A Novel Scalp Coronal Incision Approach for Esthetic Repair of Complex Craniomaxillofacial Fractures: A Case Report
- 1. Department of Stomatology, People’s Hospital of Ningxia Hui Autonomous Region, Ningxia Medical University, China
- 2. Ningxia Medical University, China
- 3. Department of Oral and Maxillofacial Surgery, General Hospital of Ningxia Medical University, China
Abstract
The scalp coronal incision treats complex craniomaxillofacial fractures as it hides incisions/scars behind the hairline. But traditional incisions extend to the non-hairy tragus front to expose fractures, causing visible scars. Anatomical variations can lead to complications like facial nerve injury and temporal hollowing. We modified the approach, moving the incision from the tragus front to the postauricular (hairy) area. Our method had esthetic benefits with no facial scars. Using the supratemporalis route, we fully exposed fractures, avoided nerve injury, reduced temporal hollowing risk, and achieved good results.
Keywords
• Craniomaxillofacial
• Fractures
• Scalp Coronal Incision Approach
• Prognosis
• Esthetic Repair
Citation
Xue J, Cao K, Yang J, Mao J, Zhou Z (2025) A Novel Scalp Coronal Incision Approach for Esthetic Repair of Complex Craniomaxillofacial Fractures: A Case Report. Ann Otolaryngol Rhinol 12(3): 1359.
INTRODUCTION
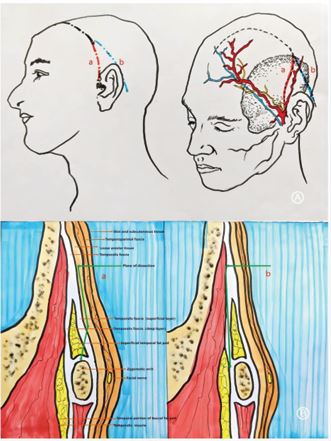
The scalp coronal incision fully exposes the cranial vault and upper two - thirds of the facial skeleton, hiding incisions and scars behind the hairline. Thus, it’s widely used for complex craniomaxillofacial fractures. However, the traditional coronal incision often extends to the hairless area in front of the tragus, causing visible scars and being less acceptable. Moreover, it has a high complication risk, including facial nerve injury, temporal hollowing, infection, and haemorrhage [1,2]. Hence, several modified approaches have been proposed [3-5].In this study, we used a modified scalp coronal incision via the postauricular and supratemporalis routes to treat upper - two - thirds facial fractures (Figure 1). We report on one patient who had successful postoperative recovery, satisfactory aesthetics, and no facial nerve injury or temporal hollowing.
Figure 1: Comparison between traditional coronal incision approach and novel scalp coronal incision approach. (1a) The traditional coronal incision approach. (1b) The novel scalp coronal incision approach.
SURGICAL TECHNIQUE
Preoperatively, patient informed consent and ethical approval from Ningxia Med Univ Gen Hosp were obtained. Patient had nasal tracheal intubation for general anesthesia. Incision started at postauricular mastoid, within hairline at external auditory canal level, extended upward behind hairline, turned in temporal region to behind frontal hairline, ending at forehead midline. Incision (2–4 cm from hairline) paralleled hair follicles. Skin, subcutaneous tissue, superficial fascia, and sub-galea connective tissue were incised sequentially. Deep temporal fascia was opened 5-6 cm above zygomatic arch, keeping fat pad intact. Fat pad was separated from temporalis and flipped with skin flap. Periosteum along deep zygomatic surface was dissected to expose fractures, followed by open reduction and internal fixation. Post-surgery, temporal fascia, galea, and skin were sutured.
CASE PRESENTATION
A 39-year-old woman presented to our hospital’s emergency department with multi-site pain due to trauma 2 days prior. Physical examination revealed facial asymmetry with left zygomatic depression. Bilateral temporomandibular joint mobility was normal; there was no pre-tragal tenderness, but marked tenderness at the zygomatic arch root. The left orbital soft tissues were swollen, ecchymotic, and tender. The left eyeball was congested, with a mouth opening of one and a half fingers. Maxillary CT showed multiple fractures in the left orbital medial/lateral walls, left maxillary sinus walls, and left zygomatic arch, indicating clear surgical indications. After preoperative examinations, our department used the modified coronal incision for open reduction and internal fixation. At the 2-week follow-up, the surgical area had healed well, free of facial nerve injury or temporal depression. Three months post-surgery, the patient was satisfied with her appearance.
