Do Attended Sessions Support the Effect of Tailored Goal Oriented Community Brief Intervention Model (TGCBI) Among Risky Drinkers in Community, Thailand
- 1. College of Public Health Sciences, Chulalongkorn University, Thailand
ABSTRACT
Tailored Goal Oriented Community Brief Intervention Model (TGCBI) is the first adapted alcohol intervention for risky drinkers in a Thai community. The TGCBI has 2 levels (the public and individual levels). The TGCBI trial was to compare two high-risk drinking prevalence communities in Lop Buri Province between the TGCBI (a community in Phatthana Nikhom District) and control (a community in Chai Badan District) groups. The samples were recruited from those in both sites aged 19-65 whose AUDIT scores identified them as risky drinkers. The TGCBI consisted of 4 sessions over two months.
The effectiveness of TGCBI compared to controls has been presented. Hence, the numbers of TGCBI sessions that the risky drinkers attended are assessed.
Outcome measures included number of non-drinking days at 1, 3 and 6 month follow up. ANOVA was used to measure the outcomes. Results showed that the number of non-drinking days in previous month were not significantly different between sites at baseline. However, there were significant differences at all three follow up points with the treatment group having significantly more non-drinking days. The number of TGCBI sessions attended was positively correlated with the number of non-drinking days.
KEYWORDS
• Sessions attended
• TGCBI
• Community
• Risky alcohol consumption
• Thailand
CITATION
Areesantichai C, Perngparn U (2014) Do Attended Sessions Support the Effect of Tailored Goal Oriented Community Brief Intervention Model (Tgcbi) Among Risky Drinkers in Community, Thailand. J Subst Abuse Alcohol 2(2): 1011.
ABBREVIATIONS
TGCBI: Tailored Goal Oriented Community Brief Intervention Model; BI: Brief Intervention; AUDIT: Alcohol Use Disorders Identification Test
INTRODUCTION
Thailand was ranked 40th of the world in terms of its per capita alcohol consumption [1]. The 2007 Thai national household survey reported the average population nationwide prevalence of substance abuse and lifetime alcohol consumption, along with past 12 months and 30 days consumption. The data indicated that 13.23 million (28.4%) consumed alcohol during the past year, and 10.54 million (22.7%) consumed in the past 30 days. The data indicated that some 2.8 million were hazardous drinkers and 0.39 million harmful drinkers (3.1%) and about 0.23 million (1.9%) alcohol dependent [2].
The survey in Lop Buri province found that Chai Badan and Phatthana Nikhom districts had the highest prevalence of alcohol consumption 30 days prior to the interview at 15.73% and 12.52% respectively. The most popular alcohol beverages were white spirit, Thai liquor, beer, local liquor and Chinese liquor respectively [3].
WHO has indicated that Brief Intervention (BI) takes a short time with a simple process, and is a cost-effective intervention for alcohol related problems [4,5]. Brief interventions can be effective in reducing alcohol consumption among moderate drinkers in a middle income country such as Thailand [6-9].
As far as we are aware, there is no community intervention which is adapted into two levels i.e. community/public level and individual level in Thailand. This TGCBI is the first intervention model of its kind that has been associated with reduced alcohol consumption among the risky drinkers in a community. In prior reports of this study, we indicated the results of AUDIT scores [10], average daily consumption and frequency of drinking [11], the sustainability in term of the number of abstinent drinkers and number of alcohol free month [12].
This article aims to assess the association between the number of non-drinking days and session attendance of TGCBI at the whole follow up.
MATERIALS AND METHODS
Briefly, (the detailed method was reported in the previous reports [10-12]) this study interviewed the participants aged 19-65 years who have lived in the household for more than 6 months in two high risk drinking prevalence communities (the intervention group: Phatthana Nikhom District and the control group: Chai Badan District) in Lop Buri Province. The distance between two communities is about 100 kilometers, sufficient distance to reduce intervention contamination across sites.
Ethical approval was provided by the Health Sciences Review committee, Chulalongkorn University.
