest during the first week of inactivity. The local application of heat and cold or the use of anelasticrib belt may also provide symptomatic relief.
Biofeedback uses instrumentation to provide feedback on a variety of physiologic responses, such as muscle tension.Itisty picallyusedtofacilitaterelaxationandtoenhanceself-regulation. Two common relaxation therapies are autogenic training and progressive muscle relaxation [19].
INTERVENTIONAL MANAGEMENT
Local infiltration of a neuroma with corticosteroids and local anesthetics, intercostal nerve blocks, in dwelling epidural catheters, and spinal nerve injections have all been used to control the pain associated with intercostal neuralgia when adequate relief is not achieved with oral and topical medications [27]. If symptoms are well controlled with intercostalnerveblocksbut recur, neurolytic injection of phenol or alcohol has been used to denervate the peripheral nerve [28]. Indwelling epidural catheters have been used to provide regional anesthesia with minimal drug use. This technique was found to be safe and effective in pregnantpatientswho developed intercostal neuralgias [29].
In Intercostal nerve block the patient is placed in the prone position with the arms hanging loosely off the sides of the table. Alternatively, this block can be done in the sitting or lateral position. The Rib to be blocked is identified by palpating its path at the posterior axillary line. The index and middle fingers are then placed on the rib, thus bracketing the site of needle insertion, and the skin is prepared with antiseptic solution (Figure 3).
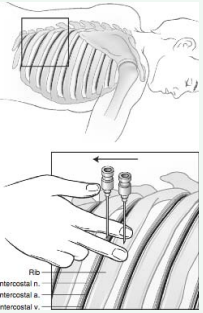
Figure 3 Intercostal nerve Block.
A11⁄2- inch, 22-gaugeneedleis attachedtoa12-mLsyringe and is advanced perpendicular to the skin while aiming for the middle of the rib between the operator’s index and middle fingers. The needle should impinge on bone after being advanced approximately 3⁄4 inch. Once bony contact is made, the needle is with drawn into the sub cutaneous tissues, and the skin and subcutaneous tissues are retracted with the operator’ spalpating fingers inferiorly. This technique allows the needle to be walked off the inferior margin of the rib. As soon as bony contact is lost, the needle is slowly advanced approximately2mmdeeper. This maneuver places the needle in proximity to the costalgroove, which contains the inter costal nerve as well as the inter costal artery and vein (Figure 4).
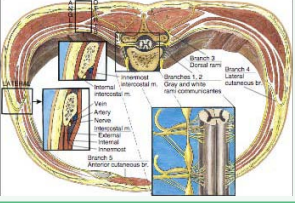
Figure 4 Intercostal nerve block: Cross-sectional anatomy.
After carefull aspiration reveals noblood or air, the operator injects 3to5mL of 1%preservative-free lidocaine. If the pain has an inflammatory component, the local anesthetic is combined with 80 mg methyl prednisolone and injected in incremental doses. Subsequent daily nerve blocks are carried out in a similar manner, substituting 40mg methylprednisolone for the initial 80- mg dose. Because of the overlapping innervation of the chest and upper abdominal wall, the intercostal nerves above and below the nerve suspected of causing the pain must also be blocked [20].
The standard of care for interventional pain management has shifted towards procedures performed under fluoroscopicguidance for accuracy and safety. For procedures not conducive to fluoroscopic guidance, nerve stimulation and ultrasound guidance may be used for accuracy and safety. Ultrasound guidance can greatly facilitate intercostal nerve blockade and improve patient comfort as ultrasound guidance offers a distinct advantage over the traditional anatomic landmark based approach. The landmark-based approach is performed at the posterior axillary line where the ribs can be easily palpated. This is often lateral, however, to the division of the intercostal nerve into deep and lateral cutaneous branches and may therefore result in good anesthesia of the rib and thoracic musculature but poor anesthesia of the parietal pleura. With direct visualization of the ribs and pleura, ultrasound guidance allows the provider to perform an intercostal block medial to the scapula where the intercostal nerve can be blocked before its division, ensuring adequate anesthesia of the pleura. In addition, routine use of ultrasound guidance enables visualization of local anesthetic injection into the intercostal space, allowing the provider to adjust the needle trajectory and depth as needed to ensure adequate anesthetic spread [30].
Thoracic Para vertebral Nerve Block is useful for the management of pain in the upper abdominal wall, the chest wall, and the thoracic spine. It is used to control acute pain in conditions such as rib fractures, acute herpes zoster of the thoracic cage, and cancer pain. The block is performed with the patient in the prone position. The spinous process of the vertebra above the nerve to be blocked is identified (Figure 5).
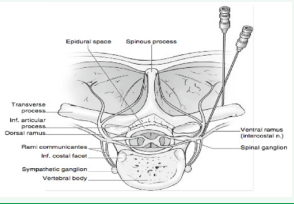
Figure 5 Thoracic paravertebral nerve block.
A 3.5-in. needle is used for the block and is inserted after appropriate antiseptic treatment of the skin immediately below and 1.5 in. lateral to the spinous process. The transverse process should be encountered at a depth approximately 1.5 in. at which point the needle is walked off the inferior aspect of the transverse process and inserted another 0.75 in. deeper until a paresthesia is obtained. After negative aspiration for blood or CSF a total of 5 cc of 1% preservative-free lidocaine solution is injected for pain relief. If there is an inflammatory component then 40 mg of methyl prednisolone can be added for the initial block [31].