DISCUSSION
In the modified postauricular approach, the incision lies behind the hairline. It fully exposes key craniofacial structures, including the orbits, zygomatic complex, temporomandibular joint, and upper maxilla, making it suitable for complex craniomaxillofacial fracture repair [6,7]. The flexibility of the upper auricular cartilage allows adequate rotation of the front flap, eliminating exposure concerns even in patients with wide zygomatic and frontal dimensions4.This approach conceals the incision, delivering good aesthetic results and high patient acceptance, especially among men with receding hairlines and children [8,9]. It also reduces the risk of damaging the superficial temporal vessels and auriculotemporal nerve-issues associated with the preauricular approach. Moreover, it minimizes intraoperative bleeding, offers a clear surgical field, and reduces postoperative complications [5]. Facial nerve injury is a common complication of the scalp coronal incision. Previous research indicates that elevating the superficial fascia and fat pad along the zygomatic arch periosteum is a simple and safe technique [10]. The scalp coronal incision, made 5 - 6 cm above the zygomatic arch via the supratemporalis approach, incises the deep temporal fascia and separates the fat pad from the temporalis muscle. Flipping the fat pad and skin flap together helps avoid facial nerve injury and reduces temporal fat pad damage, lessening temporal resorption.
CONCLUSION
The scalp coronal incision through the modified postauricular approach combined with the supratemporalis route is successfully applied to repair complex maxillofacial fractures at our institution. The overall satisfactory efficacy suggests that future prospective clinical trials with a large sample size should be performed to further evaluate the efficacy and safety of this approach.
ACKNOWLEDGEMENT
The authors thank the patients for their support of the research. This study was supported by the Natural Science Foundation of Ningxia (2021AAC05019), the Key Research and Development Plan of Ningxia Autonomous Region (2023BEG02036).
INFORMED CONSENT
The involved patients have provided written informed consents for the use of their images.
FINANCIAL DISCLOSURE STATEMENT
The authors have no financial interests or conflicts of interest to declare in relation to the content of this article. This study was supported by the Natural Science Foundation of Ningxia (2021AAC05019), the Key Research and Development Plan of Ningxia Autonomous Region (2023BEG02036.)
REFERENCES
- et al Minimizing complications associated with coronal approach by application of various modifications in surgical technique for treating facial trauma: A prospective study. Natl J Maxillofac Surg. 2016; 7: 21-28.
- Lei W, Wenjie Z, Libo S, Hangyu Z, Shuangjiang W, JingangX. Application of modified coronal approach in treatment of craniomaxillofacial fractures. Hua Xi Kou Qiang Yi Xue Za Zhi. 2017; 35: 167-170.
- Luo W, Wang L, Jing W, Zheng X, Long J, Tian W, et al. A new coronal scalp technique to treat craniofacial fracture: the supratemporalis approach. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113: 177-182.
- Polley JW, Cohen M. The retroauricular coronal incision. Scand J Plast Reconstr Surg Hand Surg. 1992; 26: 79-81.
- Liu M, Lv K, Li Z, Yang X. Using a Modified Postauricular Hemicoronal Incision to Manage Unilateral Zygomaticomaxillary Complex Fracture. J Craniofac Surg. 2019; 30: e740-e741.
- Pavri SN, Arnaud E, Renier D, Persing JA. The posterior coronal incision. J Craniofac Surg. 2015; 26: 243-244.
- Fox AJ, Tatum SA. The coronal incision: sinusoidal, sawtooth, andpostauricular techniques. Arch Facial Plast Surg. 2003; 5: 259-262.
- Posnick JC, Goldstein JA, Clokie C. Advantages of the postauricular coronal incision. Ann Plast Surg. 1992; 29: 114-116.
- Yavuzer R, Jackson IT. Coronal incision extending postauricularly. Plast Reconstr Surg. 1999; 103: 1532-1533.
- Babakurban ST, Cakmak O, Kendir S, Elhan A, Quatela VC. Temporal branch of the facial nerve and its relationship to fascial layers. Arch Facial Plast Surg. 2010; 12: 16-23.