All members in both intervention and control groups were interviewed at the same time period by two trained teams. Also, these teams were not the same as the interventionists.
The AUDIT scores were reported the positive scores (8-19 scores) as 78 risky drinkers (intervention group) and 74 risky drinkers (control group). This study reports only on participants who completed the all three follow ups (1, 3 and 6 months). This results in 47 and 50 participants in the intervention and control groups respectively.
TAILORED GOAL ORIENTED COMMUNITY MODEL BRIEF INTERVENTION (TGCBI)
Briefly, TGCBI consists of 2 levels (a community/public level and an individual level). In the community focus, we engaged cooperation and support from key stakeholders (e.g. the abbot, community doctor and village leader). The researchers and the key informants provided the whole community with information about alcohol use and associated risks and encouraged them to become more aware of their own drinking behavior. The detailed approach is discussed in previous reports [10-12].
The individually focused TGCBI is a brief intervention approach based on FRAMES [4,5]. However, for implementation in Thai communities we added the following tailored community and cultural context for the participants:
We required the participants to assess their drinking level. This step (Feedback) aims to lead their awareness for drinking effect and lead their responsibility for the next step.
We encouraged the participants to concern their problems which are related to drinking. In this step (Responsibility), the participants explored their drinking behavior and consequences and were encouraged to develop commitment to engage in the TGCBI and change their drinking behavior.
We provided specific, tailored advice which was related to their current problems and strategies to change.
We encouraged participants to set their own goal to reduce or stop drinking by using their own menu of options. The participants could engage family member and peer participation or even the support of the village leader and monk depending on their personal situation and needs.
We developed a meaningful and reliable therapeutic relationship to communicate empathy and to build a commitment to engage with the TGCBI. The participants felt empathy as they needed to join the TGCBI sessions.
The last step, self-efficacy to change, was developed through therapeutic and family/community support during the initial intervention at 1, 2 weeks and 1 month.
MEASUREMENT OF INSTRUMENTS
Study instruments assessed demographic characteristics, alcohol consumption, AUDIT (0.92 for sensitivity and 0.94 for specificity [13]) and the timeline follow-back instrument (TLFB) as a valid and reliable method of quantifying alcohol use patterns during follow up [14]. The instruments were translated into Thai and back-translated into English to ensure their accuracy in translation. Moreover, we established validity and test-retest reliability in Thai community context (Kappa .852).
Analysis
ANOVA was used to analyze outcome in terms of number of non-drinking days and sessions attended for the whole 6 month follow up, and total number of alcohol free months at the whole follow up period with the participants who completed follow-ups at 1, 3 and 6 months in the intervention and control groups. SPSS version 16.0 was used for analyses.
RESULTS
We described the baseline of risky drinkers who completed all follow-ups in intervention (47 cases) and control groups (50 cases) in previous reports, as the intervention and control groups were similar in term of demographic characteristics and alcohol consumption [10-12].
We divided the TGCBI attended sessions into 3 groups i.e. attended 4 sessions, 3 sessions and 1-2 sessions. The results indicated that most participants in the intervention group (74.5%) attended 4 sessions while 17% attended 3 sessions. In Table 1, the results showed no significant of intervention and control groups at baseline. However, the results showed significant differences at all follow-ups.
Table 1: The number of TGCBI sessions and the number of non drinking day at whole 6-month follow-up among risky drinkers in two high prevalence communities.