Recently, the implementation of pulsed radiofrequency (RF) has generated intense interest in the medical community as a safe and potentially effective treatment for neuropathic pain. In Thoracic Nerve Radiofrequency Lesioning the junction of the posterior axillary line and the rib to be blocked is identified. A 22-gauge 54-mm radiofrequency needle usually equipped with a 4 mm active tip is advanced aiming for the middle of the rib. After encountering the bone the needle is walked off the inferior border of the rib and advanced about 2 mm deeper to be close to the costal groove. First a trial sensory stimulation with 2 V at 50 Hz is performed to ensure that there is a paraesthesia along the distribution of the intercostal nerve to be lesioned. A pulsed radiofrequency lesion is then performed by heating at 40-45?for 5 min or alternatively by heating at 49-60?for 90s [31]. In one of the studies it was concluded that Pulsed RF of the dorsal root ganglia was a superior treatment to pharmacotherapy and pulsed RF of the intercostal nerves in patients with chronic post surgical thoracic pain [32]. Cryotherapy involves another way of interrupting the peripheral nerve’s ability to transmit pain by freezing it. Cryotherapy has been used on neuromas and the involved intercostal nerve [33].
Spinal cord stimulators have been implanted for inter costal neuralgia but with less success than in neuropathic pain due to diabetic peripheral neuropathy and causal gia [34]. Botulinum toxin type A (BTX-A) has been widely used in many clinical disorders including migraine, cervical dystonia, etc. The use of BTX-A in neuropathic pain, however, is uncommon, and the application of the anti-nociceptive effect of botulinum toxin is emerging. The effectiveness of BTX-A in treating neuropathic pain implies a direct action on sensory neurons and possibly with an indirect central action [35].
POTENTIAL COMPLICATIONS OF INTERVENTIONS
The most prevalent complication of interventional treatment is post-procedural pain. Local pain occurs for a few days after almost all procedures. Twenty percent of the patients who received RF treatment reported that the post-procedural pain lasted for a few weeks [36]. The major complications of an intercostal nerve block are pneumothorax and intravascular injection of local anesthetics. Careful post-procedure monitoring is necessary to detect these complications. The incidence of clinical significant pneumothorax has been reported less than 0.1% [37,38]. Accidental intravascular injection of local anesthetics during intercostal block is uncommon but potentially serious. It is known that blood levels of local anesthetics after aninter costalnerve Block are significantly greater than those after other frequently performed regional anesthetic techniques [39]. Adding epinephrine to local anesthetics and aspirating for blood before administering anesthetics, as well as injection of nonionic contrast under continuous fluoroscopy, are important steps that can be taken to minimize intravascular injection of local anesthetics. Other rare complications associated with an intercostal nerve block include infection, hemothorax, hemoptysis, hematoma, tissue necrosis, neuritis, respiratory insufficiency,
Sub arachnoid block, failed block, and allergic reaction to local anesthetics [40]. If nonionic contrast is used, anaphylactoid reaction scan occur, but are rare, and can be avoided by a pretreatment regimen of prednisone, diphenhydramine, and ranitidine [41].
SURGERY
Surgical resection of a neuroma can be effective but should be reserved for cases that have failed more conservative care and have demonstrated a temporary response to intercostal blocks. Dorsal root entry zone ablation involves surgical destruction of nociceptive secondary neurons in the spinal cord when pain is not adequately controlled with medical therapy[42,43]. The technique involves laminectomy with intradural exposure of the spinal cord. With an operating microscope, a radiofrequency probe is used to heat the dorsal horn of the affected side with a series of lesions
POTENTIAL DISEASE COMPLICATIONS
Untreated upper intercostal neuralgia can potentially lead to a frozen shoulder as patients limit their use of the arm in response to the pain. Intercostal neuralgia can also cause a chronic pain syndrome with its comorbidities. Psychosocial dysfunction associated with chronic neuropathic pain includes impaired sleep, decreased appetite, and diminished libido [19].
CONCLUSION
Intercostal neuralgia is a commonly encountered cause of chest wall and thoracic pain. Correct diagnosis is necessary to treat this painful condition properly and to avoid overlooking serious intra thoracicor intra abdominal disease. Pharmacologic agents generally provide adequate pain control. If necessary, intercostal nerve block is a simple technique that can produce dramatic pain relief, but the proximity of the intercostal nerve to the pleural space makes careful attention to technique mandatory.
Transcutaneous electrical nerve stimulation (TENS) is an option for the treatment of thoracic radicular pain. Results for this specific treatment are not known. Two publications report good results from RF treatment in thoracic radicular pain management. Stolker et al. evaluated 45 patients with thoracic radicular pain [41]. There was a significant reduction of pain in more than 70% of the patients 13 to 46 months after the treatment. A similar study was conducted by van Kleef and Spaans [44]. They found that 52% of the patients had significant pain reduction for 9 to 39 months. PRF of the DRG resulted in a higher percentage of success, and the duration of the pain relief was longer (5 months vs. 3 months). The effect of classic RF treatment is better and lasts longer, but it damages the ganglion spinale (DRG). In cases of chronic thoracic radicular pain, an intercostal block can be performed as part of the diagnostic blocks. In case of therapy resistant pain, RF treatment or PRF treatment of the ganglion spinale can be considered [36].
REFERENCES
5. Karmakar MK, Ho AM. Postthoracotomy pain syndrome. Thorac Surg Clin. 2004; 14: 345-352.
15. MooreKL, AgurAMR. Essentia lClinical Anatomy. Philadelphia: Lippincott Williams &Wilkins; 2006.
20. Waldman SD. Atlas of Common Pain Syndromes Saunders. 3rd edn. 2011; 197-199.
26. MilchRA. Neuropathicpain: implications for the surgeon. Surg Clin North Am. 2005; 85:1-10.
29. SaxTW, Rosenbaum RB. Neuromuscular disorders in pregnancy. Muscle Nerve. 2006; 34: 559-571.








































































































