| SS | MS | F | Sig. | ||
| The number of non-drinking days at baseline | Between Groups | 381.939 | 127.313 | 1.165 | .327 |
| Within Groups | 10162.226 | 109.271 | |||
| The number of non-drinking days at 1 month follow-up | Between Groups | 763.679 | 254.560 | 2.689 | .050 |
| Within Groups | 8805.001 | 94.677 | |||
| The number of non-drinking days at 3 month follow-up | Between Groups | 877.009 | 292.336 | 3.524 | .018 |
| Within Groups | 7715.898 | 82.967 | |||
| The number of non-drinking days at 6 month follow-up | Between Groups | 1618.499 | 539.500 | 5.967 | .001 |
| Within Groups | 8408.841 | 90.418 |
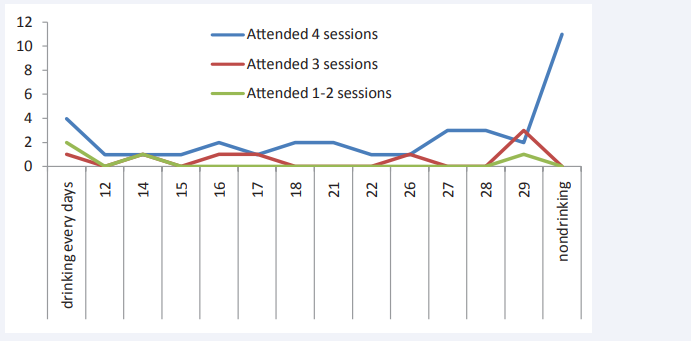
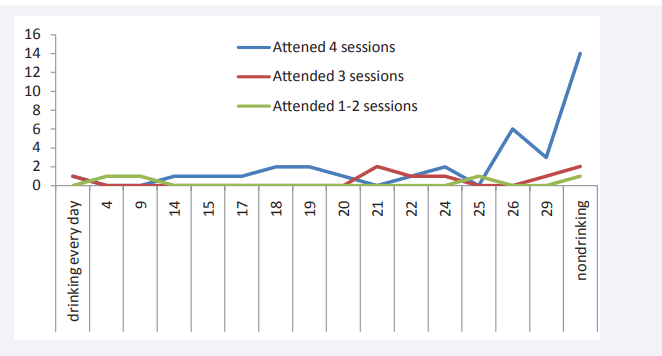
In Figure 1-3, the graphs between the number of drinking days and the number of TGCBI attended sessions illustrate that the participants who attended more sessions of TGCBI were more likely to stop drinking alcohol than the participants who attended less sessions.
Figure 1: The number of drinking days and the number of TGCBI attended at 1 month follow-up.
Figure 2: The number of driniking days and the number of TGCBI attended at 3 month follow-up.
Figure 3: The number of drinking days and the number of TGCBI attended at 6 month follow-up.
DISCUSSION
The TGCBI is the first trial of a community based brief intervention in Thailand. The inclusion of community factors (e.g. involvement of community leaders etc) is a unique feature of the Thai TGCBI. Effectiveness of TGCBI has been presented in previous reports [10-12]. The current report indicates a dose-response relationship: participants who attended 4 sessions of TGCBI had better outcome in terms of non-drinking days than those who attended fewer sessions and the control group.
The outcomes related to the sustainability of TGCBI in the intervention community, in terms of total number of alcohol free months after intervention at the whole follow up period, were 36% and 24% in the intervention and control groups respectively [12]. In addition, this study corresponded with other reports which have confirmed the efficacy of brief interventions in reducing risky levels of alcohol consumption in non-dependent individuals [6-8,15-18]. However, there are some unique features of this Thai trial.
A key limitation of the study was that it relied on self-report and there was no objective confirmatory analysis undertaken (e.g. laboratory analysis of drinking such as through blood or breath alcohol analysis). The modest sample size and trial in just two communities limits generalizability.
CONCLUSION
The overall results indicated that the participants who attended more sessions of TGCBI are more likely to stop drinking over a 6 month follow up compared to participants who attended fewer than 4 sessions and those in control group.
ACKNOWLEDGMENT
We are very much grateful to Associate Professor Vichai Poshyachinda, M.D., who gave us the knowledge and experiences regarding the substance research. We are thankful to Professor Chitr Sitti-amorn, M.D., Ph.D., who helped us regarding the consultation, comments and guidance. Our special thanks go to Professor Steve Allsop, the Director of the National Drug Research Institute (NDRI), Curtin University, Perth, Australia for his kind support, helpful guidance and consultation. We would like to thank the participants, staffs, key informants i.e. the abbot, Director of Phatthana Nikhom Community Hospital, Dr. Nopporn Pongpleumpitichai and health personnel for their kind supports and assistance of TGCBI research.